ACRONYMS
Ara-C - cytosine arabinoside
CNS - central nervous system
FAF - fundus autofluorescence
FFA - fundus fluorescein angiography
ICGA- indocyanine green angiography
IOL - intraocular lymphoma
MTX - methotrexate
OCT - optical coherence tomography
PCNSL - primary CNS lymphoma
PCNSLO - primary CNS lymphoma with ocular involvement
PIOL - primary intraocular lymphoma
PVRL - primary vitreoretinal lymphoma
SIOL - secondary intraocular lymphoma
Overview
Whereas Hodgkin lymphoma rarely causes ocular disease, non-Hodgkin lymphoma (NHL) is the most common type of ocular lymphoma. Depending on the site of involvement, ocular lymphoma can be intraocular, and adnexal. [1]
Intraocular
Intraocular lymphoma (IOL) is a rare lymphocytic malignancy. It may be either a primary intraocular lymphoma (PIOL) or a secondary intraocular lymphoma (SIOL). PIOL is mainly a subtype of primary CNS lymphoma (PCNSL). SIOL results from ocular metastasis originating from outside the CNS. The most common presentation of intraocular lymphoma is decreased vision with non-resolving uveitis. Diagnosis often is based on obtaining an intraocular biopsy specimen. Optimal management is not yet realized. Chemoradiation is the most effective treatment, but its use is associated with significant ocular and cerebral morbidity.
Orbital
Lymphoma has been described as the most common malignant orbital tumor, representing 55% of cases in adults [2] and 10% of cases in older patients. [3, 4] Lymphoproliferative disease of the orbit usually presents later in life and causes symptoms due to gradually increasing mass effect. Proptosis and visible conjunctival mass are the common modes of presentation. It tends to be localized to the orbit at the time of diagnosis and responds well to local or systemic therapy. [5]
Adnexal
Orbital and adnexal lymphoma is associated with systemic lymphoma in 30-35% of cases. Hence, all patients with ocular lymphoma should have a complete workup to rule out systemic lymphoma. [6]
Classification
Over the years, different systems have been used to classify lymphomas, including the Rappaport Classification (used until the 1970s), the Working Formulation, the National Cancer Institute Working Formulation, and the Revised European-American Lymphoma Classification (REAL). In 2001, a modern comprehensive classification system was published under the auspices of the World Health Organization (WHO); this represents the first worldwide consensus document on lymphoma classification. [7]
Prognosis
The prognosis for ocular lymphoma depends on the tumor’s histologic type and stage and the treatment employed. In general, with modern treatment of patients with NHL, the overall survival rate at 5 years is approximately 60%.
Epidemiology
According to the American Cancer Society, in 2022 there were approximately 3,360 new cancers (primarily melanomas) of the eye and orbit; 1,790 occured in men and 1,570 occured in women. Approximately 410 individuals (220 men and 190 women) died from cancers of the eye and orbit. [8, 9]
The lifetime risk of being diagnosed with non-Hodgkin lymphoma (NHL) is 2.08%. From 1975-2001, a rapid and steady increase occurred in the incidence of ocular NHL, with annual increases of 6.2% and 6.5% among White males and White females, respectively. [10]
The incidence of lymphoproliferative ocular diseases, especially malignant lymphoma, has increased over the years. Lymphoma is the most common primary malignant orbital tumor in Asian countries like Japan and Korea, [11, 12, 13] as well as in Europe. [14]
Intraocular lymphoma is rare, with fewer than 200 cases being reported. This type of lymphoma represents 1% of NHLs, 1% of intracranial tumors, and less than 1% of intraocular tumors. [15] However, over the past 20 years, a steady rise has occurred in the number of reported cases [16] in both immunocompetent patients and immunocompromised patients. [17]
The incidence of ocular lymphoma increases with advancing age. [10] Intraocular lymphoma typically affects elderly patients, with reported series having mean ages in the seventh decade of life. The median age at presentation for orbital and adnexal lymphoma is older than 60 years. In a study conducted in the United States, malignant lymphoma was the most common orbital tumor in the elderly, accounting for 24% of cases. [18]
No sex predilection was noted for ocular lymphomas in some studies. [10] However, in cases of intraocular lymphoma, women are affected twice as often as men. Orbital lymphoma was found to have a female preponderance. [5] During 1992–2001, ocular NHL rates per 100,000 person-years for both sexes were highest among Asians/Pacific Islanders, lower in Whites, and much lower in Blacks. [10]
Pathophysiology
Molecular studies demonstrating viral DNA in the ocular lymphoma cells suggest a role for infectious agents in the pathogenesis of intraocular lymphoma. Infectious agents cause lymphocyte proliferation which later turns into clonal proliferation.
