Overview
The shoulder joint, or glenohumeral joint, is a ball-and-socket synovial joint formed by the articulation between the head of the humerus and the glenoid cavity of the scapula. [1] It is the most mobile joint in the body. [2] This mobility provides the upper extremity with tremendous range of motion such as adduction, abduction, flexion, extension, internal rotation, external rotation, and 360° circumduction in the sagittal plane. Furthermore, the shoulder allows for scapular protraction, retraction, elevation, depression, and rotation. This wide range of motion also makes the shoulder joint unstable. [2] This instability is compensated for by the rotator cuff muscles, tendons, ligaments, and glenoid labrum. [3, 4, 5, 6, 7]
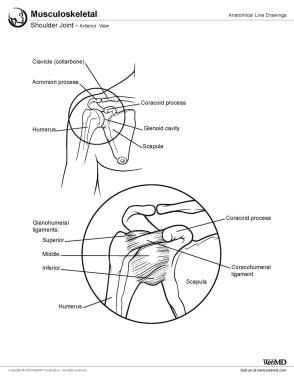
An image depicting shoulder anatomy can be seen below:
Gross Anatomy
The shoulder or pectoral girdle is composed of the bones that connect the upper extremity to the axial skeleton. Two bones comprise the shoulder girdle. These are the clavicle and scapula.
Osteology
Scapula
The scapula, commonly referred to as the shoulder blade, is a flat, triangular bone located on the posterolateral aspect of the thoracic cage. It serves as a critical component of the shoulder girdle, connecting the humerus and clavicle while providing extensive sites for muscle attachment. [1]
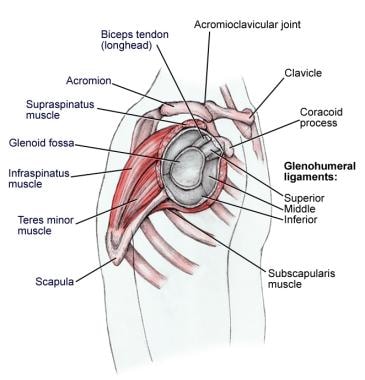
Four rotator cuff muscles that act on the shoulder take their origin from the scapula. These are the S upraspinatus, I nfraspinatus, t eres minor, and S ubscapularis (SItS; see the following image).
Supraspinatus: Originates from the supraspinous fossa, a concave area above the scapular spine, and inserts onto the superior facet of the greater tubercle of the humerus. This muscle is primarily responsible for initiating arm abduction. [1]
Infraspinatus: Arises from the infraspinous fossa, located below the scapular spine, and attaches to the middle facet of the greater tubercle of the humerus. It plays a key role in the external rotation of the arm. [1]
Teres Minor: Originates along the lateral border of the scapula and inserts into the inferior facet of the greater tubercle of the humerus. This muscle assists in the external rotation and adduction of the arm. [1]
Subscapularis: Emerges from the subscapular fossa on the anterior (costal) surface of the scapula and inserts onto the lesser tubercle of the humerus. It is chiefly responsible for the internal rotation of the arm. [1]
Additionally, the trapezius, serratus anterior, rhomboids, and levator scapulae insert on the scapula and are responsible for scapular mobility and stability. The scapula is freely moveable because it is suspended by these muscles. The scapula has four processes: the spine, the acromion, the coracoid, and the glenoid.
