Overview
For the purpose of this article on eye globe anatomy, the eye will be divided into two sections: the extraocular (i.e., structures outside of the globe) and the ocular (i.e., the globe and the intraocular structures).
Throughout the years, in the absence of ancillary or diagnostic tools, many descriptive phrases, clichés, or analogies have been used to describe the eye, such as "the eye is the window to the soul," the "eye works like a camera," and "the eye is the only structure that allows us to physically see blood vessels and nerve fibers." We use our eyes daily and in almost every activity we perform (e.g., reading, driving, watching). At the foundation, the eye is a sensory organ that detects specifically photons.
Photons within the visible spectrum (i.e., light) enter the eye first by passing through the cornea, a clear, dome-shaped structure at the anterior post portion of the globe. Light passing through the cornea is converged (bent) where it passes through the anterior chamber and the pupil, a circular opening regulating the amount of light entering the eye. Light is further converged by the crystalline lens located posterior to the iris.
Light continues through the vitreous humor and the light converges on the retina, specifically the fovea centralis of the macula. Within the layers of the retina, photons trigger a series of electrical and chemical reactions, ultimately sending electrical signals by way of the optic nerve, along with visual pathway to the occipital cortex. Within the occipital cortices, these electrical signals are processed and interpreted (i.e., "seen") by the brain as a visual image. [1]
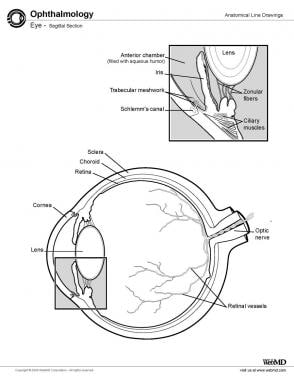
The image below depicts a sagittal section of the eye.
Extraocular Structures
Several structures exist within the category of extraocular structures, including the orbit, extraocular muscles, conjunctiva, lacrimal system, and eyelids. The functions associated with these structures include protection and lubrication.
Orbit
The orbit is a cone-shaped (four-sided pyramidal cavity) structure consisting of a base (the orbital margin) that opens into the midline of the face, the apex, the narrow end pointed posteriorly into the head, and the four walls.
In adults, the orbit is formed by seven bones: (1) frontal, (2) zygoma, (3) maxilla, (4) ethmoid, (5) sphenoid, (6) lacrimal, and (7) palatine. The frontal, ethmoid, and sphenoid are the only three unpaired bones of the orbit. The orbital margin (base) is formed by the maxillary, zygomatic, frontal, and lacrimal bones. The lesser wing of the sphenoid and frontal bones form the roof of the orbit, whereas the maxillary, zygomatic, and palatine bones form the floor of the orbit. The medial wall is formed by the sphenoid, ethmoid, lacrimal, and maxillary bones. The lateral wall is formed by the greater wing of the sphenoid and zygomatic bones.
The orbit has a volume of 30 mL, measures 4 cm horizontally and 3.5 cm vertically, and has a depth (anteroposteriorly) of 4.5 cm. Associated with the orbit are the foramina and fissures (see Table 1, below), which are important in transmitting nerves, arteries, and veins. The primary function of the orbit is to protect the eye from physical injuries. Other functions include the housing and support of the globe and associated structures, the facilitation of eye movement through the attachment of extraocular muscles, and the provision of pathways for neurovascular structures. [2]
Table 1. Contents of Orbital Foramens and Fissures (Open Table in a new window)
|
Nerve(s) |
Artery(ies) |
Vein(s) |
Other Structure(s) |
Supraorbital foramen |
Supraorbital nerve (from frontal branch of cranial nerve [CN] V1) |
Supraorbital |
|
|
Superior orbital fissure |
|
|
Superior ophthalmic |
|
Inferior orbital fissure |
|
Infraorbital |
Pterygoid plexus communication with inferior ophthalmic |
|
Optic canal |
|
Ophthalmic |
|
|
Anterior ethmoidal foramen |
Anterior ethmoidal |
Anterior ethmoidal |
Anterior ethmoidal |
|
Posterior ethmoidal foramen |
Posterior ethmoidal |
Posterior ethmoidal |
Posterior ethmoidal |
|
Zygomatic foramen |
Zygomatic branch of CN V2 (zygomaticofacial and zygomaticotemporal branches) |
Zygomatic |
|
|
Lacrimal fossa |
|
|
|
Lacrimal gland |
Fossa for lacrimal sac |
|
|
|
Lacrimal sac and nasolacrimal duct |
Extraocular Muscles
The extraocular muscles control the movements of the eye (see Table 2, below). Six extraocular muscles exist: four rectus muscles (superior, inferior, medial, and lateral) and two oblique muscles (superior and inferior). The extraocular muscles are innervated by three CNs: oculomotor (CN III), trochlear (CN IV), and abducens nerves (CN VI).
