Background
Hemorrhagic stroke is less common than ischemic stroke (ie, stroke caused by thrombosis or embolism); epidemiologic studies indicate that only 8–18% of strokes are hemorrhagic. However, hemorrhagic stroke is associated with higher mortality rates than is ischemic stroke.
Patients with hemorrhagic stroke may present with focal neurologic deficits similar to those seen in ischemic stroke, but they are often more acutely ill. Intracerebral hemorrhage is more commonly associated with headache, altered mental status, seizures, nausea and vomiting, and significant hypertension.
Brain imaging is a crucial step in the evaluation of suspected hemorrhagic stroke and must be obtained on an emergent basis (see the image below). Brain imaging aids in excluding ischemic stroke, and it may identify complications of hemorrhagic stroke such as intraventricular hemorrhage, brain edema, and hydrocephalus. Either noncontrast computed tomography (NCCT) scanning or magnetic resonance imaging (MRI) is the modality of choice.
 Axial noncontrast computed tomography scan of the brain of a 60-year-old man with a history of acute onset of left-sided weakness. Two areas of intracerebral hemorrhage are seen in the right lentiform nucleus, with surrounding edema and effacement of the adjacent cortical sulci and right sylvian fissure. Mass effect is present upon the frontal horn of the right lateral ventricle, with intraventricular extension of the hemorrhage.
Axial noncontrast computed tomography scan of the brain of a 60-year-old man with a history of acute onset of left-sided weakness. Two areas of intracerebral hemorrhage are seen in the right lentiform nucleus, with surrounding edema and effacement of the adjacent cortical sulci and right sylvian fissure. Mass effect is present upon the frontal horn of the right lateral ventricle, with intraventricular extension of the hemorrhage.
Anatomy
Knowledge of cerebrovascular arterial anatomy and the brain regions supplied by the arteries is useful in determining which vessels are involved in acute stroke. Atypical patterns that do not conform to a vascular distribution may indicate another diagnosis, such as venous infarction.
The cerebral hemispheres are supplied by three paired major arteries: the anterior, middle, and posterior cerebral arteries. The anterior and middle cerebral arteries are responsible for the anterior circulation and arise from the supraclinoid internal carotid arteries. The posterior cerebral arteries arise from the basilar artery and form the posterior circulation, which also supplies the thalami, brainstem, and cerebellum. The angiograms in the images below demonstrate some portions of the circulation involved in hemorrhagic strokes.
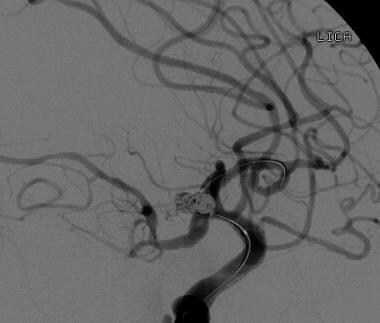
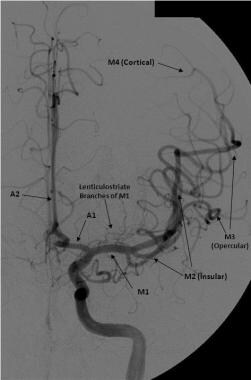 Frontal view of a cerebral angiogram with selective injection of the left internal carotid artery illustrates the anterior circulation. The anterior cerebral artery consists of the A1 segment proximal to the anterior communicating artery with the A2 segment distal to it. The middle cerebral artery can be divided into 4 segments: the M1 (horizontal segment) extends to the limen insulae and gives off lateral lenticulostriate branches, the M2 (insular segment), M3 (opercular branches), and M4 (distal cortical branches on the lateral hemispheric convexities).