Epstein-Barr virus (EBV) infection of the B lymphocytes results in uncontrolled proliferation of the lymphocytes in the absence of T- suppressor lymphocytes in immunodeficiency states such as AIDS (acquired immunodeficiency syndrome). Toxoplasma gondii DNA has been detected in B cell lymphoma cells of PIOL.
Chlamydia psittaci is associated with ocular adnexal mucosa-associated lymphoid tissue (MALT) lymphoma, and this association varies across different geographical areas. [10, 19] In South Florida, orbital and adnexal lymphomas are not associated with C psittaci infections. [20]
Extramarginal zone lymphomas, which account for most primary orbital and adnexal lymphomas, are characterized by an indolent natural history with frequent, continuous extranodal relapses. [20] Follicular lymphoma, diffuse large B cell lymphoma, mantle cell lymphoma, B-cell chronic lymphocytic leukemia, peripheral T-cell lymphoma, and natural killer cell lymphoma also have been reported to affect the orbit.
Several hypotheses explain the increasing incidence of non-Hodgkin lymphoma (NHL). Better imaging techniques, improved biopsy techniques, and newer classification systems likely have contributed to the apparent increase in the incidence of lymphoma. The aging population, the increasing number of immunosuppressive drugs, and the AIDS epidemic also have contributed to the increased incidence of NHL.
Clinical Presentation
The reported symptoms differ according to whether the lymphoma is intraocular, orbital, or adnexal.
Intraocular lymphoma
There are two distinct forms of intraocular lymphoma. When the ocular disease appears to be a subset of primary central nervous system (CNS) lymphoma (PCNSL), the term “primary CNS lymphoma with ocular involvement” (PCNSLO) is used. In these cases, intraocular lymphoma can precede CNS involvement for months or years. The second form of intraocular lymphoma arises outside the CNS and metastasizes to the eye.
Intraocular lymphoma has been divided anatomically into vitreoretinal and uveal forms. The vitreoretinal form is associated with PCNSL and is typically a large B-cell tumor (intermediate-grade lymphoma). In contrast, the uveal form is associated with systemic NHL and the involvement of orbital structures. It typically is small B-cell proliferation (low-grade lymphoma) and usually occurs with advanced systemic disease. Rare cases of T-cell lymphoma with ocular involvement have been reported.
On initial presentation, PCNSLO may be either unilateral or bilateral, but ultimately, 80-90% of patients have bilateral involvement. The intracranial disease occurs in 56-85% of patients with ocular disease, and estimates suggest that 15-25% of patients who present with CNS disease have the ocular disease—hence the distinction between PCNSL and PCNSLO. [21, 22, 23, 24, 25]
The typical clinical profile is an elderly patient with uveitis refractory to treatment. The most common subjective symptoms are painless decreased vision, photophobia, red eye, and floaters. Because of its insidious onset and ability to simulate other conditions, delay in diagnosis is common. In some patients with known PCNSL, the ocular disease may be discovered on routine screening.
Vision loss is frequent in PCNSLO and may range from mild to severe. With extensive disease, circulating tumor cells can appear in the anterior chamber in as many as 75% of patients. The cells simulate iridocyclitis and can even form a pseudohypopyon. Secondary anterior segment changes include neovascularization of the iris and iridocorneal angle with possible glaucoma. In rare circumstances, PCNSLO can form a mass in the iris or angle.
In the posterior segment, vitreous cells are a typical finding and are present in most cases. The characteristic fundus lesion is a low-lying, yellow-to-white mass deep in the sensory retina. Lesions may be single or multiple, confluent or discrete. They may even appear as multiple punctate lesions.