-
Oculomotor nerve (CN III) - Superior, medial, and inferior rectus; inferior oblique; levator palpebrae superioris
-
Trochlear nerve (CN IV) - Superior oblique
-
Abducens nerve (CN VI) - Lateral rectus [3]
The levator palpebrae superioris is the other extraocular muscle that, although not directly involved in eye movement, is primarily responsible for elevating the upper eyelid.
The origin of the four rectus muscles is the common ring tendon (annulus of Zinn) at the orbital apex. The rectus muscles insert on the sclera anterior to the equator. The insertions of the rectus muscles are not equidistant from the limbus. The imaginary line connecting the insertions of the four rectus muscles is known as the spiral of Tillaux.
The origin of the superior oblique is the sphenoid bone and has a long (10 + 10 mm) tendinous insertion. It inserts superior and temporal to the posterior pole and is covered by the superior rectus. The origin of the inferior oblique is the maxilla and has a muscular insertion temporal and inferior to the geometric posterior pole and covers the inferior rectus.
Table 2. Extraocular Muscles (Open Table in a new window)
Muscle |
Origin |
Insertion |
Distance From the Limbus |
Innervation |
Primary Function |
Length of Active Muscle (mm) |
Length of Tendon (mm) |
Direction of Pull (degree)* |
Arc of Contact (mm) |
Superior rectus |
Common ring tendon |
Anterior and superior surface |
7.7 mm |
Superior branch of cranial nerve [CN] III |
Elevation, intorsion, adduction |
±40 |
6 |
23 |
6.5 |
Lateral rectus |
Common ring tendon |
Anterior and lateral surface |
7.0 mm |
Abducens nerve (CN VI) |
Abduction |
±40 |
7 |
90 |
12 |
Inferior rectus |
Common ring tendon |
Anterior and inferior surface |
6.5 mm |
Inferior branch of CN III |
Depression, extorsion, adduction |
±40 |
7 |
23 |
6.5 |
Medial rectus |
Common ring tendon |
Anterior and medial surface |
5.5 mm |
Inferior branch of CN III |
Adduction |
±39 |
4.5 |
90 |
7 |
Superior oblique |
Sphenoid, orbit apex above common ring tendon |
Posterior, temporosuperior quadrant |
|
Trochlear nerve (CN IV) |
Intorsion, depression, abduction |
±32 |
26 |
51 |
7-8 |
Inferior oblique |
Maxilla, behind the lacrimal fossa |
Posterior, temporoinferior quadrant |
|
Inferior branch of CN III |
Extorsion, elevation abduction |
±37 |
1 |
51 |
15 |
Levator palpebrae superioris |
Orbit apex above common ring tendon |
|
|
Superior branch of CN III |
Lid elevation |
|
|
|
|
* Relative to the visual axis in the primary position. |
|||||||||
The extraocular muscles have a large ratio of nerve fibers to muscle fibers (1:3 to 1:5) compared to other skeletal muscles (1:50 to 1:125). This allows for precise control of eye movements. [4]
Conjunctiva
The conjunctiva is a thin, transparent mucous membrane overlying the anterior-most portion of the sclera and lining the inner surfaces of the eyelids. The conjunctiva is divided into the limbal, bulbar, forniceal, and palpebral regions. [2, 5, 6]
-
Limbal conjunctiva - The transition zone between the cornea and the bulbar conjunctiva
-
Bulbar conjunctiva - Covers the anterior portion of the eyeball, extending from the corneoscleral limbus onto the surface of the globe
-
Forniceal conjunctiva - Forms the superior and inferior fornices, which are deep recesses where the bulbar and palpebral conjunctiva meet
-
Palpebral (tarsal) conjunctiva - Lines the posterior surface of the eyelids
The conjunctival epithelium varies in structure depending on its location: [6]
-
Near the limbus - Columnar epithelium
-
Closer to the fornix - Squamous epithelium
The epithelium is non-keratinized and typically consists of 5-7 cell layers. Beneath the epithelium lies the substantia propria, a fibrovascular connective tissue that is thicker in the fornix and thinner at the limbus. [6]
Associated with the conjunctiva are specialized cellular components: [2, 6, 7]
-
Goblet cells - Secretory cells that produce mucin, a crucial component of the tear film. Mucus secretion from these cells is vital for maintaining epithelial integrity and supporting the tear film. They are more numerous in the inferior and medial portions of the bulbar conjunctiva and in the fornix.