Frontal view of a cerebral angiogram with selective injection of the left internal carotid artery illustrates the anterior circulation. The anterior cerebral artery consists of the A1 segment proximal to the anterior communicating artery with the A2 segment distal to it. The middle cerebral artery can be divided into 4 segments: the M1 (horizontal segment) extends to the limen insulae and gives off lateral lenticulostriate branches, the M2 (insular segment), M3 (opercular branches), and M4 (distal cortical branches on the lateral hemispheric convexities).
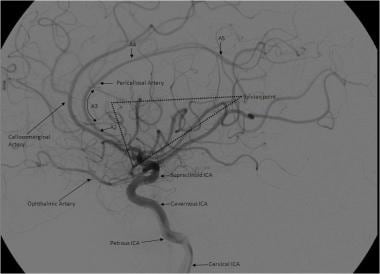 Lateral view of a cerebral angiogram illustrates the branches of the anterior cerebral artery (ACA) and sylvian triangle. The pericallosal artery has been described as arising distal to the anterior communicating artery or distal to the origin of the callosomarginal branch of the ACA. The segmental anatomy of the ACA has been described as follows: (1) the A1 segment extends from the internal carotid artery (ICA) bifurcation to the anterior communicating artery, (2) A2 extends to the junction of the rostrum and genu of the corpus callosum, (3) A3 extends into the bend of the genu of the corpus callosum, and (4) A4 and A5 extend posteriorly above the callosal body and superior portion of the splenium. The sylvian triangle overlies the opercular branches of the middle cerebral artery, with the apex representing the sylvian point.
Lateral view of a cerebral angiogram illustrates the branches of the anterior cerebral artery (ACA) and sylvian triangle. The pericallosal artery has been described as arising distal to the anterior communicating artery or distal to the origin of the callosomarginal branch of the ACA. The segmental anatomy of the ACA has been described as follows: (1) the A1 segment extends from the internal carotid artery (ICA) bifurcation to the anterior communicating artery, (2) A2 extends to the junction of the rostrum and genu of the corpus callosum, (3) A3 extends into the bend of the genu of the corpus callosum, and (4) A4 and A5 extend posteriorly above the callosal body and superior portion of the splenium. The sylvian triangle overlies the opercular branches of the middle cerebral artery, with the apex representing the sylvian point.
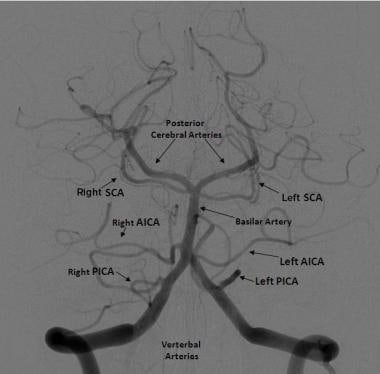 Frontal projection from a right vertebral artery angiogram illustrates the posterior circulation. The vertebral arteries join to form the basilar artery. The posterior inferior cerebellar arteries (PICA) arise from the distal vertebral arteries. The anterior inferior cerebellar arteries (AICA) arise from the proximal basilar artery. The superior cerebellar arteries (SCA) arise distally from the basilar artery before its bifurcation into the posterior cerebral arteries.
Frontal projection from a right vertebral artery angiogram illustrates the posterior circulation. The vertebral arteries join to form the basilar artery. The posterior inferior cerebellar arteries (PICA) arise from the distal vertebral arteries. The anterior inferior cerebellar arteries (AICA) arise from the proximal basilar artery. The superior cerebellar arteries (SCA) arise distally from the basilar artery before its bifurcation into the posterior cerebral arteries.
Etiology
The etiologies of stroke are varied, but they can be broadly categorized into ischemic or hemorrhagic. Approximately 85–87% of strokes are from ischemic infarction caused by thrombotic or embolic cerebrovascular occlusion. Intracerebral hemorrhages account for most of the remainder of strokes, with a smaller number resulting from aneurysmal subarachnoid hemorrhage.
In 20–40% of patients with ischemic infarction, hemorrhagic transformation may occur within 1 week after ictus.
