Background
Mastocytosis is a disorder characterized by mast cell proliferation and accumulation within various organs, most commonly the skin.
The World Health Organization (WHO) classification of mastocytosis includes the following [1, 2] :
-
Cutaneous mastocytosis - Urticaria pigmentosa, maculopapular cutaneous mastocytosis, diffuse cutaneous mastocytosis, mastocytoma of skin
-
Indolent systemic mastocytosis
-
Systemic mastocytosis with an associated (clonal) hematologic non–mast cell lineage disease
-
Aggressive systemic mastocytosis
-
Mast cell leukemia
-
Mast cell sarcoma
This article focuses on cutaneous mastocytosis (CM). The single World Health Organization (WHO) major criterion is multifocal dense infiltrates of mast cells in bone marrow and/or other extracutaneous organs. One major and 1 minor criterion or 3 minor diagnostic criteria are needed to establish a diagnosis of systemic mastocytosis. Minor criteria include baseline total tryptase level of greater than 20 ng/mL; greater than 25% of the mast cells in bone marrow aspirate smears or tissue biopsy sections having spindle atypical morphology; mast cells in bone marrow, blood, or other lesional tissue expressing CD25 or CD2; or detection of a codon 816 c-kit point mutation in blood, bone marrow, or lesional tissue. [3] Distinct polymorphisms correlate with mastocytosis subtypes. [4, 5]
Types of cutaneous mastocytosis include solitary mastocytoma, diffuse erythrodermic mastocytosis, paucicellular mastocytosis (also termed telangiectasia macularis eruptiva perstans [TMEP]), and urticaria pigmentosa (UP). Urticaria pigmentosa is the most common form and is characterized by oval or round red-brown macules, papules, or plaques ranging in number from a few to thousands (see images below). [6, 7, 8, 9]
Lesions may vesiculate in infancy (see image below).
When a urticaria pigmentosa or mastocytoma lesion is stroked, it typically urticates, becoming pruritic, edematous, and erythematous. This change is referred to as the Darier sign, which is explainable on the basis of mast cell degranulation induced by physical stimulation. Uncontrolled stroking of mastocytomas should be avoided in patients who have had a systemic reaction such as miosis and asthmalike symptoms in their past. [10] The Darier sign usually is not positive in patients with TMEP because the lesions are paucicellular, and, therefore, mast cells may not be present in sufficient numbers for significant degranulation to occur. See the images below.
Also see Systemic Mastocytosis.
Pathophysiology
Mastocytosis is now classified with the myeloproliferative neoplasms. [11] Increased local concentrations of soluble mast cell growth factor in lesions of cutaneous mastocytosis are believed to stimulate mast cell proliferation, melanocyte proliferation, and melanin pigment production. The induction of melanocytes explains the hyperpigmentation that commonly is associated with cutaneous mast cell lesions. The stimulation of pruritus seen in mastocytosis is associated with the production of interleukin (IL)–31. [12] Impaired mast cell apoptosis has been postulated to be involved, as evidenced by up-regulation of the apoptosis-preventing protein BCL-2 demonstrated in patients with mastocytosis. [13] Activating mutations of the proto-oncogene c-kit have been identified but do not explain the initiation of the disease. [14] IL-6 levels have been shown to be elevated and correlated with disease severity, indicating interleukin 6 is involved in the pathophysiology of mastocytosis. [15]
Although pediatric mastocytosis can spontaneously regress, it is a clonal disease most commonly associated with D816V and other activating c-kit mutations. [16]
Research from 2016 has shown that there are varied gene expressions in patients with mastocytosis and associated allergies. Those with associated food allergies have an elevated expression of the TRAF4 gene. [17] In the same study, patients who had an allergy to insect venom had a decreased gene expression of B3GAT1.
Associated systemic manifestations are believed to reflect the release of mast cell–derived mediators, such as histamine, prostaglandins, heparin, neutral proteases, and acid hydrolases. Symptoms and signs induced by mediators may include headache, neuropsychiatric symptoms (cognitive disorganization), flushing, dizziness, tachycardia, hypotension, syncope, anorexia, nausea, vomiting, abdominal pain, and diarrhea. The skeletal, hematopoietic, gastrointestinal (GI), cardiopulmonary, and central nervous systems may be involved either directly, via mast cell infiltration, or indirectly, via mast cell mediator release.
