Practice Essentials
Spondylolisthesis is a condition leading to slippage of one vertebral body over the one below, resulting in spinal stenosis and producing neurogenic claudication, with or without low back pain. [1] The word "spondylolisthesis" is derived from the Greek words spondylo, meaning spine, and listhesis, meaning to slip or slide. Spondylolisthesis has many etiologies, all of which ultimately lead to loss of stability offered by the locking mechanism of articular processes of the vertebrae that allow the superior vertebrae to slide forward over the inferior vertebrae. Etiologies can be classified as congenital (dysplastic), spondylolytic (isthmic), degenerative, traumatic, pathologic, or iatrogenic (eg, postoperative). [2] Spondylolisthesis is typically classified as isthmic or degenerative. Isthmic spondylolisthesis is classically precipitated by progressive spondylolysis, and degenerative spondylolisthesis is most commonly associated with progression of age. Degenerative spondylolisthesis is estimated to be about 6 times more common in females than in males. [3]
Prevalence of spondylolisthesis is age and gender specific. Other risk factors include a history of occupational driving, intense manual activity, and sedentary work. Diagnosis for patients with spondylolisthesis requires a detailed history, physical examination, and imaging attained through standing lateral radiography and magnetic resonance imaging (MRI). [1]
Etiologies are described below [2] :
-
Congenital spondylolisthesis occurs when a baby’s spine does not form the way it should before birth. Misaligned vertebrae put the person at risk for slippage later in life.
-
Isthmic spondylolisthesis occurs as a result of spondylolysis. A crack or a fissure weakens the bone.
-
Degenerative spondylolisthesis is the most common type and occrus with age. Over time, disks that cushion the vertebrae lose water. As disks thin, they are more likely to slip out of place. This is more common after age 50 years and is seen more often in women than in men.
-
Traumatic spondylolisthesis occurs when an injury causes vertebrae to slip.
-
Pathologic spondylolisthesis occurs because of disease such as osteoporosis or a tumor.
-
Iatrogenic (postoperative) spondylolisthesis results from spinal surgery.
The spondylolytic type is the most common form of spondylolisthesis. [4] It affects the region of the pars interarticularis, which is roughly the region of the junction of the pedicle and the lamina, where articular and transverse processes of the vertebrae arise. A defect at this point functionally separates the vertebral body, the pedicle, and the superior articular process from the inferior articular process and remaining vertebrae. Thus, the defect cleaves the vertebra into 2 parts. The portion of the vertebra posterior to the defect remains fixed, and anterior portions are free to potentially slip forward relative to posterior structures and the spine below. Note that a bilateral pars defect is needed to allow slippage.
Degenerative spondylolisthesis is a common back pathology in the general adult population. Patients with this condition may present for epidural steroid injection, epidural blood patch, or epidural analgesia. Sindhi et al concluded that patients with degenerative spondylolisthesis may be at higher risk for dural puncture due to stretching of the dura and contraction of the epidural space at the translated spinal level. [5]
Most patients with symptomatic degenerative spondylolisthesis and absence of neurologic deficits should do better with conservative treatment, whereas those with neurologic symptoms are more prone to undergo progressive functional deterioration without surgery. [1]
Imaging modalities
For diagnosis of spondylolisthesis, comprehensive evaluation with static, dynamic radiographic studies performed with the patient in a standing position and magnetic resonance imaging (MRI) are essential. Conservative treatment is first-line therapy and includes analgesics, anti-inflammatories, and physiotherapy. [6]
Flexion-extension functional radiographs are considered the gold standard for diagnosis of degenerative spondylolisthesis; a disc angle change greater than 10° or a change in translation greater than 3 mm is generally used as the cut-off. [7]
Lateral and anteroposterior plain radiographs of the lumbar spine should be obtained in patients with complaints of back pain. The lateral view (shown in the image below) is useful for detecting spondylolisthesis; it may show the pars defect.