Lesions may be infiltrative and involve all layers of the retina. Retinal hemorrhage rarely is seen. The deep location of the infiltrates can give rise to exudative retinal detachment. If chorioretinal lesions regress, scarring and atrophy of the retinal pigment epithelium may be the only remaining fundus findings. Optic neuropathy also may be a feature. [21, 22, 23, 24, 25]
PCNSLO appears to occur with increased frequency in severely immunosuppressed persons.
Metastatic systemic lymphoma, like other metastatic ocular tumors, usually is confined to the uvea—particularly the choroid. Compared with PCNSLO, metastatic systemic lymphomas are much less prevalent, have a better prognosis, and are less likely to create a diagnostic dilemma. [26]
Orbital and adnexal lymphoma
Orbital and ocular adnexal lymphoma has an insidious onset and can progress slowly for over a year before producing symptoms. Symptoms usually are secondary to pressure effects on surrounding structures. Clinical features include painless proptosis with or without motility disturbances, double vision, ptosis, and, rarely, decreased vision. The lesions can be unilateral or bilateral. Lymphomatous lesions can involve the preseptal portion of the eyelid.
Orbital lymphomas present with painless proptosis, the lesions being more common in the superior anterior orbit. The mass usually is rubbery to firm on palpation with no palpable bony destruction. The lacrimal gland, lacrimal sac, and extraocular muscles also can be similarly involved.
Orbital lymphoma also can occur in patients with AIDS. [27, 28]
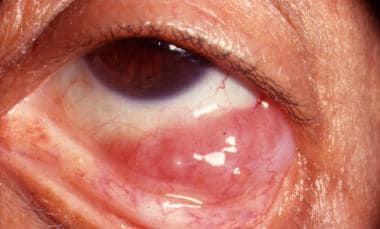
Conjunctival lymphoma has a characteristic salmon-pink appearance (see the image below). It may be an extension of orbital or intraocular lymphoma.
Simultaneous occurrence of intraocular and orbital lymphoma does occur but is rare. [29]
The presence of cervical or preauricular lymphadenopathy, parotid gland swelling, or an abdominal mass can signify systemic disease. Hence, a thorough physical evaluation should be carried out in all patients with ocular lymphoma.
Differential Diagnosis
The differential diagnosis for primary central nervous system lymphoma with ocular involvement (PCNSLO) includes reactive lymphoid hyperplasia (RLH), the spread of systemic lymphoma, primary uveitis, infection, metastatic tumor, and amelanotic melanoma. All of these (except uveal melanoma) may not uncommonly have central nervous system (CNS) involvement.
Primarily vitreoretinal involvement supports the diagnosis of PCNSLO, whereas choroidal involvement and evidence of other non-Hodgkin lymphoma (NHL) support metastatic spread to the choroid. Large cell intraocular lymphoma with retinal involvement can mimic cytomegalovirus retinitis.
Conjunctival lymphoma should be included in the differential diagnoses of chronic conjunctivitis. Persisting signs and symptoms of conjunctivitis not responding to standard treatment should prompt a biopsy. [30]
The differential diagnosis for orbital lymphoma includes idiopathic inflammatory pseudotumor, orbital lymphoid hyperplasia, orbital sarcoidosis, Wegener granulomatosis, and chronic dacryoadenitis.
Laboratory Studies
Laboratory studies are required to address the differential diagnosis of primary central nervous system lymphoma with ocular involvement (PCNSLO) and orbital lymphoma. They include the following:
-
Complete blood count (CBC) with differential
-
Serum immunoprotein electrophoresis
-
Rapid plasma reagin (RPR) screening
-
Erythrocyte sedimentation rate (ESR)
-
Fluorescent treponemal antibody absorption (FTA-Abs) test
-
Toxoplasma titers
-
Antinuclear antibodies (ANA) test
-
Rheumatoid factor
-
Angiotensin-converting enzyme (ACE)
-
Cytomegalovirus (CMV) titers
A tuberculosis skin test is advisable. The serum lactate dehydrogenase (LDH) level is a prognostic indicator, with higher levels indicative of a poorer prognosis. Enzyme-linked immunosorbent assay (ELISA) for HIV also is recommended.
Imaging Studies
Intraocular lymphoma
B-scan ultrasonography can show the presence of vitreous echoes and elevated chorioretinal lesions. In addition, retinal detachment may be seen.