Differentiating between the different types of stroke is an essential part of the initial workup of patients with stroke, as the subsequent management of each disorder will be vastly different.
Risk factors
The risk of hemorrhagic stroke is increased with the following factors:
-
Advanced age
-
Hypertension (present in up to 70–80% of cases)
-
Previous history of stroke
-
Alcohol abuse
-
Use of illicit drugs (eg, cocaine, other sympathomimetic drugs)
Causes of hemorrhagic stroke include the following:
-
Hypertension
-
Cerebral amyloidosis
-
Coagulopathies
-
Anticoagulant therapy
-
Thrombolytic therapy for acute myocardial infarction (MI) or acute ischemic stroke (can cause iatrogenic hemorrhagic transformation)
-
Arteriovenous malformation (AVM), aneurysms, and other vascular malformations (venous and cavernous angiomas)
-
Vasculitis
-
Intracranial neoplasm
Hypertension
The most common etiology of primary hemorrhagic stroke (intracerebral hemorrhage) is hypertension. At least two thirds of patients with primary intraparenchymal hemorrhage are reported to have preexisting or newly diagnosed hypertension. Hypertensive small-vessel disease results from tiny lipohyalinotic aneurysms that subsequently rupture and result in intraparenchymal hemorrhage. Typical locations include the basal ganglia, thalami, cerebellum, and pons.
Amyloidosis
Cerebral amyloidosis affects people who are elderly and may cause up to 10% of intracerebral hemorrhages. Rarely, cerebral amyloid angiopathy can be caused by mutations in the amyloid precursor protein and is inherited in an autosomal dominant fashion.
Coagulopathies
Coagulopathies may be acquired or inherited. Liver disease can result in a bleeding diathesis. Inherited disorders of coagulation such as factor VII, VIII, IX, X, and XIII deficiency can predispose to excessive bleeding, and intracranial hemorrhage has been seen in all of these disorders.
Anticoagulant therapy
Anticoagulant therapy is especially likely to increase hemorrhage risk in patients who metabolize warfarin inefficiently. Warfarin metabolism is influenced by polymorphism in the CYP2C9 genes. Three known variants have been described. CYP2C9*1 is the normal variant and is associated with typical response to dosage of warfarin. Variations *2 and *3 are relatively common polymorphisms that reduce the efficiency of warfarin metabolism.
Arteriovenous malformations
Numerous genetic causes may predispose to AVMs in the brain, although AVMs are generally sporadic. Polymorphisms in the IL6 gene increase susceptibility to a number of disorders, including AVM. Hereditary hemorrhagic telangiectasia (HHT), previously known as Osler-Weber-Rendu syndrome, is an autosomal dominant disorder that causes dysplasia of the vasculature. HHT is caused by mutations in ENG, ACVRL1, or SMAD4 genes. Mutations in SMAD4 are also associated with juvenile polyposis, so this must be considered when obtaining the patient’s history.
HHT is most frequently diagnosed when patients present with telangiectasias on the skin and mucosa or with chronic epistaxis from AVMs in the nasal mucosa. Additionally, HHT can result in AVMs in any organ system or vascular bed. AVM in the gastrointestinal tract, lungs, and brain are the most worrisome, and their detection is the mainstay of surveillance for this disease.
Cholesterol
A study of almost 28,000 women over a period of approximately 20 years found that women with very low levels of low-density lipoprotein cholesterol (LDL-C) (< 70 mg/dL) may be more than twice as likely to have a hemorrhagic stroke than women with higher levels (100–130 mg/dL). Causality remains unclear, however. Guidelines do not currently recommend avoiding LDL-lowering therapy solely due to hemorrhagic stroke risk.
Aneurysms and subarachnoid hemorrhage
The most common cause of atraumatic hemorrhage into the subarachnoid space is rupture of an intracranial aneurysm. Aneurysms are focal dilatations of arteries, with the most frequently encountered intracranial type being the berry (saccular) aneurysm. Aneurysms may less commonly be related to altered hemodynamics associated with AVMs, collagen vascular disease, polycystic kidney disease, septic emboli, and neoplasms.
