Overview
Bone marrow failure syndrome (BMFS) is a group of disorders that may manifest as single cytopenia (eg, erythroid, myeloid, or megakaryocytic) or as pancytopenia. It can be either inherited or acquired.
See the image shown below.
Single cytopenia (failure of one cell line)
Types of single cytopenia are as follows:
-
Erythroid
-
Myeloid
-
Megakaryocytic
Pancytopenia (failure of all 3 cell lines)
Types of pancytopenia are as follows:
-
Hypoplastic marrow
-
Aplastic marrow
Inherited bone marrow failure syndromes
These may be classified into those that result in pancytopenia and those limited to failure of 1 or 2 hematopoietic lineages. [1, 2, 3, 4, 5, 6, 7, 8, 9] See the image below.
Syndromes that result in pancytopenia include the following:
-
Dyskeratosis congenita
Syndromes usually limited to single hematopoietic lineage include the following:
-
Congenital neutropenia, including Kostmann syndrome
-
Diamond-Blackfan anemia
-
Congenital amegakaryocytic thrombocytopenia (CAMT)
-
Thrombocytopenia absent radii (TAR) syndrome
Acquired bone marrow failure syndromes (image shown below)
 Bone marrow section from a 7-year-old girl with idiopathic acquired aplastic anemia. Hematopoietic cells are almost totally absent. Sinuses and capillaries are prominent. Iron-laden macrophages reflecting increased iron stores from repeated RBC transfusions are present.
Bone marrow section from a 7-year-old girl with idiopathic acquired aplastic anemia. Hematopoietic cells are almost totally absent. Sinuses and capillaries are prominent. Iron-laden macrophages reflecting increased iron stores from repeated RBC transfusions are present.
These include the following:
-
Aplastic anemia
-
Idiopathic, toxin, drugs, chemicals, radiation, viral infection, malnutrition or vitamin deficiencies including vitamins B12 and folate, myelodysplastic syndrome (MDS)
Pathophysiology
The proliferation and differentiation of pluripotent stem cells give rise to progeny that can populate the entire immunologic and hematopoietic systems through committed progenitors of both the lymphoid and myeloid lineages. In turn, each of these progenitors is programmed to provide the recognizable precursors of granulocyte, erythrocyte, monocyte/macrophage, megakaryocyte, eosinophil, and basophil lineages. The microenvironment, consisting of lymphocytes, macrophages, fibroblasts, endothelial elements, and stroma in which hematopoietic cells reside, creates a regulatory niche that determines the local area network.
The etiology of bone marrow failure (BMF) includes defective stem/progenitor cells and/or stroma/accessory cells/growth factors, as well as deficient nonspecific nutrients or, as in the case of acquired aplastic anemia, immune-mediated abnormalities.
Inherited bone marrow failure syndromes (IBMFS) are usually the result of intrinsic stem cell/progenitor defects. The precise pathophysiology of inherited single cell and multilineage cytopenias has not been elucidated despite the identification of many of the genes mutated in these disorders. Accelerated hematopoietic cell apoptosis has been demonstrated in virtually all IBMFS. [10, 11, 12, 13, 14, 15, 16, 17, 18]
The genetic abnormalities that are linked to IBMFS have been identified in various conditions.
Fanconi anemia is inherited in either an autosomal recessive or X-linked fashion. Biallelic pathogenic variants in 1 of the more than 22 genes involved in DNA interstrand crosslink repair cause this syndrome. [1] Fanconi anemia (FANC) genes collaborate in a complicated pathway (FA pathway), which is responsible for the repair of DNA damage. These genes include FANCA, FANCB, FANCC, FANCD1, FANCD2, FANCE, FANCF, FANCG, FANCI, FANCJ, FANCL, FANCM, and FANCN.