Spine: This bony ridge divides the posterior surface into the supraspinous and infraspinous fossae, which serve as origins for the supraspinatus and infraspinatus muscles, respectively. The scapular spine provides attachment to the trapezius and deltoid muscles. [1, 8]
Acromion: Extending laterally from the spine, the acromion articulates with the clavicle at the acromioclavicular (AC) joint and provides attachment for the trapezius and deltoid muscles. [1, 8]
Coracoid process: A hook-like projection on the anterior scapula, it serves as an attachment site for three muscles, the pectoralis minor, coracobrachialis, and short head of the biceps brachii. [1, 8]
Glenoid cavity (fossa): Located on the lateral angle of the scapula, this shallow, oval depression articulates with the head of the humerus to form the glenohumeral (shoulder) joint. The cavity is reinforced by a fibrocartilaginous rim called the glenoid labrum, which deepens its concavity to enhance joint stability. [1, 8]
The glenoid cavity is an irregularly shaped oval and has been compared to an inverted comma shape. It is retroverted by approximately 5-7° relative to the scapular body and tilted superiorly by about 5°. The articular surface is covered with hyaline cartilage, thicker at its periphery than at its center. The superior aspect features the supraglenoid tubercle for attachment of the long head of the biceps brachii tendon, while the inferior aspect includes the infraglenoid tubercle for attachment of the long head of the triceps brachii. [9]
Scapular mobility is essential for upper limb function. Movement of the scapula includes elevation/depression, protraction/retraction, and upward/downward rotation. These motions are facilitated by coordinated muscle activity across several joints, including-the glenohumeral joint, AC joint, and scapulothoracic articulation (a functional joint without a direct bony contact). [10]
Clavicle
The clavicle is an S-shaped bone that forms the anterior portion of the shoulder girdle that keeps the arm away from the trunk, allowing it to move freely. The clavicle has two articulations, the sternoclavicular joint and the AC joint.
The medial two thirds of the clavicle are convex anteriorly and serve as an attachment site for muscles such as the sternocleidomastoid (superiorly) and subclavius (inferiorly). The costal tuberosity on its inferior surface anchors the costoclavicular ligament. [11] The sternoclavicular joint is formed by the medial aspect of the clavicle articulating with the manubrium of the sternum. This is the only skeletal connection between the axial skeleton and the upper extremity.
The lateral one-third portion of the clavicle is concave anteriorly and provides attachment points for muscles such as the deltoid (anteriorly) and trapezius (posteriorly). The conoid tubercle and trapezoid line on its inferior surface serve as attachment sites for components of the coracoclavicular ligament. [11]
The clavicle acts as a strut to keep the scapula in position, ensuring proper alignment of the shoulder joint. It transmits mechanical forces from the upper limb to the axial skeleton. [1] Furthermore, the clavicle provides protection for the subclavian artery, subclavian vein, and brachial plexus posteriorly and inferiorly. See the images below.
Humeral head
The proximal articular surface of the humerus is termed the humeral head. The humeral head articulates against the shallow glenoid cavity.
The humeral head is covered with hyaline cartilage, facilitating smooth articulation with the glenoid cavity. The surface area of the humeral head is significantly larger than that of the glenoid cavity, with a ratio of approximately 4:1, which enhances mobility but reduces inherent stability. [12]
Only 25% of the humeral head surface makes contact with the glenoid cavity. [13] The glenoid labrum, a fibrocartilaginous ring attached to the outer rim of the glenoid cavity, provides additional depth and stability. The labrum deepens the relatively shallow glenoid cavity and increases its surface area, providing additional stability to the joint. It also plays a key role in maintaining a suction effect that helps stabilize the humeral head within the socket. [12]
The convexity of the humeral head exceeds the concavity of the glenoid cavity, contributing to its wide range of motion but predisposing it to instability. The dynamic and static stabilizers of the shoulder joint, including the rotator cuff muscles, joint capsule, and ligaments (e.g., superior glenohumeral ligament [SGHL], middle glenohumeral ligament [MGHL], and inferior glenohumeral ligament [IGHL]), work together to counteract this instability and maintain proper alignment during movement. [12]
Articulations
Sternoclavicular joint
The sternoclavicular joint is the sole connection between the axial skeleton and the upper extremity. It is a synovial saddle joint formed by articulation of the sternal end of the clavicle with the manubrium sterni and the first costal cartilage. [1] The sternoclavicular joint allows 30-35° of upward elevation, 35° of anteroposterior movement, and 44-50° of rotation about the long axis of the clavicle. [14] The joint is stabilized by strong ligaments, including the anterior and posterior sternoclavicular ligaments, interclavicular ligament, and costoclavicular ligament, which collectively ensure its stability while permitting mobility essential for shoulder girdle function. [1]