Optical coherence tomography (OCT) helps demonstrate or analyze lesions at the posterior pole, provided the ocular media isn't too hazy due to vitreous involvement. Findings include nodular hyperreflective lesions in the retinal pigment epithelial layer corresponding to subretinal and sub-retinal pigment epithelium (RPE) lymphoma deposits and the absence of cystoid macular edema.
Fundus Fluorescein angiography (FFA) findings include small hypofluorescent lesions in the early and late phases corresponding to infiltrates masking the choroidal fluorescence, with late staining at the level of RPE, and punctate hyperfluorescent window defects, vasculitis, and very rarely petaloid leak at the macula.
Computed tomography (CT) and magnetic resonance imaging (MRI) has a low sensitivity for intraocular lymphoma and do not facilitate differentiating the diagnosis against uveitis or ocular melanoma. [31] Evaluation of patients with intraocular lymphoma includes high-resolution neuroradiologic imaging of the central nervous system (CNS) with contrast to look for lesions elsewhere.
Orbital and adnexal lymphoma
CT scans and MRIs have made it possible to make a strong presumptive diagnosis of orbital lymphoid tumors. They are more reliable than B-scan ultrasonography in the diagnosis of orbital lymphoma. Positron emission tomography (PET) is helpful in selected settings as well.
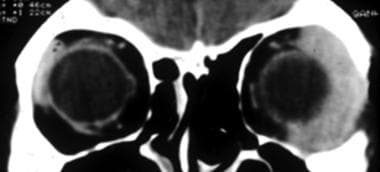
CT scan of the orbits is a sensitive investigation that facilitates the diagnosis of orbital and adnexal lymphoma. On CT scans of the orbits, orbital lymphomas are seen as well-defined, lobulated, or nodular, homogeneous masses of relatively high density and sharp margins. The lesions mold themselves to preexisting structures without eroding the bone (see the image below). [32]
The following four patterns are commonly seen:
-
Anterior preseptal
-
Retro-ocular
-
Lacrimal gland involvement
-
Extension of a lymphomatous lesion
Lacrimal gland disease may involve both orbital lobes and palpebral lobes. The lesion usually is extraconal but can extend intraconally as well. The lacrimal sac [33] and extraocular muscles [34] also may be affected. A streaky appearance may be seen, representing irregular infiltration of retrobulbar fat's microfascial structure. [35] Calcification rarely is seen. Heterogeneous lesions with bony destruction are indicative of high-grade lymphomas. [36] Bilateral lesions are possible and can signify systemic disease.
MRI of the orbits possesses good soft tissue definition; however, it cannot delineate bone destruction, which can be seen in high-grade lymphomas. MRI may miss the conjunctival disease. [37]
Orbital lesions usually are hypointense [32] or isointense on T1-weighted MRI and hyperintense on T2-weighted images. Gadolinium enhancement is seen on T1-weighted images. [36] This is indicative of high cellularity.
Fluorine-18 deoxyglucose PET (FDG-PET) sometimes can find systemic extranodal lymphomatous sites that are not detected with conventional imaging studies. This ability yields valuable information in patients with ocular lymphoma, which may result in important changes in staging and patient management. [38, 39, 40] PET has been found to have a higher sensitivity than CT scan (86% vs. 72%) in detecting distant disease. [36]
Other Tests
Lumbar puncture is indicated to obtain cerebrospinal fluid (CSF) for cytology if the patient is believed to have CNS lymphoma. Bone marrow aspiration is used for staging systemic lymphomas. CT scans of the chest and abdomen rule out retroperitoneal lymphoma. Bone scans also may be done.
Biopsy
Vitreous biopsy
Vitreous biopsy remains the mainstay of diagnosis for primary central nervous system lymphoma with ocular involvement (PCNSLO). Vitreous aspiration biopsy is a safe technique whose advantage is that it best preserves the cytomorphology. Material is aspirated directly through a 25-gauge needle into a syringe.
A mechanical vitrector provides better tissue management during the procedure and allows more specimens to be obtained. However, samples are often diluted and appear to undergo some artifactitious change since malignant lymphocytes are fragile to the effects of mechanical disruption. Material may also be lost in the tubing.