Dyskeratosis congenita (DKC) is inherited in an X-linked recessive, autosomal dominant, or autosomal recessive manner. Eighteen genes known to cause DKC have been identified. [1]
DKC is related to telomerase dysfunction [2, 3] ; all genes associated with this syndrome (ie, DKC1, TERT, TERC, NOP10) encode proteins in the telomerase complex responsible for maintaining telomeres at the ends of chromosomes. In the X-linked recessive form, the gene defect lies in the DKC1 gene (located at Xq28), which encodes for the protein dyskenin. Dyskenin is composed of 514 amino acids and has a role in ribosomal RNA processing and telomere maintenance. [4, 5]
In the autosomal dominant form, mutations in the RNA component of telomerase (TERC) or telomerase reverse transcriptase (TERT) are responsible for disease phenotype. [3, 6, 7] Mutation screening demonstrated other components of telomerase complex beside TERT and include NOP10 (24) in patients with rare autosomal-recessive DKC. In addition, heterozygous mutations of TINF2 encoding TIN2, the main component of shelterin that protects telomeres, have been identified in approximately 11% of DC. [6, 19]
Shwachman-Diamond syndrome is an autosomal-recessive disorder in which most patients have a mutation in the Shwachman Bodian Diamond syndrome gene (SBDS) located at band 7q11. More recently, three additional genes (DNAJC21, EFL1, and SRP54) have been reported to cause Shwachman-Diamond syndrome or a similar syndrome. [1]
Diamond-Blackfan anemia is usually an autosomal dominant disease in which 25% of patients have a mutation in the gene for small ribosomal protein (RPS19) located at band 19q13.2. Diamond-Blackfan anemia is caused by mutations in the RPL5, RPL11, RPL35A, RPS7, RPS17, RPS19, and RPS24 genes. These genes provide instructions for making several of the more than 75 different ribosomal proteins, which are components of cellular structures called ribosomes. Ribosomes process the cell's genetic instructions to create proteins. These mutations in the RPL5, RPL11, RPL35A, RPS7, RPS17, RPS19, and RPS24 genes are believed to affect the stability or function of the ribosomal proteins.
Severe congenital neutropenia (SCN) is associated with dominant mutations genes associated with SCN (ie, ELANE, G6PC3, GFI1, HAX1, WAS). These genes play a role in the maturation and function of neutrophils. Gene mutations that cause SCN lead to the production of neutrophils that die prematurely or are dysfunctional. Some gene mutations result in unstable proteins that build up in neutrophils, leading to cell death. Other gene mutations result in proteins that impair the maturation or function of neutrophils, preventing these cells from responding appropriately to immune signals. About 50% cases of SCN are caused by mutations in the ELANE gene. Another 15% are caused by mutations in the HAX1 gene. The other genes (GFI1, WAS, G6PC3) account for only a small percentage of SCN. In about one-third of patients with SCN, the cause of the disorder is unknown.
Thrombocytopenia absent radii (TAR) syndrome has not been identified with any particular gene in this autosomal recessive disorder.
Congenital amegakaryocytic thrombocytopenia (CAMT) is an autosomal recessive disorder with biallelic mutations in the thrombopoietin receptor (MPL) at band 1p34.
GATA2 deficiency and SAMD9/SAMD9L syndromes have been more recently recognized as causes of marrow failure. [1]
GATA2 deficiency is a germline immunodeficiency syndrome associated with a high long-term risk of MDS and acute myeloid leukemia (AML), and an inherited BMFS that includes the clinical entities previously known as MonoMAC syndrome; familial MDS/AML; dendritic cell, monocyte B and NK lymphoid (DCML) deficiency; and Emberger syndrome. The various phenotypes result from pathogenic variants in the GATA2 gene.
Germline pathogenic gain-of-function variants in the SAMD9 and SAMD9L genes have been described in association with several clinical disorders including Myelodysplasia, Infections, Restriction of growth, Adrenal hypoplasia, Genital phenotypes, and Enteropathy (MIRAGE) syndrome, and MDS and ataxia-pancytopenia syndrome (ATXPC).
Frequency and Mortality/Morbidity
United States
The incidence of bone marrow failure resulting from hypoplastic or aplastic anemia is low in the United States and Europe (2-6 cases per million persons) compared with the prevalence of bone marrow failure (BMF) resulting from acute myelogenous leukemia and multiple myeloma (27-35 cases per million persons). The incidence of myelodysplasia, on the other hand, has increased from 143 cases reported in 1973 to about 15,000 cases annually in United States. This is an underestimation of the actual incidence, which is believed to be about 35,000-55,000 new cases a year.
International
BMF is more common in the East than in the West. In Japan and the Far East, the frequency is at least 3 times higher than it is in the United States and Europe. Mexico and Latin America also have high occurrence rates, which are attributed to the liberal use of chloramphenicol. Environmental factors and pervasive use of insecticides have been implicated as a cause of this disease. The incidence of myelodysplasia was recently estimated to be around 4-5 cases per 100,000 population per year in Germany and Sweden.