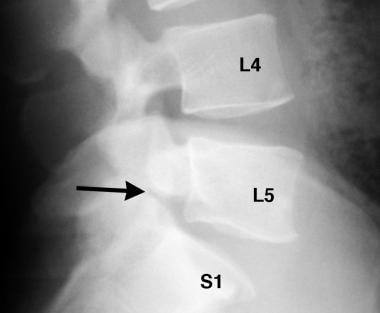 Spondylolisthesis. Straight lateral radiograph of the L4-S1 level of the spine shows lucency at the pars area (arrow). Bilateral pars defects must be present to visualize this in a lateral projection. Grade 1 spondylolisthesis is associated.
Spondylolisthesis. Straight lateral radiograph of the L4-S1 level of the spine shows lucency at the pars area (arrow). Bilateral pars defects must be present to visualize this in a lateral projection. Grade 1 spondylolisthesis is associated.
Bilateral oblique views are especially useful in visualizing the pars interarticularis defect, which has the appearance of a Scottie dog with a collar. An elongated pars also may be seen.
(See the images below.)
 Spondylolisthesis. Oblique projection radiograph shows the presence of bilateral pars defects (arrows) with an appearance resembling a Scottie dog with a collar. (The collar is the pars defect.)
Spondylolisthesis. Oblique projection radiograph shows the presence of bilateral pars defects (arrows) with an appearance resembling a Scottie dog with a collar. (The collar is the pars defect.)
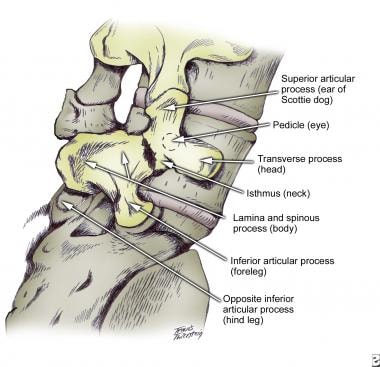 Spondylolisthesis. Diagram in the oblique projection shows components of the vertebrae that result in the appearance of a Scottie dog with a collar.
Spondylolisthesis. Diagram in the oblique projection shows components of the vertebrae that result in the appearance of a Scottie dog with a collar.
In addition, plain radiographs may show congenital types of spondylolisthesis and the changes of spondylosis. In the setting of trauma, fractures may be apparent. Note that other causes of the patient's symptoms may be identified such as osteoid osteoma, Paget disease, and osteolytic lesions. The grade of spondylolisthesis can be measured by using the lateral view (as shown in the images below).
 Spondylolisthesis. Lateral lumbar spinal radiograph in a pediatric patient shows spondylolysis with grade 1 spondylolisthesis.
Spondylolisthesis. Lateral lumbar spinal radiograph in a pediatric patient shows spondylolysis with grade 1 spondylolisthesis.
Cross-sectional imaging should be considered next.
For patients with back pain and no clinical findings of nerve root involvement, computed tomography (CT) scanning of the lumbar spine yields information regarding spondylolisthesis and its cause, along with other possible conditions, such as disc disease, disc herniation, spondylosis, and spinal canal stenosis. Other associations, such as spina bifida, may also be seen. For patients with radiculopathy, CT myelography can yield information regarding nerve root impingement and its etiology, such as disc herniation, abscess, or neoplasm. CT scanning is more sensitive for detecting spondylolysis, but occasionally this condition may be missed because scanning occurs in the plane of the spondylolysis or as the result of volume averaging. Sagittal reconstruction images are of help in patients with these findings.
MRI offers the distinct advantage of imaging the spine in any plane without exposure to radiation. Typically, axial and sagittal planes are used, but images in the coronal plane can also be acquired easily, if needed. MRI reveals spondylolisthesis on sagittal views. Spondylolysis may not be readily apparent on MRI, especially if a mild degree of bony sclerosis is evident. Other sclerotic lesions in the pars interarticularis, such as osteoblastic metastases, may present with a similar appearance. [8, 9, 10, 11]
Traumatic cervical spine fractures and dislocations are common in clinical practice, but high-grade traumatic cervical spondylolisthesis is rare. Total spondylolisthesis, or dislocation of a single cervical vertebra, can occur only with high-energy trauma, such as that seen in motor vehicle collisions, diving accidents, or severe falls. Detailed 3-dimensional (3D) reconstructive CT should be performed to evaluate fractures, subluxations, and dislocations. MRI can be used to analyze the spinal cord and ligamentous injuries, and CT angiography can reveal a vascular injury. [12]
(A grading system for spondylolisthesis is shown in the image below.)
