Practice Essentials
Early pregnancy loss is estimated to occur in 10% of all clinically recognized pregnancies, with about 80% occurring in the first trimester. [1] The term "abortion" is commonly used to mean all forms of early pregnancy loss; however, due to the polarizing social stigma assigned to this term, the term "miscarriage" is used here to indicate all forms of spontaneous early pregnancy loss or potential loss. One of the common complications of pregnancy is spontaneous miscarriage, which occurs in an estimated 5-15% of pregnancies. Spontaneous miscarriages are categorized as threatened, inevitable, incomplete, complete, or missed, and can be further classified as sporadic or recurrent (>3 occurrences). An incomplete miscarriage is shown in the image below.
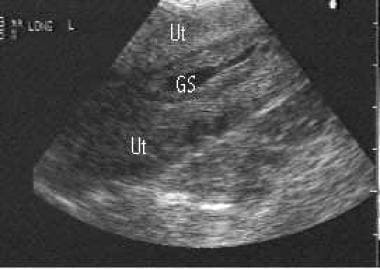 This image shows an endovaginal longitudinal view of a low-lying gestational sac (GS) within the uterus (Ut), representing an incomplete miscarriage.
This image shows an endovaginal longitudinal view of a low-lying gestational sac (GS) within the uterus (Ut), representing an incomplete miscarriage.
Pathophysiology
The pathophysiology of a spontaneous miscarriage may be suggested by its timing. Chromosomal defects are commonly seen in spontaneous miscarriages, especially those that occur during 4-8 weeks' gestation. Genetic etiologies are common in early first-trimester loss but may be seen throughout gestation. Trisomy chromosomes are the most common chromosomal anomaly. Insufficient or excessive hormonal levels usually result in spontaneous miscarriage before 10 weeks' gestation. Infectious, immunologic, and environmental factors are generally seen in first-trimester pregnancy loss. Anatomic factors are usually associated with second-trimester loss. Factor XIII deficiency and a complete or partial deficiency of fibrinogen are associated with recurrent spontaneous miscarriage. [2]
A prospective study by Jayasena et al indicated that in in asymptomatic pregnant women at 6 weeks’ gestation or more, low plasma levels of the hormone kisspeptin are associated with an increased miscarriage risk. [3]
A spontaneous miscarriage is a process that can be divided into 4 stages, as follows: threatened, inevitable, incomplete, and complete.
Threatened miscarriage
Vaginal bleeding, abdominal/pelvic pain of any degree, or both during early pregnancy represents a threatened miscarriage. Approximately a fourth of all pregnant women have some degree of vaginal bleeding during the first 2 trimesters. About half of these cases progress to an actual miscarriage. [4] Bleeding and pain accompanying threatened miscarriage is usually not very intense. Threatened miscarriage rarely presents with severe vaginal bleeding. On vaginal examination, the internal cervical os is closed and no cervical motion tenderness or tissue is found. Diffuse uterine tenderness, adnexal tenderness, or both may be present. Threatened miscarriage is defined by the absence of passing/passed tissue and the presence of a closed internal cervical os. These findings differentiate threatened miscarriage from later stages of a miscarriage.
Inevitable miscarriage
Vaginal bleeding is accompanied by dilatation of the cervical canal. Bleeding is usually more severe than with threatened miscarriage and is often associated with abdominal pain and cramping.
Incomplete miscarriage
Vaginal bleeding may be intense and accompanied by abdominal pain. The cervical os may be open with products of conception being passed, or the internal cervical os may be closed. Ultrasonography is used to reveal whether some products of conception are still present in the uterus.
Complete miscarriage
Patients may present with a history of bleeding, abdominal pain, and tissue passage. By the time the miscarriage is complete, bleeding and pain usually have subsided. Ultrasonography reveals a vacant uterus. Diagnosis may be confirmed by observation of the aborted fetus with the complete placenta, although caution is recommended in making this diagnosis without ultrasonography because it can be difficult to determine if the miscarriage is complete.
Etiology
Causes of first- and second-trimester miscarriage
Embryonic abnormalities
Embryonic abnormalities account for 80-90% of first-trimester miscarriages. Note the following:
-
Chromosomal abnormalities are the most common cause of spontaneous miscarriage. More than 90% of cytogenic and morphologic errors are eliminated through spontaneous miscarriage.
-
Chromosomal abnormalities have been found in more than 75% of fetuses that miscarry in the first trimester.
-
The rate of chromosomal abnormalities increases with age, with a steep increase in women older than 35 years.
-
Trisomy chromosomes commonly are encountered, with trisomy 16 accounting for approximately a third of chromosomal abnormalities in early pregnancy.