Mortality/morbidity
Morbidity and mortality from pancytopenia are caused by low levels of mature blood cells. Severe anemia can cause high-output cardiac failure and fatigue. Neutropenia can predispose individuals to bacterial and fungal infections. Thrombocytopenia can cause spontaneous bleeding and hemorrhage.
The severity and extent of the cytopenia influences the prognosis. Severe pancytopenia is a medical emergency, requiring rapid institution of definitive therapy (ie, early determination of supportive care and identification of bone marrow transplant candidates).
Several of the inherited bone marrow failure syndromes (IBMFs) are associated with a high-risk of leukemia and/or specific solid tumors. [20, 8, 21]
Clinical Presentation
History
Weakness and fatigue resulting from anemia can develop slowly. Months may elapse before the patient seeks medical help with these symptoms
Low platelet counts predispose patients to spontaneous bleeding in the skin and mucous membranes. Neutropenia places the patient at risk for serious infections. Bleeding complications are usually the most alarming symptom, and infections prompt individuals to visit the emergency department.
Additional clues may be found in the family histories, which must include information about hematologic diseases, leukemia, solid tumors, and birth defects or other abnormal physical findings. The inheritance patterns of the inherited bone marrow failure syndromes (IBMFS) encompass autosomal recessive, autosomal dominant, and X-linked recessive, as well as sporadic cases; thus, drawing of a pedigree should be part of the history. Personal medical histories are also informative because many of the inherited bone marrow failure syndromes (particularly Fanconi anemia and dyskeratosis congenita) may present with syndrome-specific cancers, myelodysplastic syndrome (MDS), or leukemia prior to the development of aplastic anemia. [8]
Ethnic background is relevant because founder mutations for Fanconi anemia genes are found in Ashkenazi Jews, South African Afrikaners, and Spanish Romani; these genes increase the expected carrier rates from 1 in 300 to 1 in 100 and the incidence of homozygotic individuals from 1 in 360,000 to 1 in 40,000.
Exposure to toxins, drugs, environmental hazards, and recent viral infections (eg, hepatitis) should be noted.
Physical examination
The manifestations of bone marrow failure relate to the clinical effects of low blood cell counts.
Patients with severe anemia may present with pallor and/or signs of congestive heart failure, such as shortness of breath.
Bruising (eg, ecchymoses, petechiae) on the skin, gum bleeding, or nosebleeds frequently are associated with thrombocytopenia.
Fever, cellulitis, pneumonia, or sepsis can be complications of severe neutropenia.
Inherited bone marrow failure (IBMF) includes Fanconi anemia, which has characteristic physical developmental anomalies including absent thumbs, absent radius, microcephaly, renal anomalies, short stature, and abnormal skin pigmentation (ie, café-au-lait and hypopigmented or hyperpigmented spots). As many as half of patients with Fanconi anemia may not exhibit obvious developmental or skin manifestation, and it is increasingly clear that the diagnosis should be considered in adults with bone marrow failure, myelodysplastic syndrome, or early onset of epithelial cancer.
Fever, cellulitis, pneumonia, or sepsis can be infectious complications of severe neutropenia
Characteristics of Specific Bone Marrow Failure Syndromes
Single cytopenia
Diamond-Blackfan anemia (congenital pure red cell aplasia)
Diamond-Blackfan anemia is a disorder with pure red cell aplasia, in which 90% of patients are diagnosed in the first year. The physical findings may include short stature and abnormal thumbs (hypoplastic, triphalangeal, or with underdeveloped thenar muscles), but many patients are normal in appearance. The anemia is usually macrocytic, with elevated fetal hemoglobin, and increased red cell adenosine deaminase.
Diamond-Blackfan anemia is caused by mutations in the RPL5, RPL11, RPL35A, RPS7, RPS17, RPS19, and RPS24 genes. These genes provide instructions for making several of the more than 75 different ribosomal proteins, which are components of cellular structures called ribosomes. Ribosomes process the cell's genetic instructions to create proteins.