-
Melanocytes - Pigment-producing cells found in the basal layer of the epithelium
-
Langerhans cells - Antigen-presenting cells, important for immune responses
-
Lymphocytes - Part of the conjunctiva-associated lymphoid tissue (CALT), contributing to ocular surface defense
The conjunctiva also bears eccrine glands: the conjunctival glands (of Krause) and the accessory lacrimal glands (of Wolfring). The conjunctival glands (of Krause) are concentrated in the upper fornix, whereas the accessory lacrimal glands (of Wolfring) are associated with the tarsus.
The conjunctiva serves several important functions: [2, 7]
-
Allows smooth movement of the eyelids over the eyeball
-
Keeps the ocular surface moist
-
Protects the eye from external injuries
-
Contains blood vessels that supply oxygen and nutrients to the ocular surface
-
Plays a role in the immune defense of the eye
Studies highlight the conjunctiva's lymphoid layer, also known as CALT, which includes T and B lymphocytes, resembling mucosal-associated lymphoid tissue found in other areas, such as the gut and bronchi. In this layer, Langerhans cells, specialized antigen-presenting immune cells, are distributed, especially in the tarsal conjunctiva, decreasing in number with aging. [7, 8, 9]
The fibrous layer, located beneath the lymphoid layer, houses the blood vessels, nerves, and accessory lacrimal glands of the conjunctiva, including the glands of Krause and Wolfring. The glands of Krause, concentrated in the upper fornix, and Wolfring, associated with the tarsus, contribute to tear secretion, complementing the main lacrimal gland's function. These glands are essential in sustaining ocular moisture, with their structures resembling primary lacrimal glands. [10]
Additionally, melanocytes are frequently seen in the conjunctival limbus and plica semilunaris, and they can give the conjunctiva a brownish tint in some individuals. [11]
Lacrimal Gland and the Nasolacrimal System
The lacrimal gland is an exocrine gland nestled within the fossa of the frontal bone located in the anterior superotemporal quadrant of the orbit. The lacrimal gland is composed of acini, myoepithelial cells, and intralobular and interlobular ducts. It produces the aqueous component of tears, which contains water, electrolytes, and proteins. [12]
The gland is divided into the orbital lobe and the palpebral lobe by the tendon of the levator palpebrae superioris. Ducts from both lobes traverse through the palpebral lobe and empty into the conjunctival fornix temporally.
The nasolacrimal system consists of the following structures: [2]
-
Lacrimal puncta - Two small openings located on the medial aspect of each eyelid margin
-
Lacrimal canaliculi - Two narrow canals that extend from the puncta; they have a vertical segment and a horizontal segment
-
Common canaliculus - Formed by the union of the upper and lower canaliculi
-
Lacrimal sac - A dilated structure located in the lacrimal fossa; it's divided into a fundus superiorly and a body inferiorly
-
Nasolacrimal duct - Extends from the lacrimal sac to the inferior nasal meatus
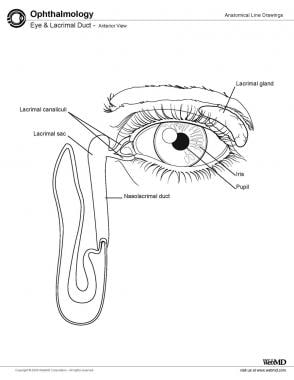
See the following image.