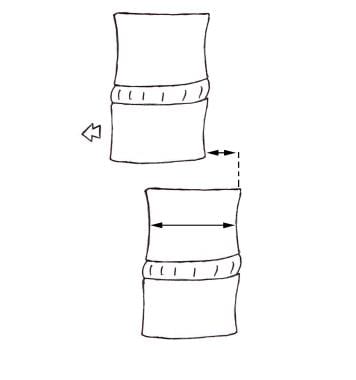 Spondylolisthesis. Diagram shows how to grade spondylolisthesis. The 2 arrows, one indicating vertebral body width and the other indicating the amount of slippage that has occurred, represent the measurements needed. The ratio of amount of slippage to vertebral body width is obtained as a percentage. Grade 1 is a ratio of 0 to 25%, grade 2 is 25% to 50%, grade 3 is 50% to 75%, and grade 4 is 75% to 100%.
Spondylolisthesis. Diagram shows how to grade spondylolisthesis. The 2 arrows, one indicating vertebral body width and the other indicating the amount of slippage that has occurred, represent the measurements needed. The ratio of amount of slippage to vertebral body width is obtained as a percentage. Grade 1 is a ratio of 0 to 25%, grade 2 is 25% to 50%, grade 3 is 50% to 75%, and grade 4 is 75% to 100%.
Meyerding grading scale
The most common grading scale for spondylolisthesis was proposed by Meyerding and describes the degree of vertebral slippage, as follows [3, 13] :
-
Grade I is < 25% slippage.
-
Grade II is 25-50% slippage.
-
Grade III is 50-75% slippage.
-
Grade IV is 75-100% slippage.
-
Grade V is complete slippage.
Radiography
For patients with complaints of back pain, anteroposterior and lateral projection plain radiographs of the lumbar spine should be obtained, at the least. [11, 14, 15]
The lateral view is especially useful in detecting spondylolisthesis. Moreover, the grade of spondylolisthesis is measured on the lateral view (as shown in the images below). The pars defect may or may not be visualized on the lateral view.
 Spondylolisthesis. Lateral lumbar spinal radiograph in a pediatric patient shows spondylolysis with grade 1 spondylolisthesis.
Spondylolisthesis. Lateral lumbar spinal radiograph in a pediatric patient shows spondylolysis with grade 1 spondylolisthesis.
Bilateral oblique views may be obtained to visualize the pars defect, which has the appearance of a Scottie dog with a collar (as shown in the radiographs below). An elongated pars may also be seen. Note that oblique views increase specificity, but not sensitivity, for pars defects. [16]
 Spondylolisthesis. Oblique projection radiograph shows the presence of bilateral pars defects (arrows) with an appearance resembling a Scottie dog with a collar. (The collar is the pars defect.)
Spondylolisthesis. Oblique projection radiograph shows the presence of bilateral pars defects (arrows) with an appearance resembling a Scottie dog with a collar. (The collar is the pars defect.)
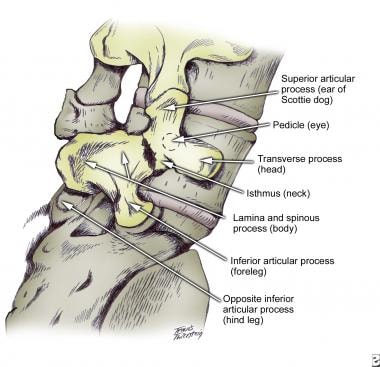 Spondylolisthesis. Diagram in the oblique projection shows components of the vertebrae that result in the appearance of a Scottie dog with a collar.
Spondylolisthesis. Diagram in the oblique projection shows components of the vertebrae that result in the appearance of a Scottie dog with a collar.