Nonaneurysmal perimesencephalic subarachnoid hemorrhage may also be seen. This phenomenon is thought to arise from capillary or venous rupture. It has a less severe clinical course and, in general, a better prognosis.
Berry aneurysms are most often isolated lesions whose formation results from a combination of hemodynamic stresses and acquired or congenital weakness in the vessel wall. Saccular aneurysms typically occur at vascular bifurcations, with more than 90% occurring in the anterior circulation. Common sites include the following:
-
The junction of the anterior communicating arteries and anterior cerebral arteries—most commonly, the middle cerebral artery (MCA) bifurcation
-
The supraclinoid internal carotid artery at the origin of the posterior communicating artery
-
The bifurcation of the internal carotid artery (ICA)
Genetic causes of aneurysms
Intracranial aneurysms may result from genetic disorders. Although rare, several families have been described that have a predisposition—inherited in an autosomal dominant fashion—to intracranial berry aneurysms. A number of genes, all categorized as ANIB genes, are associated with this predisposition. Presently, ANIB1 through ANIB11 are known.
Autosomal dominant polycystic kidney disease (ADPKD) is another cause of intracranial aneurysm. Families with ADPKD tend to show phenotypic similarity with regard to intracranial hemorrhage or asymptomatic berry aneurysms.
Loeys-Dietz syndrome (LDS) consists of craniofacial abnormalities, craniosynostosis, marked arterial tortuosity, and aneurysms and is inherited in an autosomal dominant manner. Although intracranial aneurysms occur in LDS of all types, saccular intracranial aneurysms are a prominent feature of LDS type IC, which is caused by mutations in the SMAD3 gene.
Ehlers-Danlos syndrome is a group of inherited disorders of the connective tissue that feature hyperextensibility of the joints and changes to the skin, including poor wound healing, fragility, and hyperextensibility. However, Ehlers-Danlos vascular type (type IV) also is known to cause spontaneous rupture of hollow viscera and large arteries, including arteries in the intracranial circulation.
Patients with Ehlers-Danlos syndrome may also have mild facial findings, including lobeless ears, a thin upper lip, and a thin, sharp nose. The distal fingers may appear prematurely aged (acrogeria). In the absence of a suggestive family history, it is difficult to separate Ehlers-Danlos vascular type from other forms of Ehlers-Danlos. Ehlers-Danlos vascular type is caused by mutations in the COL3A1 gene; it is inherited in an autosomal dominant manner.
Hemorrhagic transformation of ischemic stroke
Hemorrhagic transformation represents the conversion of a bland infarction into an area of hemorrhage. Proposed mechanisms for hemorrhagic transformation include reperfusion of ischemically injured tissue, either from recanalization of an occluded vessel or from collateral blood supply to the ischemic territory or disruption of the blood-brain barrier. With disruption of the blood-brain barrier, red blood cells extravasate from the weakened capillary bed, producing petechial hemorrhage or frank intraparenchymal hematoma. (For more information, see Reperfusion Injury in Stroke.)
Hemorrhagic transformation of an ischemic infarct occurs within 2–14 days postictus, usually within the first week. It is more commonly seen following cardioembolic strokes and is more likely with larger infarct size. Hemorrhagic transformation is also more likely following administration of tissue plasminogen activator (tPA) in patients whose noncontrast computed tomography (CT) scans demonstrate areas of hypodensity. See the image below.
