Practice Essentials
Mirizzi syndrome is an unusual presentation of obstructive jaundice caused by extrinsic compression of an extrahepatic biliary duct from one or more calculi within the cystic duct or gallbladder. It is a functional hepatic syndrome but can often present with biliary duct dilatation and can mimic other hepatobiliary pathologies such as cholangiocarcinoma.
The clinical presentation varies from no symptoms to severe cholangitis. [1] Patients may present with recurrent episodes of jaundice and cholangitis. It can be associated with acute cholecystitis. Fistulae can develop between the gallbladder and the common duct, and the stone may pass into the common duct. [2] Generally, distinguishing between Mirizzi syndrome and other causes of obstructive jaundice is not possible with physical examination alone. [3, 4]
(See images of Mirizzi syndrome below.)
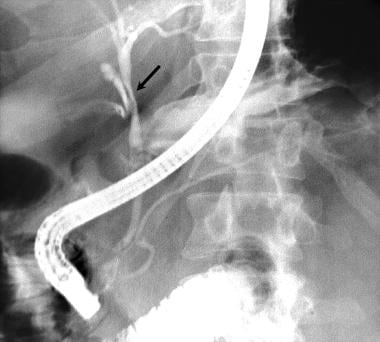 This patient presented with acute cholecystitis, as confirmed at imaging. His pain resolved over a few days, but mildly elevated bilirubin levels persisted. Image obtained during endoscopic retrograde cholangiopancreatography shows smooth narrowing of the bile duct (arrow) at the site of insertion of the cystic duct (Mirizzi syndrome). Note the small calculus in the cystic duct. Courtesy of Dr. Ali Nawaz Khan.
This patient presented with acute cholecystitis, as confirmed at imaging. His pain resolved over a few days, but mildly elevated bilirubin levels persisted. Image obtained during endoscopic retrograde cholangiopancreatography shows smooth narrowing of the bile duct (arrow) at the site of insertion of the cystic duct (Mirizzi syndrome). Note the small calculus in the cystic duct. Courtesy of Dr. Ali Nawaz Khan.
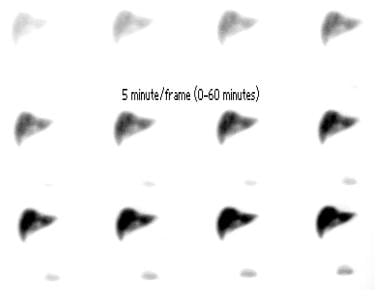 Cholescintigraphy (1-h initial images) in 61-year-old man with right upper quadrant pain for 2 days. Note the nonvisualization of gallbladder and small bowel activity. Lower activity is within the urinary bladder. Courtesy of Dr. Arthur Krasnow, Department of Radiology, Medical College of Wisconsin.
Cholescintigraphy (1-h initial images) in 61-year-old man with right upper quadrant pain for 2 days. Note the nonvisualization of gallbladder and small bowel activity. Lower activity is within the urinary bladder. Courtesy of Dr. Arthur Krasnow, Department of Radiology, Medical College of Wisconsin.
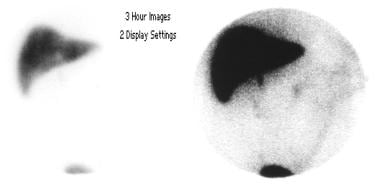 Cholescintigraphy (3-h delayed images in the anterior projection) of the same patient as in the previous image. Note persistent nonvisualization of the gallbladder and minimal activity within the small bowel. Courtesy of Dr. Arthur Krasnow, Department of Radiology, Medical College of Wisconsin.
Cholescintigraphy (3-h delayed images in the anterior projection) of the same patient as in the previous image. Note persistent nonvisualization of the gallbladder and minimal activity within the small bowel. Courtesy of Dr. Arthur Krasnow, Department of Radiology, Medical College of Wisconsin.
Classification
Although a number of classification systems have been described, such as acute vs chronic variant, anatomic variant of cystic duct vs no anatomic variant of cystic duct, and obstruction due to gallstones vs obstruction due to inflammation, the most widely used is the Csendes classification system. The Csendes system recognizes 5 major types of Mirizzi syndrome: type I is characterized by “classic” compression stenosis; types II–IV involve formation of a cholecystocholedochal fistula; and type V is defined by the formation of a cholecystoenteric fistula in addition to the presence of types I-IV (see Table 1 below).
Radiography
Generally, plain radiography is not useful in diagnosing Mirizzi syndrome. Radiographs may depict radiopaque gallstones that contain sufficient amounts of calcium.
(See the image below.)
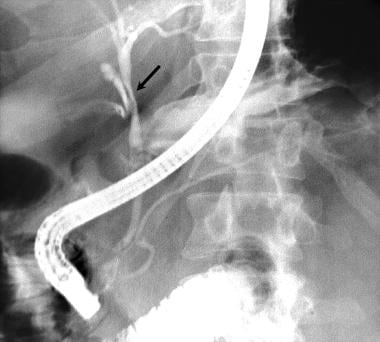 This patient presented with acute cholecystitis, as confirmed at imaging. His pain resolved over a few days, but mildly elevated bilirubin levels persisted. Image obtained during endoscopic retrograde cholangiopancreatography shows smooth narrowing of the bile duct (arrow) at the site of insertion of the cystic duct (Mirizzi syndrome). Note the small calculus in the cystic duct. Courtesy of Dr. Ali Nawaz Khan.