Some ribosomal proteins are involved in the assembly or stability of ribosomes. Others help carry out the ribosome's main function of translating proteins. Studies suggest that some ribosomal proteins may have other functions, such as participating in chemical signaling pathways within the cell, regulating cell division, and controlling the self-destruction of cells (apoptosis).
Mutations in the RPL5, RPL11, RPL35A, RPS7, RPS17, RPS19, and RPS24 genes are believed to affect the stability or function of the ribosomal proteins. Studies indicate that a shortage of functioning ribosomal proteins may increase the self-destruction of blood-forming cells in the bone marrow, resulting in anemia. Inappropriate triggering or regulation of cell division and apoptosis may contribute to the other health problems that affect some people with Diamond-Blackfan anemia.
Approximately half of all individuals with Diamond-Blackfan anemia have identified mutations. Researchers suspect that other unidentified genes may also be associated with this disorder
Mutations in the gene for small ribosomal protein (RPS19), located at 19q13.2, are found in approximately 25% of patients with Diamond-Blackfan anemia. A small proportion of patients may develop pancytopenia. In about 85% of patients with Diamond-Blackfan anemia, the erythrocyte adenosine deaminase level is elevated. [1]
Most patients with Diamond-Blackfan anemia improve with corticosteroid treatment. Those who require high doses or fail to respond receive regular red cell transfusions and eventually require iron chelation. Stem cell transplantation is sometimes recommended for such patients. Note that 15-25% of patients undergo remission and may not need treatment again; however, some may relapse after reaching adulthood. [2, 22, 23]
Shwachman-Diamond syndrome
Shwachman-Diamond syndrome (SDS) results from disordered ribosomal biogenesis. It is characterized by bone marrow failure, skeletal abnormalities, exocrine pancreatic dysfunction, and an increased risk of myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML). In 90% of patients with SDS, genetic testing for the SBDS gene on chromosome 7q11 confirms the diagnosis. More recently, other genes (DNAJC21, EFL1, and SRP54) have been linked to SDS or a similar syndrome. [1]
The most common hematologic manifestation is neutropenia, which requires monitoring. Granulocyte colony-stimulating factor (G-CSF) therapy is recommended for patients with severe persistent neutropenia who have recurrent infections. For those with BMF or leukemia, hematopoietic cell transplantation (HCT) is the only curative treatment. The prognosis is particularly poor for patients who have SDS-related AML, owing to resistant disease and treatment toxicity. [1]
Thrombocytopenia absent radii syndrome
Thrombocytopenia absent radii syndrome (TAR) is perhaps the only inherited bone marrow failure syndrome (IBMFs) that should be exclusively diagnosed in the neonatal period, when patients present with thrombocytopenia and bilateral absence of the radii. If patients survive beyond the first year, the platelet count stabilizes, and the prognosis is much better. Treatment during infancy or later for surgical procedures includes platelet transfusions as needed. Stem cell transplantation has been rarely performed for patients whose severe thrombocytopenia did not improve. [24]
Congenital amegakaryocytic thrombocytopenia
This is a rare autosomal recessive bone marrow failure syndrome induced by mutations of the gene coding for thrombopoietin (TPO) receptor (c-MPL), despite high levels of serum TPO. It presents with isolated thrombocytopenia in infancy and develops into pancytopenia in later childhood. It has tendency to transform into MDS/AML. Classic diagnostic bone marrow findings reveal absent or significantly decreased megakaryocytes with otherwise normal marrow cellularity. The primary treatment is bone marrow transplantation.
Severe congenital neutropenia
Severe congenital neutropenia (SCN) is defined as early onset severe neutropenia, with absolute neutrophil counts below 200/mcL (see the Absolute Neutrophil Count calculator) and severe infections. More than half of all patients have dominant mutations in neutrophil elastase (ELA2), which is located at 19p13.3; a few patients have mutations in GFI-1 and HAX1. Patients may develop myelodysplastic syndrome (MDS) or leukemia. Patients with severe congenital neutropenia often improve when treated with G-CSF.