The drainage of tears involves several structures starting with the lacrimal puncta, tiny openings near the inner edges of the eyelids, through which tears enter the canaliculi. From the canaliculi, tears pass into the lacrimal sac at the medial canthus before moving through the nasolacrimal duct to the inferior meatus of the nasal cavity. A key structure in tear drainage is the valve of Hasner, located at the end of the nasolacrimal duct, which prevents the backflow of air and fluid into the tear drainage system from the nasal cavity. [2, 13]
Tears from the lacrimal gland provide essential moisture, nutrients, and immune protection to the eye surface. They mix with secretions from the meibomian glands and goblet cells to form the tear film, a three-layer structure essential for smooth vision and ocular comfort. The tear film, consisting of the lipid, aqueous, and mucin layers, spreads across the ocular surface during blinking, protecting the cornea from environmental irritants and infections. [14]
Studies highlight that the lacrimal gland contains stem/progenitor cells that can potentially regenerate damaged tissue, offering possibilities for treating dry eye disease. The nasolacrimal system is now recognized to have an important immunological function, containing lacrimal drainage-associated lymphoid tissue (LDALT) that plays a role in ocular surface defense. [15, 16]
Blood supply to the lacrimal gland and the nasolacrimal system primarily comes from the lacrimal artery, a branch of the ophthalmic artery, while additional supply to the nasolacrimal duct comes from the facial artery. The lacrimal gland receives both parasympathetic innervation, which drives tear secretion, and sympathetic innervation in response to emotional or physical stimuli. The sensory innervation of the lacrimal gland is through the lacrimal nerve (a branch of the ophthalmic nerve). The lacrimal apparatus also has lymphatic connections to the preauricular and submandibular lymph nodes, crucial for immune defense and fluid balance within the ocular structures. [2, 17]
Eyelids
The eyelids are designed to protect, nourish, and sustain the cornea and the anterior sclera. Anatomically, the eyelid is divided into two lamellae, anterior and posterior, demarcated by the gray line, which represents the muscle of Riolan, an extension of the orbicularis oculi muscle.
The anterior lamella is composed of the epithelium and orbicularis oculi. This muscle has a palpebral segment, further subdivided into pretarsal and preseptal regions, both contributing to eyelid movement and tear distribution. [2, 18]
The orbicularis oculi muscle has a dual role, as it includes both voluntary fibers for forced eyelid closure and involuntary fibers responsible for the blink reflex. The lacrimal part (pars lacrimalis) of this muscle, known as Horner’s muscle, attaches near the lacrimal crest, aiding in tear drainage through a pumping action. [2, 18]
The orbital septum, an extension of the periosteum, acts as a barrier that prevents the spread of infection between the anterior lamella (superficial structures) and the orbit. The septum helps differentiate between preseptal and orbital infections, which have different clinical implications and treatments. [2, 18]
The posterior lamella is primarily composed of the tarsus and palpebral conjunctiva. The tarsus is a dense connective tissue structure supporting the eyelid's shape and housing meibomian glands. These glands secrete oils critical for tear film stability and preventing tear evaporation. Meibomian gland orifices open along the eyelid margin just posterior to the gray line, ensuring an oily tear layer across the eye. [2, 18]
-
Orbicularis oculi - Main protractor (closure) muscle
-
Levator palpebrae superioris - Main retractor of upper eyelid
-
Muller's muscle - Accessory retractor
-
Sensory - Ophthalmic (V1) and maxillary (V2) branches of trigeminal nerve
-
Motor - Facial nerve (CN VII) for orbicularis, oculomotor nerve (CN III) for levator
Intraocular Structures
Tunica Fibrosa
Sclera
The sclera is a dense, fibrous tissue that forms the outermost layer of the eye (see the image below). It protects the eyes and provides for extraocular muscle insertion. Posteriorly, the sclera is perforated by the optic nerve at the lamina cribrosa. The peripapillary sclera (PPS) surrounding the optic nerve head has been identified as a critical biomechanical structure, with its properties potentially influencing glaucoma susceptibility. [21]
Scleral thickness is not uniform. Anteriorly, the sclera is 0.6 mm thick, 0.3 mm thick at the insertion of the rectus muscles, 0.5 mm thick at the equator, and 1.0 mm thick at the posterior pole.
Externally, the sclera is covered by the episclera, containing episcleral vessels, and the anterior and posterior plexus.
The sclera is understood to have a complex, hierarchical structure composed of collagen fibrils organized into lamellae. These lamellae demonstrate more branching and interweaving compared to the cornea, varying with tissue depth and anatomical location. Scleral composition includes approximately 68% water, 28% collagens, and smaller amounts of proteoglycans, elastin, and other proteins. Imaging techniques have revealed that scleral collagen fiber organization varies regionally, likely adapting to local mechanical stresses. Studies have highlighted the importance of scleral biomechanics in myopia development and progression. [21]
Cornea
The cornea is a clear and transparent layer anterior to the eye. It is the eye's main refracting surface. This layer is avascular and exhibits the following five layers:
- The epithelium is a stratified squamous nonkeratinized epithelium (5-6 layers of cells); it is highly sensitive due to numerous nerve endings and has excellent regenerative power. The corneal epithelium plays a crucial role in maintaining corneal homeostasis through the production of various growth factors and cytokines. Research has highlighted the importance of limbal stem cells, located at the corneal-scleral junction, in maintaining the corneal epithelium. [22, 23]
- The Bowman membrane is structureless and acellular. It separates the epithelium from the stroma. [2]
- The substantia propria (stroma) forms 90% of the cornea's thickness; fibrils of the stroma criss-cross at 90° angles, and these fibrils are of types I, III, V, and VII collagen.