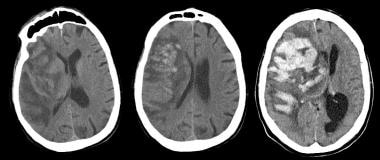 Noncontrast computed tomography scan (left) obtained in a 75-year-old man who was admitted for stroke demonstrates a large right middle cerebral artery distribution infarction with linear areas of developing hemorrhage. These become more confluent on day 2 of hospitalization (middle image), with increased mass effect and midline shift. There is massive hemorrhagic transformation by day 6 (right), with increased leftward midline shift and subfalcine herniation. Obstructive hydrocephalus is also noted, with dilatation of the lateral ventricles, likely due to compression of the foramen of Monroe. Intraventricular hemorrhage is also noted layering in the left occipital horn. Larger infarctions are more likely to undergo hemorrhagic transformation and are one contraindication to thrombolytic therapy.
Noncontrast computed tomography scan (left) obtained in a 75-year-old man who was admitted for stroke demonstrates a large right middle cerebral artery distribution infarction with linear areas of developing hemorrhage. These become more confluent on day 2 of hospitalization (middle image), with increased mass effect and midline shift. There is massive hemorrhagic transformation by day 6 (right), with increased leftward midline shift and subfalcine herniation. Obstructive hydrocephalus is also noted, with dilatation of the lateral ventricles, likely due to compression of the foramen of Monroe. Intraventricular hemorrhage is also noted layering in the left occipital horn. Larger infarctions are more likely to undergo hemorrhagic transformation and are one contraindication to thrombolytic therapy.
Pathophysiology
In intracerebral hemorrhage, bleeding occurs directly into the brain parenchyma. The usual mechanism is thought to be leakage from small intracerebral arteries damaged by chronic hypertension. Other mechanisms include bleeding diatheses, iatrogenic anticoagulation, cerebral amyloidosis, and cocaine abuse.
Intracerebral hemorrhage has a predilection for certain sites in the brain, including the thalamus, putamen, cerebellum, and brainstem. In addition to the area of the brain injured by the hemorrhage, the surrounding brain can be damaged by pressure produced by the mass effect of the hematoma. A general increase in intracranial pressure may occur.
Subarachnoid hemorrhage
The pathologic effects of subarachnoid hemorrhage (SAH) on the brain are multifocal. SAH results in elevated intracranial pressure and impairs cerebral autoregulation. These effects can occur in combination with acute vasoconstriction, microvascular platelet aggregation, and loss of microvascular perfusion, resulting in profound reduction in blood flow and cerebral ischemia. See the images below.
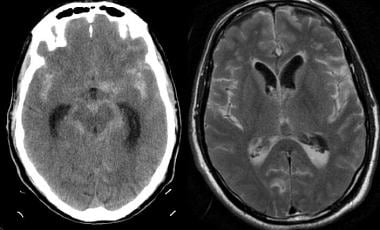 Noncontrast computed tomography (CT) scanning was performed emergently in a 71-year-old man who presented with acute onset of severe headache and underwent rapid neurologic deterioration requiring intubation. The noncontrast CT scan (left image) demonstrates diffuse, high-density subarachnoid hemorrhage in the basilar cisterns and both Sylvian fissures. There is diffuse loss of gray-white differentiation. The fluid-attenuated inversion-recovery (FLAIR) image (right) demonstrates high signal throughout the cortical sulci and in the basilar cisterns, as well as in the dependent portions of the ventricles. FLAIR is highly sensitive to acute subarachnoid hemorrhage; the suppression of high cerebrospinal fluid signal aids in making subarachnoid hemorrhage more conspicuous than do conventional magnetic resonance imaging sequences.
Noncontrast computed tomography (CT) scanning was performed emergently in a 71-year-old man who presented with acute onset of severe headache and underwent rapid neurologic deterioration requiring intubation. The noncontrast CT scan (left image) demonstrates diffuse, high-density subarachnoid hemorrhage in the basilar cisterns and both Sylvian fissures. There is diffuse loss of gray-white differentiation. The fluid-attenuated inversion-recovery (FLAIR) image (right) demonstrates high signal throughout the cortical sulci and in the basilar cisterns, as well as in the dependent portions of the ventricles. FLAIR is highly sensitive to acute subarachnoid hemorrhage; the suppression of high cerebrospinal fluid signal aids in making subarachnoid hemorrhage more conspicuous than do conventional magnetic resonance imaging sequences.