Patients may develop MDS or leukemia, long-term follow-up is recommended. [24] Based on the published data from Severe Chronic Neutropenia International Registry (SCNIR), G-CSF is considered specific and effective therapy for long-term management of chronic neutropenia. During therapy, patients commonly develop bony pain early in the course of treatment; they may also develop splenomegaly (15%), osteopenia/osteoporosis (17%), vasculitis (4%), and thrombocytopenia (4%). Long-term potential risk of transformation to MDS or acute myeloid leukemia was 9%, according to the report. It is believed to be due to the underlying genetic mutation with multistep evolution to monosomy 7, Ras oncogene mutations, and finally overt malignant disease. [25]
Therefore, patients with severe congenital neutropenias on G-CSF therapy should have annual bone marrow assessment to monitor early morphologic and cytogenetic changes.
GATA2 deficiency
GATA2 deficiency is a germline immunodeficiency syndrome associated with a high long-term risk of MDS and AML; this syndrome includes the entities previously known as MonoMAC syndrome, familial MDS/AML, DCML deficiency, and Emberger syndrome. The various phenotypes result from pathogenic variants in the GATA2 gene. About 72% of adolescents with MDS and monosomy 7 have GATA2 deficiency. [1]
Diagnosis of GATA2 deficiency requires high clinical suspicion. Although many patients have no symptoms, persistent warts, monocytopenia, NK cell/B cell deficiency, pulmonary alveolar proteinosis (PAP), or high-risk MDS can suggest the diagnosis. Genetic analysis of GATA2 is confirmatory; however, false-negative results may occur owing to regulatory region pathogenic variants or copy number variants, which may necessitate further genomic analyses or mRNA sequencing. [1]
The only curative option is HCT, particularly for patients with MDS. HCT can resolve MDS, ameliorate PAP, and decrease infection burden; however, the optimal timing and regimen remain uncertain. Patients with advanced MDS have worse outcomes with HCT than those with moderate or mild disease. Future advances in gene technology such as homologous recombination and CRISPR/Cas9 hold promise for individualized treatment. [1]
SAMD9/SAMD9Lsyndromes
Germline pathogenic gain-of-function variants in the SAMD9 and SAMD9L genes have been linked to several disorders, including MIRAGE syndrome, MDS, and ATXPC syndrome. GATA2 deficiency and SAMD9/SAMD9L syndromes are together responsible for 50% or more of MDS cases in children and adolescents.
Heightened clinical suspicion and early screening for SAMD9/SAMD9L pathogenic variants are essential for diagnosis. Because both SAMD9 and SAMD9L are found on chromosome 7, genetic testing with nonblood material is advised for patients with monosomy 7 and pediatric MDS.
Treatment approaches vary based on the presentation and subtype. Watchful waiting may be appropriate for patients with stable disease, in whom spontaneous remission is possible. HCT has been successful in patients with MDS; however, outcomes in those with severe MIRAGE and ATXPC syndromes have been poor.
Pancytopenias
Fanconi anemia
Fanconi anemia is the most common type of IBMFs. Although approximately 75% of the known patients with Fanconi anemia have one or more physical abnormalities, many patients appear healthy or have subtle findings that may be overlooked (such as short stature, café au lait spots, and hypoplastic thenar muscles). Approximately 10% of the reported patients are age 16 years or older at the time of diagnosis. The presence of significant birth defects correlates with early onset hematologic disease.
The diagnosis of Fanconi anemia homozygotes is confirmed by the detection of chromosome aberrations (breaks, gaps, rearrangements, endoreduplications) in cells (usually blood lymphocytes stimulated with phytohemagglutinin) following culture with DNA crosslinking agents, such as diepoxybutane (DEB) or mitomycin C (MMC). In approximately 10-15% of patients, somatic mosaicism is found, in which some or all of the hematopoietic cells have undergone molecular gene correction. Failure to correctly diagnose Fanconi anemia may be fatal to the patient.