- The Descemet membrane is structureless, homogeneous, and measures 3-12 microns; it is composed of the anterior banded zone and the posterior nonbanded zone; the Descemet membrane is rich in type IV collagen fibers.
The endothelium is a single layer of simple cuboidal and hexagonal cells that line the inner surface of the cornea. The endothelium is derived from the neural crest and functions to transport fluid from the anterior chamber to the stroma. Because the cornea is avascular, its nutrients are derived mainly from diffusion from the endothelium layer. Imaging techniques, such as in vivo confocal microscopy, have allowed for better visualization and quantification of corneal nerves, revealing their importance in corneal sensation and wound healing. Studies have focused on the corneal nerves' role in maintaining corneal health, with new surgical techniques such as corneal neurotization being developed to address neurotrophic keratopathy. [24, 25]
Tunica vasculosa (uveal tract)
Choroid
The choroid is a spongy, brown membrane with extensive venous plexuses, which has the following four layers:
- The epichoroid layer bridges the space between the sclera and choroid. It contains collagen fibers, melanocytes, and nerve fibers. [26]
- The vessels layer forms the bulk of the choroid layer and contains melanocytes, blood vessels, and connective tissue. It provides structural integrity and pigmentation. [26]
- The choriocapillaris is a layer of capillaries lined by fenestrated type II endothelium that supplies nutrition to the outer portion of the retina.
- The Bruch membrane is a shiny, homogeneous membrane that lies between the choriocapillaris and retina. It ensures selective permeability for waste removal and nutrient exchange. [26]
The choroid plays a crucial role in supplying oxygen and nutrients to the outer retinal layers and regulating ocular temperature. [26]
Ciliary body
The ciliary body is a ring-shaped structure located between the choroid and iris. [27] The ciliary body is the thickest part of the tunica vasculosa. It encircles the eye, anterior to the ora serrata. The ciliary processes are radiating folds of smooth muscles. The bulk of the ciliary body is made up of smooth muscle arranged in meridional, radial, and equatorial bands. They function to contract and relax the zonule fibers, which results in altered tension on the capsule of the lens.
The ciliary body is divided into two regions: [27, 28]
-
Pars plicata - The anterior, folded portion containing the ciliary processes
-
Pars plana - The posterior, flatter region transitioning to the retina
Functions of the ciliary body include: [27, 28]
-
Aqueous humor production
-
Accommodation
-
Supporting the lens via zonular fibers
-
Contributing to uveoscleral outflow
Iris
The iris is the most anterior part of the uvea. It has a central aperture, the pupil. Peripherally, the iris is attached to the ciliary body, and anteriorly, it rests against the anterior surface of the lens, thus separating the anterior chamber from the posterior chamber. The anterior surface is irregular with crypts and furrows; posteriorly, the surface shows shallow furrows and is uniformly black due to the two layers of pigmented epithelium.
The iris has both a sphincter and a dilator pupillary muscle. The sphincter pupillae muscle lies as a ring of smooth muscle at the pupillary margin and is supplied by the parasympathetic fibers of CN III. The dilator pupillae muscle is thin and radially oriented; it is supplied by the sympathetic fibers.
Lens
The lens is a crystalline structure, biconvex, and covered by a lens capsule. Attached to it are the zonular fibers that pass to the ciliary body as the suspensory ligament. The lens is avascular and derives its nutrients from the aqueous humor. It is elastic and transparent and held in place by suspensory ligament or zonule.