This patient presented with acute cholecystitis, as confirmed at imaging. His pain resolved over a few days, but mildly elevated bilirubin levels persisted. Image obtained during endoscopic retrograde cholangiopancreatography shows smooth narrowing of the bile duct (arrow) at the site of insertion of the cystic duct (Mirizzi syndrome). Note the small calculus in the cystic duct. Courtesy of Dr. Ali Nawaz Khan.
Endoscopic retrograde cholangiopancreatography (ERCP)
Potential surgical complications of a missed diagnosis obviate direct cholangiography in any patient with suspected Mirizzi syndrome after the initial evaluation with ultrasonography and/or CT. Endoscopic retrograde cholangiopancreatography (ERCP) is the criterion standard, with a mean sensitivity of 76.2%. [10] Percutaneous transhepatic cholangiography (PTC) may also be used for diagnosis, especially if ERCP findings fail to help. [9] Common signs include visible calculus in the expected position of the cystic duct, as well as smooth, lateral, and extrinsically compressed CHD. [6]
Computed Tomography
Typical diagnostic findings of Mirizzi syndrome on CT include the following [11, 12] :
-
Dilatation of the biliary system, including the CHD, distal to the level of the gallbladder neck
-
An impacted calculus in the neck of the gallbladder
-
A contracted gallbladder
-
A normal diameter of the CBD below the level of the stone.
Yun et al measured the preoperative diagnostic accuracy of magnetic resonance cholangiopancreatography (MRCP) and CT for Mirizzi syndrome and found that for combined modality (MRCP and CT), the overall sensitivity was 96% (versus 42% for CT); specificity was 93.5% (CT, 98.5%); positive predictive value was 83.5% (CT, 93%); negative predictive value was 98.5% (CT, 83.5%); and accuracy was 94% (CT, 85%). [12]
Magnetic Resonance Imaging
Typical magnetic resonance cholangiopancreatography (MRCP) findings of Mirizzi syndrome include the following [13, 14, 15, 16] :
-
An impacted stone in the gallbladder neck
-
Compression of the common hepatic duct
-
Dilatation of the biliary system above the level of impaction
-
A contracted gallbladder with wall-thickening
Additional sequences should be used to exclude the presence of malignancy.
In one report, successful preoperative diagnosis was achieved by abdominal ultrasonography in only 17% (2/12) of cases, but 83% (10/12) of cases were successfully diagnosed by MRCP. [6]
Ultrasonography
Ultrasonographic findings include the following [4, 9] :
-
An impacted calculus in the Hartmann pouch or the cystic duct
-
Dilatation of the CHD above the level of the impacted stone
-
Narrowing of the CHD at the level of impaction
-
Normal caliber of the CBD below the impaction
Nuclear Imaging
Hepatobiliary iminodiacetic acid–diisopropyl iminodiacetic acid (HIDA-DISIDA) scintigraphy may be useful in diagnosing Mirizzi syndrome. Three highly sensitive and specific signs noted are a nonvisualized gallbladder, moderate dilatation of the common hepatic duct (CHD), and delayed excretion into the duodenum.
(See the images below.)
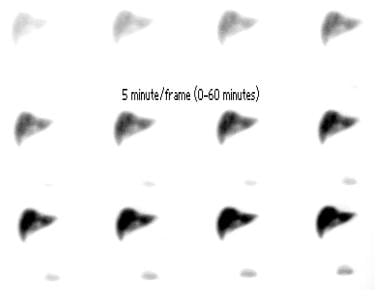 Cholescintigraphy (1-h initial images) in 61-year-old man with right upper quadrant pain for 2 days. Note the nonvisualization of gallbladder and small bowel activity. Lower activity is within the urinary bladder. Courtesy of Dr. Arthur Krasnow, Department of Radiology, Medical College of Wisconsin.
Cholescintigraphy (1-h initial images) in 61-year-old man with right upper quadrant pain for 2 days. Note the nonvisualization of gallbladder and small bowel activity. Lower activity is within the urinary bladder. Courtesy of Dr. Arthur Krasnow, Department of Radiology, Medical College of Wisconsin.
Angiography
Percutaneous transhepatic cholangiography (PTC) findings include the following:
-
An impacted calculus in the Hartmann pouch or gallbladder neck
-
Narrowed CHD at the level of impaction
-
Dilatation of the CHD distal to the level of the impacted calculus
-
Normal-caliber CBD proximal to the impacted calculus
-
This patient presented with acute cholecystitis, as confirmed at imaging. His pain resolved over a few days, but mildly elevated bilirubin levels persisted. Image obtained during endoscopic retrograde cholangiopancreatography shows smooth narrowing of the bile duct (arrow) at the site of insertion of the cystic duct (Mirizzi syndrome). Note the small calculus in the cystic duct. Courtesy of Dr. Ali Nawaz Khan.
-
Cholescintigraphy (1-h initial images) in 61-year-old man with right upper quadrant pain for 2 days. Note the nonvisualization of gallbladder and small bowel activity. Lower activity is within the urinary bladder. Courtesy of Dr. Arthur Krasnow, Department of Radiology, Medical College of Wisconsin.
-
Cholescintigraphy (3-h delayed images in the anterior projection) of the same patient as in the previous image. Note persistent nonvisualization of the gallbladder and minimal activity within the small bowel. Courtesy of Dr. Arthur Krasnow, Department of Radiology, Medical College of Wisconsin.