Fanconi anemia is an autosomal-recessive disease in most affected patients. Eleven Fanconi anemia genes have been cloned to date. These genes are FANCA, FANCB, FANCC, FANCD1, FANCD2, FANCE, FANCF, FANCG, FANCI, FANCJ, FANCL, FANCM and FANCN. The Fanconi anemia gene products collaborate in a complicated pathway whose ultimate role is the repair of DNA damage. An intermediate repair step involves the formation of protein complexes. Biallelic pathogenic variants in 1 of the more than 22 genes involved in DNA interstrand crosslink repair are responsible for Fanconi anemia. [1]
The Fanconi anemia consensus guidelines suggest initiation of packed RBC transfusion when the hemoglobin level is 8 g/dL or less and platelet concentrates transfusion when the platelet count is 30,000 mcL. Febrile episodes when neutrophil count less than 1000/mcL are managed by broad spectrum parenteral antibiotics. In the same time patients with an HLA-matched healthy related donor should be offered stem cell transplant. Preparation for stem cell transplant has been most successful with low-dose cyclophosphamide -based conditioning regimen, and the survival is more than 70%; with an alternative donor, the survival is less than 40%. Hematopoietic stem cells can be obtained from bone marrow, cord blood, or peripheral blood. [26, 27]
Patients without a matched sibling donor should be offered treatment with androgens, usually oxymetholone at 2-5 mg/kg/d. More than 50% respond with improved blood counts, and the dose can be titrated to maintain adequate numbers. Side effects of androgens include virilization, liver dysfunction, and liver tumors (3% of reported patients with Fanconi anemia) and treatment should be monitored with physical examinations, liver function tests, and abdominal ultrasound examinations.
Leukemia has been reported in approximately 10% of patients, and MDS has been reported in about 6% of patients (see the image below), primarily in teens and young adults, some of whom may not have had a preceding phase of aplastic anemia.
 Clonality of the stem cell compartment during evolution of myelodysplastic syndromes and other bone marrow failure syndromes.
Clonality of the stem cell compartment during evolution of myelodysplastic syndromes and other bone marrow failure syndromes.
Solid tumors have been reported in close to 10% of patients, often in young adults who may never have had aplastic anemia. The most common tumors are liver adenomas and hepatomas, primarily in patients who had aplastic anemia that was treated with oral androgens. Other types of solid tumors occur in young adults and primarily involve the head and neck, esophagus, and gynecologic areas. Oral cancers have been reported in patients with Fanconi anemia who have received bone marrow transplantation; transplantation (especially if graft versus host disease occurs) appears to further increase the risk of these cancers. [28, 29, 19, 30, 31, 32, 22, 33, 34, 21]
Dyskeratosis congenita
This is a rare, progressive bone marrow failure syndrome characterized by the triad of reticulated skin hyperpigmentation, nail dystrophy, and oral leukoplakia. Dyskeratosis congenita (DKC) is genetically heterogeneous, with X-linked recessive, autosomal dominant, and autosomal recessive subtypes. DKC is related to telomerase dysfunction. Analysis of 270 families in the DKC registry found that mutations in dyskenin (DKC1), TERT, and TERC only account for 64% of patients, with an additional 1% due to NOP10, suggesting that other genes associated with this syndrome are, as yet, unidentified. To date, 18 genes known to cause DKC have been identified. [1]
The incidence of classic DKC is approximately 1/1,000,000 individuals annually. [15] Patients usually present during the first decade of life, with the skin hyperpigmentation and nail changes typically appearing first.
In an analysis of individuals with DKC, approximately 70% of patients died either directly from bone marrow failure or from its complications at a median age of 16 years. Eleven percent died from sudden pulmonary complications; a further 11% died of pulmonary disease in the bone marrow transplantation setting. Seven percent died from malignancy (eg, Hodgkin disease, pancreatic carcinoma). Fatal opportunistic infections such as Pneumocystis carinii pneumonia and cytomegalovirus infection have been reported.
Specific tests depend on the clinical findings and may include a CBC count, chest radiography, pulmonary function tests, and stool tests for occult blood. Elevated von Willebrand factor levels have been associated with fatal vascular complications after bone marrow transplant and may be a marker for patients with a predisposition for endothelial deterioration.
Flow cytometry with fluorescence in situ hybridization (flow-FISH) is used to detect shortened leukocyte telomere length and/or to identify pathogenic variants in telomere biology genes. [1] Mutations in the TERC gene and in the TERT gene, the gene for telomerase reverse transcriptase (another member of the ribonucleoprotein complex), have been identified in a subset of patients with aplastic anemia.
Genetic testing for occult DKC should be considered in patients with aplastic anemia. However, a 2006 genetic analysis of the TERC gene among 284 children with either aplastic anemia or myelodysplastic syndrome found only 2 mutations in the TERC gene.
Medical management of the bone marrow failure includes androgens as in Fanconi anemia, with perhaps a benefit from the addition of erythropoietin and G-CSF. Approximately 50% of patients experience a temporary increase in blood counts with androgen therapy.