Acromioclavicular joint
The AC joint is a plane-type synovial joint. [1] It is the only articulation between the clavicle and scapula. It is formed by the distal clavicle articulating with the acromion of the scapula. Little motion exists in this joint. The AC joint is an encapsulated diarthrodial joint held together by its joint capsule and the coracoclavicular ligaments: the trapezoid and conoid ligaments. These ligaments are essential for maintaining stability, especially during overhead activities. Despite its limited range of motion, this joint plays a critical role in transmitting forces between the upper limb and axial skeleton. [1]
Glenohumeral joint
The glenohumeral joint is the main articulation of the shoulder joint. It is the multiaxial ball-and-socket synovial joint formed by the articular surfaces of the glenoid cavity and the head of the humerus. The glenoid labrum increases the glenoid cavity depth, contributing up to half of its depth. This joint allows for extensive mobility in multiple planes, including flexion, extension, abduction, adduction, internal rotation, external rotation, and circumduction. [1]
Labrum
The glenoid labrum is a ring composed of mostly dense fibrous tissue. The average depth of the glenoid cavity is 2.5 mm, but the labrum serves to increase this depth. Although the labrum increases the depth and volume of the glenoid cavity, it does not seem to increase the stability of the glenohumeral joint. [14] The labrum also serves as an attachment site for various structures, including the long head of the biceps brachii tendon superiorly. [1]
Ligaments
Coracoclavicular
The conoid and trapezoid ligaments comprise the coracoclavicular ligaments (see the image below). They function to maintain the articulation of the clavicle with the coracoid process of the scapula. Studies have concluded that the coracoclavicular ligaments are the primary restraint to superior and posterior clavicular dislocation. [15]
Glenohumeral
Three glenohumeral ligaments exist: (1) the SGHL, (2) the MGHL, and (3) the IGHL. SGHL has a variable origin and inserts on the humerus near the lesser tubercle; this ligament resists inferior translation of the humeral head in the adducted shoulder.
MGHL originates from the labrum and inserts on the humerus medial to the lesser tubercle; this ligament resists inferior translation in the adducted and externally rotated shoulder.
IGHL originates from the labrum and the adjacent glenoid neck, inserts on the anatomic neck of the humerus, and resists humeral head anterior and posterior translation. Furthermore, it is the primary restraint to inferior dislocation in the abducted shoulder.
Coracohumeral
The coracohumeral ligament originates on the base and lateral border of the coracoid process of the scapula and inserts on the greater tubercle. It blends with fibers of the SGHL and envelops portions of the rotator interval. It supports superior stability by limiting inferior subluxation of the humeral head and restraining excessive external rotation. [1] The biomechanical function of this ligament is not fully understood; however, it appears to have suspensory function of the humeral head.
Rotator Cuff
The supraspinatus, infraspinatus, teres minor, and subscapularis muscles comprise the rotator cuff (see the following image) (see Table 1 below). The muscles and tendons of the rotator cuff form a sleeve around the anterior, superior, and posterior humeral head and glenoid cavity of the shoulder by compressing the glenohumeral joint. In addition to stabilization, the rotator cuff provides the shoulder with tremendous mobility.
Table 1. Origins, Insertions, Actions, and Nerve Supplies of the Rotator Cuff Muscles (Open Table in a new window)
Muscle |
Origin |
Insertion |
Action |
Nerve Supply |
Supraspinatus |
Supraspinous fossa |
Greater tubercle of humerus |
Abduction of the arm to approximately 30º |
Suprascapular nerve |
Infraspinatus |
Infraspinous fossa |
Greater tubercle of humerus |
External (lateral) rotation of the arm |
Suprascapular nerve |
Teres minor |
Upper 2/3rd of the lateral border of the scapula |
Greater tubercle of humerus |
External (lateral) rotation of the arm |
Axillary nerve |
Subscapularis |
Subscapular fossa on the anterior surface of the scapula |
Lesser tubercle of humerus |
Internal (medial) rotation of the arm |
Upper and lower subscapular nerves |
The tendons of these muscles blend with the joint capsule to form a continuous structure that protects most of the joint. This configuration also allows for efficient force couples: vertical (coronal) coupling between supraspinatus and deltoid and horizontal (axial) coupling between subscapularis and infraspinatus/teres minor. [16]
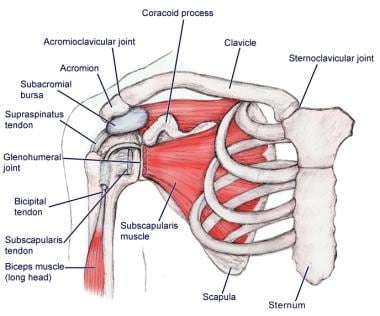
Subacromial/Subdeltoid Bursa
The subacromial bursa lies on the superior aspect of the supraspinatus tendon (see the images below). It is the largest bursa in the human body, located between the acromion, deltoid muscle, and rotator cuff tendons. [17] The bursa acts to cushion and reduce friction during motion between the overlying bone of the acromion and the soft rotator cuff muscles below. It often extends laterally to be continuous with the subdeltoid bursa.