The lens continues to grow throughout life, with new fiber cells being added to its outer layers. This growth process is tightly regulated to maintain optical clarity. The lens is composed of three main parts: the capsule, the epithelium, and the fiber cells. The fiber cells make up the bulk of the lens and are arranged in concentric layers. Imaging techniques have shown that the human lens has a gradient refractive index, with the highest index at the center. This gradient contributes significantly to the lens's optical power. [29]
Research has revealed that the lens contains its own circadian clock machinery, which may play a role in regulating lens homeostasis and growth. [30]
Chambers of the Eye
The anterior chamber is a space bounded anteriorly by the posterior surface (endothelium) of the cornea and posteriorly by the lens, iris, and anterior surface of the ciliary body. Circumferentially, the lateral border of the anterior chamber is occupied by the trabecular meshwork, through which aqueous humor is drained into the scleral venous sinus (canal of Schlemm).
The posterior chamber is bounded anteriorly by the iris, posteriorly by the lens and zonule fibers, and peripherally by the ciliary processes.
Aqueous Humor
The aqueous humor is a watery fluid that fills both the anterior and posterior chambers of the eye. It is secreted partially by the ciliary epithelium and partially by diffusion from the capillaries in the ciliary processes. The aqueous humor contains diffusible materials from the blood plasma but has a low protein content.
The aqueous humor contains various growth factors and cytokines that play crucial roles in maintaining ocular health. Outflow pathways for aqueous humor include the trabecular outflow, uveoscleral, and lymphatic routes. [31, 32]
Scleral Venous Sinus (Canal of Schlemm)
The scleral venous sinus, or canal of Schlemm, is an annular vessel encircling the eye. The canal is lined by endothelium and its function is to drain the aqueous humor.
Trabecular Meshwork
The trabecular meshwork is a spongelike tissue that is interposed between the anterior chamber and the scleral venous sinus. The trabeculae are made up of a core of collagenous fibers that are covered by endothelium.
Vitreous Body
The vitreous body is a clear, transparent gel that fills the space between the retina and the lens that adheres to the retina. Its function is to maintain the shape and turgidity of the eye and to permit the passage of light rays to the retina.
Refractive Media
Refractive media include all transparent structures through which light rays must pass to reach the retina, such as the cornea, anterior chamber, lens, and vitreous body.
Retina
The retina is the innermost layer of the eyeball, which is composed of photoreceptor cells. In the posterior pole, a shallow depression is termed the fovea centralis (see the following image). This area is the point of greatest visual acuity. This area is composed of only cones. Around the fovea is an area containing yellow pigment termed the macula lutea.
The layers of the retina are as follows:
-
Pigment epithelium (the layer closest to the choroid layer)
-
Layer of rods and cones
-
External limiting membrane
-
Outer nuclear layer
-
Outer plexiform layer
-
Inner nuclear layer
-
Inner plexiform layer
-
Ganglion cell layer
-
Optic nerve fiber layer
-
Internal limiting membrane (the layer closest to the vitreous body)
Pigment epithelium
The pigment epithelium is a single layer of polygonal cells regular in shape. The nuclei are spherical and lie toward the cell base. Numerous melanin granules are seen. Functionally, the pigment epithelium absorbs light and prevents reflection, and it is also involved in the nutrition of photoreceptors. The pigment epithelium is essential for the formation of rhodopsin and its movement by storing and releasing vitamin A, a rhodopsin precursor.
Layer of rods and cones
Rods are slender, cylindrical cells and number about 130 x 106. Cones have a flask shape and number about 67 x 106. Nuclei of the cones are larger than those of the rods, and they are also less dense. They do not contain rhodopsin but have a pigment that is sensitive to blue, green, and red light. The fovea, located in the central retina, is known to contain about 200,000 cones per sq mm, providing high visual acuity. [33]
External and internal limiting membrane
The external limiting membrane supports the photoreceptor cells. The internal limiting membrane is the basal lamina of the Muller cells, separating the retina from the vitreous body. Muller glia cells have been found to act as optical fibers, guiding light through the retina to photoreceptors. [34]
Outer and inner nuclear layers
The outer nuclear layer is composed of the nucleated portion of the rod and cone cells. The inner nuclear layer contains the cell bodies and nuclei of the bipolar neurons as well as supporting cells named Muller cells.
Outer and inner plexiform layers
The outer plexiform layer contains synapses made between the rod and cone cells and the bipolar cells. The inner plexiform layer contains the synapses between the bipolar neurons and the ganglionic cells.
Ganglion cell layer
The ganglion cell layer contains cell bodies and nuclei of the ganglion cells. Neuroglia are also present.
Optic nerve fibers
The optic nerve fibers contain axons of the ganglion cells that pass radially to form the optic nerve.
-
Eye, sagittal section.
-
Eye, fundoscopic view.
-
Eye and lacrimal duct, anterior view.