Congenital and degenerative types of spondylolisthesis also can be visualized on plain radiographs. Lumbar degenerative spondylolisthesis most commonly occurs at the L4–L5 level, followed in frequency by L3–L4, L5–S1, and L2–L3 levels. The slip occurs secondary to degenerative changes in the facet joints. A grade 1 slip is most common, followed by a grade 2 slip. The width of the lumbar canal can be directly measured on these films from the mid aspect of the vertebral body in front (anteriorly) to the dorsal (back) interlaminar line (line created by the laminae coming together to form the spinous process). Normal canal width is 20 mm. Smaller widths are considered spinal stenosis. [17]
In the setting of trauma, fractures may be apparent. Traumatic spondylolisthesis of the axis, also known as a hangman’s fracture, is caused by hyperextension of the neck. These fractures are classified according to degree of anteroposterior deviation, evidence of disruption of the posterior longitudinal ligament, position of the fracture line, and presence of a facet joint dislocation. [18]
Other causes of symptoms may be noted; these include osteoid osteoma, Paget disease, and osteolytic lesions.
In a study of lateral flexion-extension radiographs and MRI for degenerative cervical spondylolisthesis by Alvarez et al, of the 77 levels of spondylolisthesis, 17 levels (22.1%) were missed on neutral radiographs, 20 levels (26.0%) were missed when flexion-extension radiographs were used alone, and 29 levels (37.7%) identified on radiograph were missed by MRI. The authors concluded that flexion-extension radiographs should not be used in place of standard anteroposterior and lateral radiographs but that they can be a useful adjunct in identifying cervical spondylolisthesis when standard AP and lateral radiographs and MRI are not able to identify the source of neck and radicular pain. [19]
Kashigar et al conducted a multicenter study to assess whether flexion-extension radiographs add value in assessment of patients with degenerative spondylolisthesis and concluded that flexion-extension radiographs may play a limited role. Patients for whom flexion-extension views were most likely to provide value were those with smaller slips (< 7 mm) with no evidence of motion on standing radiography. [20]
Bredow et al identified surgical modification of pelvic tilt and sagittal rotation as the radiologic alignment parameters that can most accurately predict long-term clinical outcomes after lumbar interbody fusion surgery. [21]
Degree of confidence
Five-view plain radiography of the spine is the standard for a plain radiographic evaluation.
Visualization of spondylolisthesis on standard radiographs, particularly lateral plain radiographs, confirms the presence of the condition. The etiology may not be readily evident, and other modalities may be needed for elucidation. CT scanning is perhaps the most valuable cross-sectional modality used to achieve this.
In the setting of trauma in a child, a pseudosubluxation of the vertebra in the cervical spine may be observed; such a finding may cause some confusion with traumatic spondylolisthesis. Clinical correlation may be helpful because focal tenderness at that level may require further evaluation clinically and/or radiologically; CT scanning may be needed.
No normal variants that mimic spondylolysis or degenerative changes have been identified.
Computed Tomography
For patients with back pain and no clinical findings of nerve root involvement, computed tomography (CT) scanning of the lumbar spine yields information regarding spondylolisthesis and its cause, along with other possible conditions, such as disc disease, disc herniation, spondylosis, and spinal canal stenosis. Other associations, such as spina bifida, also may be revealed. For patients with radiculopathy, CT myelography can provide information regarding nerve root impingement and its etiology, such as disc herniation, abscess, or neoplasm.
CT scanning of the spine can be performed with or without intrathecal contrast enhancement. Axial images are obtained in a plane parallel to disc spaces at each level imaged. Sagittal reconstruction images (shown below) are obtained by using post-acquisition processing software. Bone window (eg, 1500/300 HU) and soft tissue window (eg, 300/30 HU) settings are used.
 Spondylolisthesis. Sagittal CT reconstruction image shows the pars defect along with grade 1 spondylolisthesis (arrow).
Spondylolisthesis. Sagittal CT reconstruction image shows the pars defect along with grade 1 spondylolisthesis (arrow).
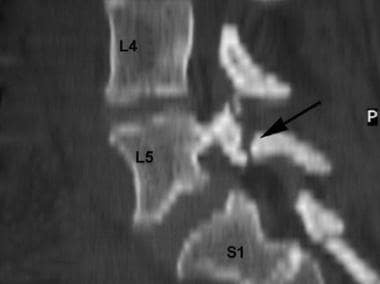 Spondylolisthesis. Sagittal CT reconstruction image shows the pars defect along with grade 1 spondylolisthesis.