The aplastic anemia may require treatment by bone marrow transplant, but the overall survival is less than 30%, whether the donor is matched-related or mismatched or unrelated. Some of the deaths were due to late developments of mucositis or venoocclusive disease, and it is speculated that there may be toxicity from preparation with cyclophosphamide or radiation. Nonmyeloablative hematopoietic stem cell transplant conditioning regimens (ie, reduced-intensity conditioning) with fludarabine may offer better outcomes. Recent review showed that reduced intensity conditioning was associated with 22% mortality rate compared with a 71% mortality rate with traditional myeloablative regimens.
Cancer was reported in close to 15% of the reported cases. Most were squamous cell carcinomas of the oropharyngeal and gastrointestinal regions, at a median age of 30 years, similar to Fanconi anemia. Leukemia and MDS also occur in DKC, but are less common.
Acquired aplastic anemia
Aplastic anemia is a life-threatening bone marrow failure disorder, which can lead to a high mortality rate if untreated. Hematopoietic stem-cell transplantation offers an opportunity for cure, but for those who do not have a suitable donor or who are unfit for the procedure, alternative therapeutic options are available, such as immune suppressive therapy with antithymocyte globulin (ATG) and cyclosporine (CsA) or high–dose cyclophosphamide.
In 50% of cases, acquired aplastic anemia occurs in first 3 decades of life. The incidence is 2 cases per 1,000,000 population per year in Western countries. Its occurrences has been associated with multiple etiologies including chemicals, drugs to infectious associations such as hepatitis, and infectious mononucleosis. In addition association with pregnancy and collagen vascular process (eg eosinophilic fasciitis, seronegative hepatitis) indicates different mechanisms of disease and also include host genetic predisposition.
Immune-mediated dysfunction underlines the disease. With an immune response with expanded oligoclonal cytotoxic T cells targeting hematopoietic stem and progenitor cells. This was proven in vitro by improvement in the colony number in tissue culture after removal of lymphocytes, and their addition to normal marrow inhibits hematopoiesis. Specific CD8+CD28- cell clones are expanded in aplastic anemia peripheral blood, as manifest by skewed usage of the Vb repertoire; and oligoclones recognize and induce apoptosis of autologous myeloid cells. [35] Regulatory T cells, which control and suppress autoreactive T cells, are decreased at presentation in almost all patients with aplastic anemia. [36]
Aplastic anemia can predispose to cancer. It evolves to clonal disorders such as paroxysmal nocturnal hemoglobinuria (PNH), myelodysplasia (MDS) and acute myeloid leukemia. A study suggested that the detection of a paroxysmal nocturnal hemoglobinuria clone can be a useful diagnostic tool to exclude the diagnosis of inherited bone marrow failure syndromes from acquired aplastic anemia and focus the work-up and treatment on an acquired form of marrow failure. [37]
Administration of ATG leads to depletion of immune compete cells, its exact mechanism of action remains unclear. [38] ATG preparations contain various antibodies recognizing human T-cell epitopes, many directed against activated T cells or activation antigens. [39, 40]
CsA has a more selective inhibitory effect on T lymphocytes, suppressing early cellular response to antigenic and regulatory stimuli. By blocking expression of nuclear regulatory proteins, it leads to reduced T-cell proliferation and activation with diminished release of cytokines such as interleukin-2 and interferon-gamma. The combination of ATG and CsA is the current standard therapy in severe aplastic anemia. [41, 42, 43] Overall response is achieved in about two thirds of patients; the cumulative incidence of relapse among responders is approximately 20–30% and clonal evolution occurs in about 10–15% of cases. [44, 45, 46, 47]
Pediatric population studies in general report a higher response rate of about 70–80% with long-term survival of 80–90%; relapse and clonal evolution occur at rates that are comparable with what is observed in patients of all ages. [46, 48, 49] As first course, Horse ATG (h-ATG) is used in the immunosuppressive combination, however for refractory and relapse cases further courses are given using rabbit ATG (r-ATG). r-ATG appears to be more immunosuppressive as a more prolonged lymphopenia is observed with this agent compared with h-ATG. [50] It may promote immune regulation as suggested by an in vitro assay where CD4+CD25- were converted to CD4+CD25+ regulatory T cells in the presence of r-ATG but not h-ATG. [51]
For the one third of patients who are refractory to h-ATG/CsA, repeated courses of immunosuppression have yielded response rates varying from 30–70%. [52, 53, 54] Re-treatment with ATG/CsA in relapsed aplastic anemia has resulted in response rates of 50–60%. [53, 54, 55]
Addition of further immunomodulatory therapy in addition to ATG/CsA (such as G-CSF, mycophenolate mofetil, sirolimus, androgens, corticosteroids) has not resulted in better response rates or decreased relapse rates and clonal evolution.