Retinal biopsy
If vitreous samples do not provide diagnostic tissue in the presence of retinal lesions, retinal and chorioretinal biopsies or subretinal aspiration may be done. Either an intraocular approach or a transscleral approach can be used.
Orbital biopsy
A biopsy of the lesion is essential to confirm the diagnosis and also to help grade the lymphoma. The diffuse infiltrating nature of lymphomas may make their complete excision difficult. Also, their excellent response to irradiation obviates the need for complete excision.
The route of biopsy is chosen depending on the site of the lesion. The direct approach is possible for conjunctival and lid lesions, whereas orbitotomy is needed for lesions involving the lacrimal gland or posterior orbit. In the case of bilateral disease, only one orbit must undergo a biopsy.
Histologic Findings
A critical factor in obtaining an accurate diagnosis of intraocular lymphoma is a cytopathologist with experience in intraocular specimens.
Mucosa-associated lymphoid tissue (MALT) lymphoma, diffuse large cell lymphoma, and small lymphocytic lymphoma are common types of intraocular lymphoma. Because of the fragility of neoplastic lymphocytes, a specimen may contain numerous abnormal-appearing but uninterruptable cells.
Tumor cells can involve the vitreous, retina, optic nerve, or choroid. They are found less often in the anterior segment. Choroidal involvement by primary central nervous system lymphoma with ocular involvement (PCNSLO) typically is diffuse, whereas retinal involvement may be more perivascular. When present, retinal necrosis can be extensive.
Molecular analysis detecting immunoglobulin gene rearrangements and ocular cytokine levels showing elevated interleukin (IL)–10 (IL-10), with an IL-10–to–IL-6 ratio greater than 1.0, are helpful adjuncts to cytology for establishing the diagnosis of PCNSLO. [41] CDR3 polymorphism analysis is recommended to confirm clonality.
Extranodal marginal zone B-cell lymphoma represents the most common orbital lymphoma subtype. [42, 43] Most patients with ocular adnexal lymphoma have stage IE disease. Immunohistochemical staining with CD markers helps classify lymphomas.
Gross specimens appear salmon-colored with a fish-flesh consistency. Hypercellular proliferations are seen with sparse stroma. Immunologic identification of cell surface markers on lymphocytes can classify tumors as containing T or B cells and as monoclonal or polyclonal.
Most orbital lymphomas are of B-cell origin with monoclonal proliferation from a single neoplastic cell. Well-differentiated monoclonal lesions have been associated with systemic disease in 20% of cases, whereas the association increases to 60% with less well-differentiated lesions.
The MIB-1 proliferation rate and p53 positivity may aid in predicting disease stage and disease progression. In contrast, polymerase chain reaction (PCR) testing can support the diagnosis and reduce the number of histologically indeterminate lesions. [44]
Treatment & Management
Intraocular lymphoma
Local therapy includes intravitreal chemotherapy, radiation, and vitrectomy.
Currently used intravitreal chemotherapy includes methotrexate 0.4mg/0.1ml and rituximab 1mg/0.1ml in varying treatment schedules. Intravitreal chemotherapy is indicated (1) in unilateral and bilateral PIOL, (2) in combination with systemic chemotherapy for PVRL with CNS involvement, (3) in relapsed PIOL, and (4) in the ocular relapse of PCNSL.
Because of the high recurrence rate and refractory nature of primary central nervous system lymphoma with ocular involvement (PCNSLO), treatment is complex. [16] However, the treatment of intraocular lymphoma underwent a significant advance with the introduction of chemoradiation to the central nervous system (CNS) and ocular radiation.
Radiation (3500-4000 cGy) alone to the eyes and CNS gave high initial response rates, but patients usually succumbed to recurrent disease. With multimodality therapy, including a boosted radiation dose (5000-10,000 cGy) to the spinal cord and intrathecal methotrexate, vision can be improved, and life can be prolonged, with some patients alive at nine years after treatment. In selected cases, patients with the isolated ocular disease have been treated with ocular radiation alone, with some longer-term survivors. [45, 46, 47]
Radiotherapy for PCNSLO is highly effective, and complications generally are acceptable. Complications of radiotherapy include cataracts, dry eye, corneal ulcer, neovascular glaucoma, radiation retinopathy, and optic neuropathy. [48, 49] In the absence of a clear advantage to intravitreal chemotherapy, which involves repetitive injections and associated risks, radiotherapy may still be the most appropriate first-line treatment in most cases. [50]
Research is ongoing to determine if lower doses of local radiation are effective and still reduce associated complications.