Spondylolisthesis. Sagittal CT reconstruction image shows the pars defect along with grade 1 spondylolisthesis.
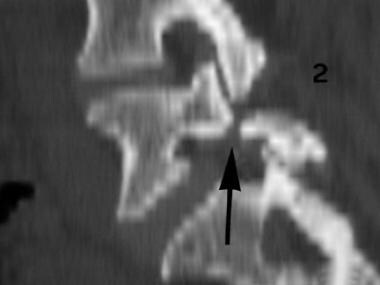 Spondylolisthesis. Sagittal CT reconstruction image shows the pars defect along with grade 1 spondylolisthesis (arrow).
Spondylolisthesis. Sagittal CT reconstruction image shows the pars defect along with grade 1 spondylolisthesis (arrow).
Thin sections should be used to avoid problems such as volume averaging. (Contiguous images also reduce such problems.) Indeed, if sections are too thick and if a gap is present between sections, spondylolysis can be missed. In such cases, sagittal reconstructions may be of help in showing spondylolysis.
With spondylolysis, CT is performed as close as possible to an angle that is 90° to the level of interest. CT scans typically reveal a horizontally oriented defect in the pars, which interrupts the normally complete bony ring of posterior elements.
Spondylolisthesis is evaluated best on lateral topography, but it can be suggested for patients with spinal stenosis in the absence of disc pathology, posterior hypertrophic changes, or a congenitally narrow spinal canal. One typically looks for an elongated spinal canal (as shown in the images below).
 Spondylolisthesis. Axial CT image shows bilateral spondylolysis (arrows). Note elongation of the spinal canal at this level.
Spondylolisthesis. Axial CT image shows bilateral spondylolysis (arrows). Note elongation of the spinal canal at this level.
 Spondylolisthesis. Axial CT image shows bilateral spondylolysis (arrows). Note elongation of the spinal canal at this level.
Spondylolisthesis. Axial CT image shows bilateral spondylolysis (arrows). Note elongation of the spinal canal at this level.
CT scans can reveal findings of congenital/dysplastic and degenerative types of spondylolisthesis. Abnormalities of vertebral body or of articular processes may be present.
Changes in spondylosis deformans (degenerative changes) are apparent on CT scans. Degenerative disease of the spine has a characteristic appearance involving loss of disc space height with or without the presence of a vacuum phenomenon, narrowing of the facet joint space, subchondral sclerosis, osteophyte formation, and subchondral cysts. Some or all of these changes may be noted and may cause altered alignment of the facet joint articular surface, leading to slippage. Spinal canal and/or intervertebral neural foraminal stenosis may be identified.
In traumatic spondylolisthesis, findings may include jumped facets and fractures of articular processes and/or laminae that result in spondylolisthesis.
Degree of confidence
Usually, CT findings confirm the presence of spondylolisthesis, its etiologies, and potential complications. MRI provides complementary imaging in some patients with traumatic spondylolisthesis for whom information regarding ligamentous and spinal cord integrity is required. One of the limitations of CT scanning is that it does not clearly show ligamentous injury.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) offers the distinct advantage of imaging the spine in any plane. Typically, axial and sagittal planes are used, but images in the coronal plane can also be acquired easily, if needed. [8, 9, 22, 23, 24]
Spin-echo and fast spin-echo sequences are applied for image acquisition in these planes. A fat saturation technique can be used to minimize signal from fat and to bring out signal from fluid structures (eg, bone edema). Gradient-echo sequences can also be used; they provide the advantage of faster image acquisition, limiting problems related to motion. For a postoperative patient, consideration should be given to gadolinium enhancement with T1-weighted spin-echo sequences.
Spondylolisthesis is confirmed by visualization on MRI. Spondylolysis may be difficult to appreciate, and plain radiographs and/or CT scans may be complementary in this regard.
Gadolinium-based contrast agents have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). This disease has occurred in patients with moderate to end-stage renal disease after they were given a gadolinium-based contrast agent to enhance MRI or magnetic resonance angiography (MRA) scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness.