Microscopic Anatomy
Connective Tissues and Muscles of the Shoulder
The shoulder complex is composed of many different tissue types, and it is the connective tissue that provides the supportive framework for the shoulder's many functions. The different types of connective tissues in the shoulder are the bone, articular cartilage, ligaments, joint capsules, and bursa (see Gross Anatomy).
The muscles of the shoulder joint are composed of skeletal muscle (see Skeletal Muscle - Structure and Histology and Skeletal Muscle Pathology).
Natural Variants
Labrum, Clavicle, and Scapular Notch Variability
Several minor anatomic variations exist in the attachment sites, size, and histologic composition of the labrum. These variations are not considered pathologic.
Sublabral recesses and sublabral foramina are common variants. The sublabral recess, a physiological sulcus at the superior glenoid rim, is often mistaken for pathology but represents a normal detachment of the labrum from the cartilage. Similarly, the sublabral foramen, found anteriorly between 1 and 3 o'clock positions, is another benign variant. These features should be distinguished from labral tears during imaging or arthroscopy to avoid misdiagnosis. Additionally, variations in the attachment of the long head of the biceps tendon to the superior glenoid rim influence labral morphology, with posterior-dominant attachments being most common. [18]
Variations in the shape of the clavicle are considered normal and are not usually pathologic. These variations may range from an almost straight bone to one with exaggerated curves. Another variation of the clavicle that is present in 6-10% of the population is termed the canalis nervi supraclavicularis. [19] In this variation, a foramen forms through the clavicle, and the medial supraclavicular nerve passes through this accessory osseous canal. Additionally, supraclavicular nerves may exhibit branching patterns that traverse over or through the clavicle, increasing the risk for iatrogenic nerve injury during clavicle fixation. [20]
The scapular notch varies in size and shape. The notch is bridged by the superior transverse scapular ligament. This ligament ossifies in 10% of patients, producing a bony foramen for the suprascapular nerve. [19]
The morphology of the scapular notch is classified into types based on its depth and width (e.g., U-shaped or V-shaped), with narrow V-shaped notches posing a higher risk for nerve compression. [21]
Pathophysiological Variants
Acromion Morphology Variability
Bigliani et al., separated acromions into three categories based on their shape and correlation with rotator cuff tears (see the image below) as follows:
-
Type I - Flat undersurface of the acromion. This type has the lowest risk for impingement syndrome.
-
Type II - Curved undersurface of the acromion
-
Type III - Hooked undersurface of the acromion. This type has the highest correlation with subacromial pathology.