Innovations in treatment include multiagent primary chemotherapy. This approach was designed to reduce the radiation-associated cognitive defects that can occur in up to 40% of patients older than 50. The regimen includes methotrexate and procarbazine, vincristine, thiotepa, or both vincristine and cytarabine. Complete remission has been seen for as long as 30 months. [45, 46, 51]
Orbital and adnexal lymphoma
The recommended therapy for stage IE tumors is radiotherapy, whereas disseminated disease is treated with chemotherapy. [42]
Lymphoid tumors of the conjunctiva traditionally have been treated with local radiation therapy. Some cases of conjunctival lymphoma were seen to regress after biopsy spontaneously; hence, follow-up without radiation has been considered an option for patients with mucosa-associated lymphoid tissue (MALT) lymphoma of conjunctival origin after the pathologic diagnosis by biopsy. [52, 53] Cryotherapy for certain conjunctival lymphomatous tumors has been suggested because of fewer ocular and systemic complications and lower cost. [54]
Radiotherapy alone is a highly effective modality in the curative management of solitary low-grade primary orbital lymphoma. [48, 55] Bilateral orbital disease itself is not an indication for chemotherapy in the absence of systemic disease.
Approximately 50% of orbital lymphomas are confined to the orbit at the time of diagnosis. In cases where there is no evidence of systemic lymphoma, local orbital low-dose (1500-3000 cGy) irradiation in fractionated doses is advised. High-grade tumors may require up to 4000 cGy. Appropriate shielding of the globe (lens-sparing technique) is recommended to minimize ocular complications of radiotherapy. [48]
In cases of massive orbital involvement, chemotherapy and radiation therapy can simultaneously be given.
Because secondary orbital lymphomas often exhibit widespread systemic involvement and usually have a more aggressive histologic classification than primary orbital lymphomas, treatment of these lesions with systemic chemotherapy or systemic immunotherapy is warranted. Chemotherapy, with or without radiotherapy, should be chosen for disseminated and high-grade lymphomas. [55, 56] After radiotherapy, local control was achieved in 97-100% of patients. [48, 57, 58]
Lymphomas respond well to monoclonal antibody (mAb) therapy, and research is ongoing to determine if such therapy can replace chemotherapy. Rituximab, ibritumomab, and epratuzumab are mAbs that are either already in use or being tested for use in lymphoma treatment. Intravenous rituximab has been used to treat low-grade lymphoma with good results. [59, 60]
Antiangiogenic drugs, such as thalidomide, are being researched for lymphoma treatment, as they slow cancer cell growth.
Consultations
Neurologic evaluation is required in patients with intraocular lymphoma to rule out CNS involvement. Patients with ocular lymphoma should be referred to a clinical oncologist to assess systemic lymphoma.
Further outpatient care
Despite usually demonstrating an indolent course, extranodal marginal zone B-cell lymphomas are renowned for recurrence in extranodal sites, including other ocular adnexal sites. [42] These sites can also include the lung, parotid gland, and bone marrow. [49]
Close clinical follow-up every 6 months for 2 years upon completion of treatment and annually after that is recommended. The evaluation should include neuroimaging studies (eg, ultrasonography, computed tomography [CT], or magnetic resonance imaging [MRI] of the orbits) to look for residual or recurrent local disease.
Serial imaging can be a handy tool for detecting recurrence. Residual fibrosis of involved extraocular muscles or other orbital structures can appear similar to tumors. Whether re-biopsy or exploration is indicated should be a clinical decision, often aided by serial imaging.
A clinical oncologist also should follow up with the patient for a thorough systemic evaluation every 6 months for 2 years and annually.
Prognosis
Death can occur as a result of the systemic spread of lymphoma. [5] Prior or concurrent systemic disease has been noted as the most significant predictive factor for lymphoma-related death. Still, tumor-related death also was found to be more common and earlier with bilateral disease. Tumor-related death is slightly less where symptoms have been present for more than a year and somewhat greater in the elderly.