MRIs should be scrutinized for the presence of a spondylolisthesis or any abnormality of the pars interarticularis, pedicles, or facet joints. Nerve structures, including those exiting neural foramina, and the spinal canal should be evaluated.
Spondylolisthesis is best assessed on median sagittal images of the spine. The levels and the grade involved can be seen.
Spondylolysis pathologically can be a fibrous bridge or a pseudarthrosis, both of which have corticated/sclerotic margins in adjacent portions of the bony ring. Bony sclerosis and fibrous tissue appear as an area of low signal intensity in the region of the pars interarticularis on images obtained with all sequences. This finding may not be easily seen, which is a limitation of using MRI for spondylolysis.
Similar signal intensity changes in these areas may be seen with bony sclerosis, volume averaging with adjacent osteoarthritic facet joints, osteoblastic metastases, and even involvement of the pedicles with Paget disease. Even if one sees normal bone signal extending from the vertebral body to the pedicle and into the lamina, it is not possible to exclude spondylolysis because minimal sclerosis may have occurred in the bone and because its signal intensity is similar to that of posterior element bone. This is a limitation of MRI in detecting spondylolysis.
High signal intensity may be seen in the pars interarticularis with T2-weighted sequences. This finding indicates the presence of fluid, a pseudarthrosis, or bone edema from infection.
Degenerative disease can also be seen. [25, 26] Narrowed disc space with disc desiccation (low T2 signal intensity) should be sought. This disc narrowing causes superoinferior subluxation of the facet joint at the level of disease, resulting in anterolisthesis or retrolisthesis. Reactive marrow changes should also be sought; these are seen in portions of vertebral body adjacent to discs and in marrow adjacent to facet joints and may result in abnormal signal intensity in the pars interarticularis.
Neoplastic disease involving the pars interarticularis or other parts of the vertebra typically yields low marrow signal intensity with all sequences. Infection may be evident as fluid signal intensity (bright on T2-weighted MRIs) from bone edema. Both disease processes show enhancement with a gadolinium-based contrast agent. Other diseases causing a sclerotic response (eg, Paget disease) result in low signal intensity with all sequences.
Nuclear Imaging
Nuclear medicine has no role as a primary imaging modality in spondylolisthesis. Spondylolysis can be detected as areas of increased activity on bone scans, but its appearance is nonspecific, and such findings may be seen in other disorders (eg, neoplasms, infections). Usually, correlation with clinical and plain radiographic findings is helpful in narrowing the differential diagnosis.
Nuclear medicine imaging involves the use of diphosphonates labeled with technetium-99m (99mTc). These are administered intravenously, and planar images of the whole body are acquired (as shown in the image below).
 Spondylolisthesis. Planar image of lumbar spine in a 14-year-old with back pain. Note hot spots at L5 in the region where one would see the pedicles end-on on a plain radiograph.
Spondylolisthesis. Planar image of lumbar spine in a 14-year-old with back pain. Note hot spots at L5 in the region where one would see the pedicles end-on on a plain radiograph.
High-count (1000 k) spot views of the lumbar spine are also obtained. Single-photon emission CT (SPECT) scanning, used to produce the images below, is a more powerful way to detect areas of increased activity that may not be readily apparent on planar images.
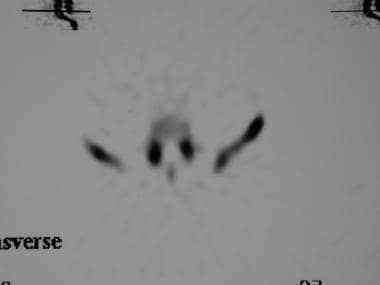 Spondylolisthesis. Axial single-photon emission CT (SPECT) image shows bilateral hot spots in the pars; these indicate spondylolysis.
Spondylolisthesis. Axial single-photon emission CT (SPECT) image shows bilateral hot spots in the pars; these indicate spondylolysis.
 Spondylolisthesis. Coronal single-photon emission CT (SPECT) image shows bilateral hot spots in the pars; these indicate active spondylolysis.
Spondylolisthesis. Coronal single-photon emission CT (SPECT) image shows bilateral hot spots in the pars; these indicate active spondylolysis.