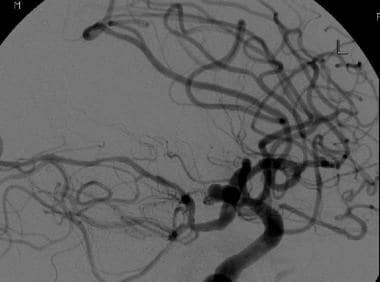 Computed tomographic angiography examination and subsequent cerebral angiography were performed in 71-year-old man who presented with acute onset of severe headache and underwent rapid neurologic deterioration. Multiple aneurysms were identified, including a 9-mm aneurysm at the junction of the anterior cerebral and posterior communicating arteries seen on this lateral view of an internal carotid artery injection. Balloon-assisted coil embolization was performed.
Computed tomographic angiography examination and subsequent cerebral angiography were performed in 71-year-old man who presented with acute onset of severe headache and underwent rapid neurologic deterioration. Multiple aneurysms were identified, including a 9-mm aneurysm at the junction of the anterior cerebral and posterior communicating arteries seen on this lateral view of an internal carotid artery injection. Balloon-assisted coil embolization was performed.
Epidemiology
Prevalence
Stroke is the second leading cause of death and a major contributor to long-term disability worldwide. In 2019, an estimated 12.2 million individuals experienced a new stroke, resulting in 6.55 million deaths. In the United States, stroke is the fifth leading cause of death and a leading cause of serious disability, with a prevalence of 3.3% and approximately 795,000 new or recurrent strokes annually.
Hemorrhagic stroke accounts for approximately 10% of all incident strokes but contributes disproportionately to stroke-related mortality and disability-adjusted life-years lost compared with ischemic stroke. Intracerebral hemorrhage (ICH) comprises about 75% of hemorrhagic strokes, with the remainder due to subarachnoid hemorrhage. In 2020, the global prevalence of ICH was estimated at 18.88 million cases, with a 3.33% decrease in the age-standardized prevalence rate compared to 2010. In 2021, ICH was responsible for an estimated 3.31 million deaths worldwide, although the age-standardized mortality rate declined between 2010 and 2021. Regional mortality rates were highest in Oceania, followed by Southeast and East Asia, and Central and Eastern sub-Saharan Africa. The estimated global lifetime risk of hemorrhagic stroke from age 25 onward is 8.2%.
The incidence of stroke varies with age, sex, ethnicity, and socioeconomic status. Studies have consistently shown that Black and Hispanic individuals have a higher incidence of ICH compared to their White counterparts.
Prognosis
The prognosis in patients with hemorrhagic stroke varies depending on the severity of stroke and the location and the size of the hemorrhage. Lower Glasgow Coma Scale (GCS) scores are associated with poorer prognosis and higher mortality rates. A larger volume of blood at presentation is also associated with a poorer prognosis. Growth of the hematoma volume is associated with a poorer functional outcome and increased mortality rate.
The intracerebral hemorrhage score is the most commonly used instrument for predicting outcome in hemorrhagic stroke. The score is calculated as follows:
-
GCS score 3–4: 2 points
-
GCS score 5–12: 1 point
-
GCS score 13–15: 0 points
-
Age ≥80 years: Yes, 1 point; no, 0 points
-
Infratentorial origin: Yes, 1 point; no, 0 points
-
Intracerebral hemorrhage volume ≥ 30 cm3: 1 point
-
Intracerebral hemorrhage volume < 30 cm3: 0 points
-
Intraventricular hemorrhage: Yes, 1 point; no, 0 points
In a study by Hemphill et al, all patients with an Intracerebral Hemorrhage Score of 0 survived, and all of those with a score of 5 died; 30-day mortality increased steadily with the Score.