Research has introduced a fourth type, type IV (convex undersurface), characterized by an upturned undersurface. However, its clinical significance regarding impingement or rotator cuff pathology remains inconclusive. [22]
Research suggests that the presence of an acromial spur, particularly the heel-type spur, is more significantly associated with full-thickness rotator cuff tears than other anatomical variants. Thus, specific morphological features such as acromial spurs may be more critical in assessing rotator cuff pathology than previously thought. [23]
Sprengel Deformity
Sprengel deformity is a congenital deformity; this is actually a composite of deformities caused by an undescended, hypoplastic scapula. People with Sprengel deformity have limited range of motion in abduction at the shoulder. [14] Such deformities include cosmetic concerns (e.g., a lump in the back and the appearance of a short neck). Also, 47% of people with Sprengel deformity develop scoliosis, and 29% develop Klippel-Feil syndrome. [14]
Acute Shoulder Injury
Clavicle Fracture
The clavicle plays a significant role in shoulder stability, strength, and range of motion. However, clavicle fractures are very common and account for 5% of all fractures in adults. Clavicle fractures can be categorized into the following three groups, as classified by Allman: [2]
-
Group 1 - A fracture in the middle of the clavicle; the most common clavicle fracture
-
Group 2 - Fracture on the lateral one third of the clavicle; osteoarthritis often develops after a group 2 fracture if the fracture involves the AC joint
-
Group 3 - Fracture on the medial one third of the clavicle; the rarest form of clavicle fracture
Proximal Humerus Fracture
The anatomic neck of the humerus lies at the junction of the humeral head and the tubercles. Fractures of the anatomic neck of the humeral head are quite rare and have a poor prognosis because the fracture usually disrupts blood supply to the humeral head. The surgical neck of the humerus is distal to the tubercles. Fractures of the surgical neck are more common and have a better prognosis.
Glenohumeral Dislocation
The glenohumeral joint is the major articulation of the shoulder joint. Dislocation of the glenohumeral joint occurs when the humeral head is moved out of contact with the glenoid cavity. Almost 85% of shoulder dislocations are anterior dislocations. [14] An anterior dislocation is likely to occur when the arm is abducted, extended, and externally rotated. Posterior dislocation of the glenohumeral joint is rare but is more likely to occur when the arm is adducted and internally (medially) rotated. Violent muscle contractions during a seizure or electrocution may also produce a posterior glenohumeral dislocation.
(See also Multidirectional Glenohumeral Instability, Anterior Glenohumeral Instability, Posterior Glenohumeral Instability.)
Acromioclavicular Joint Sprain or Dislocation (Shoulder Separation)
The AC joint is frequently injured in athletes. The injury commonly occurs when direct force is applied to the acromion with the arm adducted. The force causes the acromion to suddenly move inferiorly, which first strains or tears the AC ligaments and may subsequently strain or tear the coracoclavicular ligaments as well.
Rotator Cuff Tear
Rotator cuff tears are common injuries; such a diagnosis indicates that one or more of the rotator cuff tendons have torn. The injury may be a result of chronic impingement and tendonitis that has progressed or it may refer to an acute injury such as a fall or direct trauma. People with rotator cuff tears may experience pain and weakness in their shoulder. The supraspinatus muscle is the most frequently torn rotator cuff muscle.
Subacromial/Subdeltoid Bursitis
Inflammation of the bursa is relatively rare but may occur.
Labral Tear
People that participate in repetitive overhead activities such as swimming or throwing a ball have an increased risk for labral tear. A labral tear may be asymptomatic or manifest as shoulder instability, pain, or crepitus.
Glenohumeral Osteoarthritis
Glenohumeral osteoarthritis is a slowly progressive arthropathy that is caused by the loss or destruction of articular cartilage. This is usually a condition that develops as people age and their articular cartilage wears down. However, it can also be due to trauma such as humeral head fractures, shoulder dislocation, or rotator cuff tendon tears.
Adhesive Capsulitis
Primary adhesive capsulitis causes a painful and stiff shoulder usually without a known inciting event. The stiff glenohumeral joint is most likely a result of chronic inflammation and fibrosis. Adhesive capsulitis has three phases, and each phase typically lasts 4-6 weeks, with wide variability. The three phases are as follows:
- "Freezing phase": Spontaneous pain and stiffness in the shoulder
- "Frozen phase": Increased stiffness and stable or decreased pain
- "Thawing phase": Increased range of motion and decreased pain
-
Shoulder joint, anterior view.
-
Shoulder anatomy, lateral view.
-
Shoulder anatomy, posterior view.
-
Shoulder anatomy muscle, anterior view.
-
Acromion types.