Etiology
Mastocytosis probably is a hyperplastic response to an abnormal stimulus. Rare cases of familial urticaria pigmentosa have been recorded. [18] Rarer cases of cutaneous mastocytosis have been associated with radiotherapy fields in patients with breast cancer. [19]
One case report describes an apparent temporal association between the development of cutaneous mastocytosis and HIV seroconversion, proposing similarities of immunoglobulin E receptors on mast cells and basophils and the association of basophils in HIV pathophysiology. [20]
Autism spectrum disorders may be increased in children with mastocytosis. [21]
Epidemiology
Frequency
Of new patients visiting dermatology clinics, 0.1-0.8% have some form of mastocytosis. Maculopapular cutaneous mastocytosis is the most common subgroup found in children, at approximately 47-75% of cases. There are approximately 17-51% of mastocytoma and 1-5% of diffuse cutaneous mastocytoma in pediatric cases as well. [22]
Race
Most reported cases are in whites. The cutaneous lesions of most types of mastocytosis are less visible in persons with more heavily pigmented skin.
Sex
Mastocytosis affects males and females equally (no known sex predilection).
Age
Most patients with mastocytosis are children; 75% of cases occur during infancy or early childhood and usually resolve by puberty. Mastocytosis incidence peaks again in patients aged 30-49 years.
Prognosis
The prognosis depends on the age of onset. Most patients with urticaria pigmentosa (UP) exhibit onset before age 2 years, which is associated with an excellent prognosis, often with resolution by puberty. The number of lesions diminishes by approximately 10% per year. However, acute extensive degranulation rarely can cause life-threatening episodes of shock.
Increased serum baseline tryptase levels and extensive skin involvement are predictors for the severity of mast cell activation episodes in children with mastocytosis. Serum baseline total tryptase to predict the need for daily antimediator therapy, hospitalization, and episodic management in an ICU were 6.6, 15.5, and 30.8 μg/L, respectively. [23]
Slight improvement of skin symptoms, reflected by decrease of SCORing MAstocytosis Index, with decline in serum tryptase levels is the typical course in patients with diffuse cutaneous mastocytosis. [24] Systemic mastocytosis may occur more frequently in diffuse cutaneous mastocytosis patients. [25] Patients with adult or adolescent-onset urticaria pigmentosa are more likely to have persistent disease and are at greater risk for systemic involvement. Juvenile-onset systemic mastocytosis has a malignant transformation rate as high as 7%, whereas adult-onset systemic mastocytosis has a malignant transformation rate as high as 30%. [26]
Rarely, mast cell leukemia may develop in young adults with persistent maculopapular cutaneous mastocytosis. [27]
Primary cutaneous mast cell sarcoma due to the transformation of a benign solitary mastocytoma in an adult has been reported. [28]
Cutaneous mastocytosis onset after age 10 years portends a poorer prognosis, because late-onset disease tends to be persistent, is associated more often with systemic disease, and carries a higher risk of malignant transformation.
In patients with systemic mastocytosis, regression of urticaria pigmentosa is associated with a decreased frequency and severity of other symptoms. Bone marrow findings do not change with regression of urticaria pigmentosa.
One study shows that anaphylaxis is common in patients with mastocytosis (4.3-5.5% per year disease duration) and appears higher than in the healthy population. In childhood, the risk of anaphylactic episodes has been shown to be limited to those with extensive blistering skin disease, but nonexistent for children with mastocytoma or limited disease. In adults, anaphylactic episodes generally appear to be more severe in patients with extensive systemic disease. [29]
Patient Education
Instruct cutaneous mastocytosis patients about avoiding physical stimuli and substances that trigger the condition. Additionally, educate patients and/or parents about the signs and treatment of anaphylaxis, especially in patients with systemic disease or severe symptoms.
Advise mastocytosis patients with systemic disease or extensive symptoms to wear a medical alert bracelet and carry injectable epinephrine in case of an acute event causing mast cell degranulation and subsequent shock. Adults have been reported with severe anaphylaxis after insect stings, especially hymenoptera stings. [30]
-
Urticaria pigmentosa lesions on the face of a child. Courtesy of Lee H. Grafton, MD.
-
Urticaria pigmentosa lesions on the back of a child. Courtesy of Lee H. Grafton, MD.
-
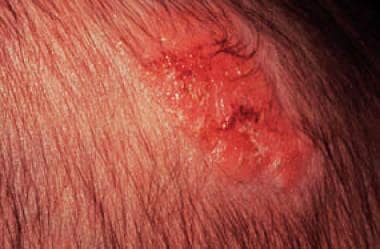
Lesion on the scalp of an infant.
-
Lesion on the arm. Courtesy of Lee H. Grafton, MD.
-
Blistering lesion.
-
Hematoxylin and eosin stain revealing mast cells in the papillary dermis.
-
Giemsa stain revealing mast cells.
-
Positive Darier sign on a child's back.
-
Urticaria pigmentosa on a child.