Other prognostic factors include the following:
-
Nonaneurysmal perimesencephalic stroke has a less severe clinical course and, in general, a better prognosis
-
The presence of blood in the ventricles is associated with a higher mortality rate; in one study, the presence of intraventricular blood at presentation was associated with a mortality increase of more than 2-fold
-
Patients with oral anticoagulation-associated intracerebral hemorrhage have higher mortality rates and poorer functional outcomes
In studies, withdrawal of medical support or issuance of Do Not Resuscitate (DNR) orders within the first day of hospitalization predict poor outcome independent of clinical factors. Because limiting care may adversely impact outcome, American Heart Association/American Stroke Association (AHA/ASA) guidelines suggest that new DNR orders should probably be postponed until at least the second full day of hospitalization. Patients with DNRs should be given all other medical and surgical treatment, unless the DNR explicitly says otherwise.
-
Axial noncontrast computed tomography scan of the brain of a 60-year-old man with a history of acute onset of left-sided weakness. Two areas of intracerebral hemorrhage are seen in the right lentiform nucleus, with surrounding edema and effacement of the adjacent cortical sulci and right sylvian fissure. Mass effect is present upon the frontal horn of the right lateral ventricle, with intraventricular extension of the hemorrhage.
-
Noncontrast computed tomography scan of the brain (left) demonstrates an acute hemorrhage in the left gangliocapsular region, with surrounding white matter hypodensity consistent with vasogenic edema. T2-weighted axial magnetic resonance imaging scan (middle image) again demonstrates the hemorrhage, with surrounding high-signal edema. The coronal gradient-echo image (right) demonstrates susceptibility related to the hematoma, with markedly low signal adjacent the left caudate head. Gradient-echo images are highly sensitive for blood products.
-
Noncontrast computed tomography scan (left) obtained in a 75-year-old man who was admitted for stroke demonstrates a large right middle cerebral artery distribution infarction with linear areas of developing hemorrhage. These become more confluent on day 2 of hospitalization (middle image), with increased mass effect and midline shift. There is massive hemorrhagic transformation by day 6 (right), with increased leftward midline shift and subfalcine herniation. Obstructive hydrocephalus is also noted, with dilatation of the lateral ventricles, likely due to compression of the foramen of Monroe. Intraventricular hemorrhage is also noted layering in the left occipital horn. Larger infarctions are more likely to undergo hemorrhagic transformation and are one contraindication to thrombolytic therapy.
-
Noncontrast computed tomography (CT) scanning was performed emergently in a 71-year-old man who presented with acute onset of severe headache and underwent rapid neurologic deterioration requiring intubation. The noncontrast CT scan (left image) demonstrates diffuse, high-density subarachnoid hemorrhage in the basilar cisterns and both Sylvian fissures. There is diffuse loss of gray-white differentiation. The fluid-attenuated inversion-recovery (FLAIR) image (right) demonstrates high signal throughout the cortical sulci and in the basilar cisterns, as well as in the dependent portions of the ventricles. FLAIR is highly sensitive to acute subarachnoid hemorrhage; the suppression of high cerebrospinal fluid signal aids in making subarachnoid hemorrhage more conspicuous than do conventional magnetic resonance imaging sequences.
-
Computed tomographic angiography examination and subsequent cerebral angiography were performed in 71-year-old man who presented with acute onset of severe headache and underwent rapid neurologic deterioration. Multiple aneurysms were identified, including a 9-mm aneurysm at the junction of the anterior cerebral and posterior communicating arteries seen on this lateral view of an internal carotid artery injection. Balloon-assisted coil embolization was performed.
-
Lateral view of a selective injection of the left internal carotid artery demonstrates a microcatheter passing distal to the aneurysm neck. This lateral view from an angiogram performed during balloon-assisted coil embolization demonstrates significantly diminished filling of the aneurysm.