Maternal factors
Maternal factors account for the majority of second-trimester miscarriages, with advanced age and a previous early pregnancy loss as the most common risk factors. [1] Chronic maternal health factors include the following:
-
Maternal insulin-dependent diabetes mellitus (IDDM): As many as 30% of pregnancies in women with IDDM result in spontaneous miscarriage, predominantly in patients with poor glucose control in the first trimester.
-
Severe hypertension
-
Renal disease
Acute maternal health factors include the following:
-
Infections (eg, rubella, cytomegalovirus [CMV], and mycoplasmal, ureaplasmal, listerial, toxoplasmal infections)
-
Trauma
Severe emotional shock may also cause first- and second-trimester miscarriages.
Other factors that may contribute to miscarriage
Exogenous factors include the following:
-
Alcohol
-
Tobacco
-
Cocaine and other illicit drugs
Anatomic factors include the following:
Congenital or acquired anatomic factors are reported to occur in 10-15% of women who have recurrent spontaneous miscarriages.
-
Congenital anatomic lesions include müllerian duct anomalies (eg, septate uterus, diethylstilbestrol [DES]-related anomalies). Müllerian duct lesions usually are found in second-trimester pregnancy loss.
-
Anomalies of the uterine artery with compromised endometrial blood flow are congenital.
-
Acquired lesions include intrauterine adhesions (ie, synechiae), leiomyoma, and endometriosis.
-
Other diseases or abnormalities of the reproductive system that may result in miscarriage include congenital or acquired uterine defects, fibroids, cervical incompetence, abnormal placental development, or grand multiparity.
Endocrine factors include the following:
-
Endocrine factors potentially contribute to recurrent miscarriage in 10-20% of cases.
-
Luteal phase insufficiency (ie, abnormal corpus luteum function with insufficient progesterone production) is implicated as the most common endocrine abnormality contributing to spontaneous miscarriage.
-
Hypothyroidism, hypoprolactinemia, poor diabetic control, and polycystic ovarian syndrome are contributive factors in pregnancy loss.
Infectious factors include the following:
-
Presumed infectious etiology may be found in 5% of cases.
-
Bacterial, viral, parasitic, fungal, and zoonotic infections are associated with recurrent spontaneous miscarriage.
Immunologic factors include the following:
-
Immunologic factors may contribute in up to 60% of recurrent spontaneous miscarriages.
-
Both the developing embryo and the trophoblast may be considered immunologically foreign to the maternal immune system.
-
Antiphospholipid antibody syndrome generally is responsible for more second-trimester pregnancy losses than first-trimester losses.
Miscellaneous factors
Miscellaneous factors may account for up to 3% of recurrent spontaneous miscarriages. Other contributing factors implicated in sporadic and recurrent spontaneous abortions include environment, drugs, placental abnormalities, medical illnesses, and male-related causes. Among the risk factors for early pregnancy loss are very low or very high body mass index, a history of previous miscarriages, smoking, alcohol use, working night shifts, air pollution, and exposure to pesticides. [5]
Gestational exposure to nonaspirin NSAIDs may increase the risk for miscarriage. Nakhai-Pour et al identified 4705 women who had spontaneous abortions by 20 weeks' gestation. Each case was matched to 10 control subjects (n=47,050) who did not have a spontaneous abortion. In the women who had a miscarriage, 352 (7.5%) were exposed to a nonaspirin NSAID, whereas NSAID exposure was lower (1213 exposed [2.6%]) in women who did not have a miscarriage. [6]
On the other hand, a study by Daniel et al suggested that for the most part, gestational exposure to nonaspirin NSAIDs does not increase the risk for spontaneous miscarriage. In a study cohort that included 65,457 women who conceived during the study period, a total of 6508 (9.9%) experienced spontaneous miscarriage. Exposure to NSAIDs was not found to be an independent risk factor for miscarriage, with the exception of indomethacin, which, the study indicated, is significantly associated with spontaneous abortion following first-trimester exposure. [7]
Epidemiology
United States statistics
Many pregnancies are not viable. According to estimates, 50% of pregnancies terminate spontaneously before the first missed menstrual period; these miscarriages usually are not clinically recognized. Spontaneous miscarriage is typically defined as a clinically recognized (ie, by blood test, urine test, or ultrasonography) pregnancy loss before 20 weeks' gestation. Approximately 5-15% of diagnosed pregnancies result in spontaneous miscarriage.