Patients with primary central nervous system lymphoma with ocular involvement (PCNSLO) have a poor prognosis even with chemoradiation, and many succumb to central nervous system (CNS) disease within 2 years. Yet, the median survival of primary central nervous system lymphoma (PCNSL) has increased from 1-1.5 years to over 3 years with newer therapies. Features affecting the prognosis of PCNSLO are not well understood. [61] Death ensues by CNS dissemination. Ocular lymphoma may be the initial manifestation of PCNSL.
In a study of patients with ocular adnexal lymphomas, age, sex, and anatomic location of the lymphomas did not have prognostic significance during a follow-up period of 6 months to 16.5 years. [44] The primary prognostic criteria for ocular adnexal lymphomas include the anatomic location of the tumor, stage of disease at first presentation, subtype of lymphoma, immunohistochemical markers determining factors such as tumor growth rate, and the serum lactate dehydrogenase (LDH) level. [42]
The extent of the disease at the time of presentation was the most important clinical prognostic factor. Advanced disease correlated with increased risk ratios of persistent disease at the final follow-up and lymphoma-related death. [44]
The longest survival has been seen in patients with low-grade lymphomas (ie, marginal zone lymphoma, follicular lymphoma). [62] T-cell lymphomas are associated with high mortality with conventional treatment, as there is a high incidence of systemic involvement. [63]
The overall prognosis for ocular adnexal lymphoid tumors is excellent; when lumped together, 67% are not found to be associated with the systemic disease, with a mean follow-up of over 4 years. Throughout follow-up, it could be anticipated that 20-25% of patients not known to have systemic lymphoma develop evidence of disseminated disease within 5 years. [64]
Conjunctival lymphoma is known to have the lowest rate of extraorbital spread and lymphoma-related death, the rate of these two events being sequentially greater for patients with predominantly deep orbital lymphoma, lacrimal gland lymphoma, or eyelid lymphoma. [64, 65]
With radiotherapy for orbital disease, the 5-year disease-free survival, and the overall survival rate have been between 65-73.6% and 65.5-78%. [48, 57] Most relapses occur in the first 2 years after therapy. The risk of late relapse is higher in patients with divergent histology of indolent and aggressive diseases.
Intraocular lymphoma can lead to blindness due to damage to the intraocular structures. Orbital lymphoma can cause blindness in untreated or aggressive cases, with severe proptosis leading to corneal complications or optic neuropathy. Local irradiation can also cause reversible blindness due to cataracts. And irreversible blindness in cases of radiation-induced optic neuropathy and retinopathy.
Questions & Answers
Overview
What is intraocular lymphoma (IOL)?
What are orbital and adnexal lymphoma?
What is ocular lymphoma classified?
What are the survival rates for ocular lymphoma?
What is the prevalence of ocular lymphoma?
Which age group has the highest prevalence of ocular lymphoma?
What are the sexual and racial predilections of ocular lymphoma?
What is the pathophysiology of ocular lymphoma?
What are the signs and symptoms of ocular lymphoma?
What are the forms of intraocular lymphoma?
Which clinical history findings are characteristic of ocular metastatic systemic lymphoma?
Which clinical history findings are characteristic of orbital and adnexal lymphoma?
How is conjunctival lymphoma differentiated from chronic conjunctivitis?
Which conditions are included in the differential diagnoses of orbital lymphoma?
What is the role of lab tests in the workup of ocular lymphoma?
What is the role of imaging studies in the workup of intraocular lymphoma?
What is the role of imaging studies in the workup of orbital and adnexal lymphoma?
What is the role of lumbar puncture in the workup of ocular lymphoma?
What is the role of vitreous biopsy in the workup of ocular lymphoma?
What is the role of retinal biopsy in the workup of ocular lymphoma?
What is the role of orbital biopsy in the workup of ocular lymphoma?
Which histologic findings are characteristic of ocular lymphoma?
How is intraocular lymphoma treated?
How are orbital and adnexal lymphoma treated?
Which specialist consultations are beneficial to patients with ocular lymphoma?
What is included in the long-term monitoring of ocular lymphoma?
What is the prognosis of ocular lymphoma?
-
Salmon-pink appearance of conjunctival lymphoma.
-
Homogeneous isodense orbital mass molding around the lateral ocular surface.