 Spondylolisthesis. Sagittal single-photon emission CT (SPECT) image shows hot spots in the pars; these indicate active spondylolysis.
Spondylolisthesis. Sagittal single-photon emission CT (SPECT) image shows hot spots in the pars; these indicate active spondylolysis.
 Spondylolisthesis. Sagittal single-photon emission CT (SPECT) image shows hot spots in the pars; these indicate active spondylolysis.
Spondylolisthesis. Sagittal single-photon emission CT (SPECT) image shows hot spots in the pars; these indicate active spondylolysis.
 Spondylolisthesis. Sagittal single-photon emission CT (SPECT) image shows hot spots in the pars; these indicate active spondylolysis.
Spondylolisthesis. Sagittal single-photon emission CT (SPECT) image shows hot spots in the pars; these indicate active spondylolysis.
-
Spondylolisthesis. Diagram shows how to grade spondylolisthesis. The 2 arrows, one indicating vertebral body width and the other indicating the amount of slippage that has occurred, represent the measurements needed. The ratio of amount of slippage to vertebral body width is obtained as a percentage. Grade 1 is a ratio of 0 to 25%, grade 2 is 25% to 50%, grade 3 is 50% to 75%, and grade 4 is 75% to 100%.
-
Spondylolisthesis. Straight lateral radiograph of the L4-S1 level of the spine shows lucency at the pars area (arrow). Bilateral pars defects must be present to visualize this in a lateral projection. Grade 1 spondylolisthesis is associated.
-
Spondylolisthesis. Oblique projection radiograph shows the presence of bilateral pars defects (arrows) with an appearance resembling a Scottie dog with a collar. (The collar is the pars defect.)
-
Spondylolisthesis. Oblique projection radiograph shows the presence of bilateral pars defects (arrows) with an appearance resembling a Scottie dog with a collar. (The collar is the pars defect.)
-
Spondylolisthesis. Diagram in the oblique projection shows components of the vertebrae that result in the appearance of a Scottie dog with a collar.
-
Spondylolisthesis. The appearance of a Scottie dog with a collar has been outlined in the normal vertebra, with the pars defect (the collar) shown by the arrows.
-
Spondylolisthesis. Axial CT image shows bilateral spondylolysis (arrows). Note elongation of the spinal canal at this level.
-
Spondylolisthesis. Axial CT image shows bilateral spondylolysis (arrows). Note elongation of the spinal canal at this level.
-
Spondylolisthesis. Sagittal CT reconstruction image shows the pars defect along with grade 1 spondylolisthesis (arrow).
-
Spondylolisthesis. Sagittal CT reconstruction image shows the pars defect along with grade 1 spondylolisthesis.
-
Spondylolisthesis. Sagittal CT reconstruction image shows the pars defect along with grade 1 spondylolisthesis (arrow).
-
Spondylolisthesis. Lateral lumbar spinal radiograph in a pediatric patient shows spondylolysis with grade 1 spondylolisthesis.
-
Spondylolisthesis. Grade 4 traumatic spondylolisthesis.
-
Spondylolisthesis. Planar image of lumbar spine in a 14-year-old with back pain. Note hot spots at L5 in the region where one would see the pedicles end-on on a plain radiograph.
-
Spondylolisthesis. Axial single-photon emission CT (SPECT) image shows bilateral hot spots in the pars; these indicate spondylolysis.
-
Spondylolisthesis. Coronal single-photon emission CT (SPECT) image shows bilateral hot spots in the pars; these indicate active spondylolysis.
-
Spondylolisthesis. Sagittal single-photon emission CT (SPECT) image shows hot spots in the pars; these indicate active spondylolysis.
-
Spondylolisthesis. Sagittal single-photon emission CT (SPECT) image shows hot spots in the pars; these indicate active spondylolysis.
-
Spondylolisthesis. Sagittal single-photon emission CT (SPECT) image shows hot spots in the pars; these indicate active spondylolysis.
-
Spondylolisthesis. Sagittal single-photon emission CT (SPECT) image shows hot spots in the pars; these indicate active spondylolysis.