International
Some European investigators quote the rate of spontaneous miscarriage to be as low as 2-5%. Chinese researchers concluded that increased parental exposure to phenols is associated with spontaneous abortion. [8]
Race- and age-related demographics
Surveillance data for pregnancy-related deaths demonstrate more deaths due to ectopic pregnancy, spontaneous miscarriage, and induced abortion among African American women than among White women. Eight percent of pregnancy-related deaths among Black women were due to ectopic pregnancies; 7% were due to miscarriages. Among White women, data show that 4% of pregnancy-related deaths were due to ectopic pregnancies; 4% were due to miscarriages. [9, 10]
Age and increased parity affect a woman's risk of miscarriage. In women younger than 20 years, miscarriage occurs in an estimated 12% of pregnancies. In women older than 20 years, miscarriage occurs in an estimated 26% of pregnancies.
Age primarily affects the oocyte. When oocytes from young women are used to create embryos for transfer to older recipients, implantation and pregnancy rates mimic those seen in younger women. The number of miscarriages and chromosomal anomalies decreases, suggesting that the uterus is not responsible for poor outcomes in women of advanced reproductive age.
Prognosis
The prognosis for a successful pregnancy depends upon the etiology of previous spontaneous miscarriages, the age of the patient, and the sonographic appearance of the gestation.
Correction of an endocrine abnormality in women with recurrent miscarriage has the best prognosis for a successful pregnancy (>90%).
In women with an unknown etiology of prior pregnancy loss, the probability of achieving successful pregnancies is 40-80%.
The live-birth rate after documentation of fetal cardiac activity at 5-6 weeks of gestation in women with 2 or more unexplained spontaneous miscarriages is approximately 77%.
When the transvaginal pelvic sonogram shows an embryo of at least 8 weeks estimated gestational age (EGA) and cardiac activity, the miscarriage rate for patients younger than 35 years is 3-5% and for those older than 35 years is 8%.
Unfavorable sonographic prognostic indicators are a fetal cardiac activity rate that is slower than 90 beats per minute, an abnormally shaped or sized gestational sac, and a large subchorionic hemorrhage.
The overall miscarriage rate for patients older than 35 years is 14% and for patients younger than 35 years is 7%.
Mortality/Morbidity
Surveillance data suggest that spontaneous miscarriages and induced abortions accounted for about 4% of pregnancy-related deaths in the United States. [9]
Complications
Potential complications of early pregnancy loss include septic miscarriage and hypovolemic or septic shock.
Preexisting anemia may make patients more susceptible to hypovolemic shock.
Patients with HIV infection who are undergoing curettage may have a higher rate of procedure-related complications but no increase in infectious morbidity.
Coagulation defects may be associated with a retained dead fetus.
Other possible complications include post miscarriage bleeding, retained products of conception, and hematometra.
A prospective survey study by Farren et al found that 28% of women surveyed after early pregnancy loss met the criteria for probably post-traumatic stress disorder at one month and 38% at three months. [11, 12]
Patient Education
Advise patients to return to the ED upon occurrence of symptoms such as the following:
-
Profuse vaginal bleeding (more than 1 pad/hour)
-
Severe pelvic pain
-
Temperature above 38°C (100.4°F)
Patients may experience intermittent menstrual-like flow and cramps during the following week. The next menstrual period usually occurs in 4-5 weeks.
Patients can resume regular activities when able to but should refrain from intercourse and douching for approximately 2 weeks.
For patient education resources, see Pregnancy Center, as well as Bleeding During Pregnancy, Miscarriage, Abortion, and Dilation and Curettage (D&C).
-
This image shows an endovaginal longitudinal view of a low-lying gestational sac (GS) within the uterus (Ut), representing an incomplete miscarriage.
-
This endovaginal longitudinal view demonstrates fluid within the uterus (Ut). Echogenic debris also is present within the endometrial cavity. This image shows a large pseudogestational sac of an ectopic pregnancy.
-
This endovaginal ultrasonographic image demonstrates a subchorionic hemorrhage (SH) less than half the gestational sac size.
-
This flowchart details a diagnostic algorithm based on sonographic findings in early pregnancy, using high-frequency endovaginal sonography (HFEVS) of more than 5 megahertz (MHz). The flowchart incorporates clinical presentation (spotting vs clinical bleeding) with sonographic findings to aid in making clinical decisions. The algorithm continues in Media file 5.
-
This flowchart outlines a diagnostic algorithm based on the initial endovaginal sonographic finding of an intrauterine embryo. The chart incorporates fetal cardiac activity, crown-rump length (CRL), presence of subchorionic hemorrhage (SCH), and uterine or adnexal masses with clinical presentation (spotting vs bleeding) to aid in making clinical decisions.
-
This endovaginal ultrasonogram reveals an irregular gestational sac with an amorphic fetal pole. No fetal cardiac activity was noted. This image represents a missed miscarriage or fetal demise.