-
Lateral view of a cerebral angiogram illustrates the branches of the anterior cerebral artery (ACA) and sylvian triangle. The pericallosal artery has been described as arising distal to the anterior communicating artery or distal to the origin of the callosomarginal branch of the ACA. The segmental anatomy of the ACA has been described as follows: (1) the A1 segment extends from the internal carotid artery (ICA) bifurcation to the anterior communicating artery, (2) A2 extends to the junction of the rostrum and genu of the corpus callosum, (3) A3 extends into the bend of the genu of the corpus callosum, and (4) A4 and A5 extend posteriorly above the callosal body and superior portion of the splenium. The sylvian triangle overlies the opercular branches of the middle cerebral artery, with the apex representing the sylvian point.
-
Frontal projection from a right vertebral artery angiogram illustrates the posterior circulation. The vertebral arteries join to form the basilar artery. The posterior inferior cerebellar arteries (PICA) arise from the distal vertebral arteries. The anterior inferior cerebellar arteries (AICA) arise from the proximal basilar artery. The superior cerebellar arteries (SCA) arise distally from the basilar artery before its bifurcation into the posterior cerebral arteries.
-
Frontal view of a cerebral angiogram with selective injection of the left internal carotid artery illustrates the anterior circulation. The anterior cerebral artery consists of the A1 segment proximal to the anterior communicating artery with the A2 segment distal to it. The middle cerebral artery can be divided into 4 segments: the M1 (horizontal segment) extends to the limen insulae and gives off lateral lenticulostriate branches, the M2 (insular segment), M3 (opercular branches), and M4 (distal cortical branches on the lateral hemispheric convexities).
-
Frontal view from a cerebral angiogram in a 41-year-man who presented 7 days earlier with subarachnoid hemorrhage from a ruptured anterior communicating artery (ACA) aneurysm (which was treated with surgical clipping). There is significant narrowing of the proximal left ACA, left M1 segment, and left supraclinoid internal carotid artery, indicating vasospasm.
-
Angiographic view in a 41-year-man who presented 7 days earlier with subarachnoid hemorrhage from a ruptured anterior communicating artery (ACA) aneurysm (which was treated with surgical clipping). Superimposed road map image demonstrates placement of a wire across the left M1 segment and balloon angioplasty. The left proximal ACA and supraclinoid internal carotid artery (ICA) were also angioplastied, and intra-arterial verapamil was administered. Follow-up image on the right after treatment demonstrates resolution of the left M1 segment and distal ICA, which are now widely patent. Residual narrowing is seen in the left proximal ACA.
-
A cerebral angiogram was performed in a 57-year-old man with a family history of subarachnoid hemorrhage and who was found on previous imaging to have a left distal internal carotid artery (ICA) aneurysm. The lateral projection from this angiogram demonstrates a narrow-necked aneurysm arising off the posterior aspect of the distal supraclinoid left ICA, with an additional nipplelike projection off the inferior aspect of the dome of the aneurysm. There is also a mild, lobulated dilatation of the cavernous left ICA.
-
Follow-up cerebral angiogram after coil embolization in a 57-year-old man with a left distal internal carotid artery aneurysm. Multiple coils were placed with sequential occlusion of the aneurysm, including the nipple at its inferior aspect. A small amount of residual filling is noted at the proximal neck of the aneurysm, which may thrombose over time.
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Treatment
- Guidelines
- Medication
- Anticonvulsants, Hydantoins
- Beta Blockers, Alpha Activity
- Beta Blockers, Beta-1 Selective
- Vasodilators
- Calcium Channel Blockers
- Angiotensin-converting Enzyme Inhibitors
- Angiotensin Receptor Blockers
- Diuretics, Thiazide
- Diuretics, Osmotic Agents
- Analgesics, Other
- Hemostatics
- Blood Components
- Antidotes, Other
- Vasopressin-Related
- Anticonvulsants, Benzodiazepine
- Show All
- Media Gallery
- References