Using high-dose cyclophosphamide alone without hematopoietic stem cell transplantation is also a therapeutic option. It leads to durable remission in most patients with severe aplastic anemia. Results from more than 100 patients treated with high-dose cyclophosphamide have been reported in the medical literature. According to these data, the response rate in treatment-naive patients is 70%, with most responders achieving a complete remission (normalization of peripheral blood counts). Relapse and secondary clonal disorders (PNH and MDS) may occur; however, these appear to be rare events. Overall and event-free survival are less in patients with refractory severe aplastic anemia, and the risk of fungal infections is increased; however, durable remission has been described in roughly 25% of patients.
For patients who are not suitable candidates for hematopoietic stem cell transplant, both ATG/CsA and high-dose cyclophosphamide are reasonable options. Both have response rates of 70%. [56, 57]
Allogeneic stem cell transplantation from an HLA-matched sibling is curative therapy in most patients who undergo this procedure. The International Bone Marrow Transplant Registry showed 77% 5-year survival. [58] In children and patients who are minimally transfused, survival of 80–90% can be achieved. [59] Modern radiation-free conditioning regimens (cyclophosphamide + ATG) have improved the tolerability and allowed for engraftment in heavily transfused patients. [60] Alternate stem cell donor source can be offered (Matched unrelated, umbilical cord) for those who lacked an HLA-matched related donor or failed to respond to immune suppressive therapy (IST) or have recurrent disease after IST.
Workup
Pancytopenia
The following should be considered in the workup:
-
History
Detailed drug history
Toxin and radiation exposure history
Family history of aplastic anemia
-
Physical examination for congenital anomalies
-
Blood cell count, including absolute reticulocyte count, granulocyte count, hemoglobin level, hematocrit level, mean corpuscular volume, platelet count
-
Antinuclear antibody (ANA) and DNA titer, Coombs test, rheumatoid factor, liver function tests, tuberculin test
-
Viral serology, including HIV, Epstein-Barr virus (EBV), parvovirus, and hepatitis A, B, and C; polymerase chain reaction (PCR) for virus, when indicated
-
Serum vitamin B12, red cell, and serum folate levels
-
Bone marrow aspiration and trephine biopsy; because of patchiness of bone marrow involvement, biopsy at multiple sites may be required
-
Chromosome breakage assay on blood lymphocytes or skin fibroblasts using clastogen stimulation (eg, diepoxybutane or mitomycin C) to diagnose Fanconi anemia (skeletal radiography; renal, cardiac, and abdominal ultrasonography; and chest radiography to determine congenital anomalies in Fanconi anemia)
-
Cytogenetic and fluorescent in situ hybridization (FISH) studies
-
Flow cytometric immunophenotypic analysis of erythrocytes for deficiency of glycosyl-phosphatidylinositol-linked surface protein (eg, CD55/59) to exclude paroxysmal nocturnal hemoglobinuria
-
Diagnostic tests to rule out Schwachman-Diamond syndrome, such as skeletal radiography, chest radiography, and pancreatic ultrasonography and serum trypsinogen and isoamylase level measurement
-
Mutation analysis for inherited bone marrow failure syndromes (IBMFS) when suspected. Screening tests as needed (red cell ADA levels for DBA, shortened lymphocyte telomere length for DC)
Fanconi anemia
Further work up is indicated to rule out FA in the following individuals:
-
Children with unexplained cytopenias
-
Children with myelodysplastic syndrome (MDS) or acute myeloid leukemia (AML)
-
Patients with classic birth defects suggestive of Fanconi anemia
-
Patients with skeletal, urogenital and cardiac
-
Patients with excessive café au lait spots, microcephaly, microphthalmia, and growth failure
-
Patients who develop squamous cell carcinoma at a young age in the esophagus, head, neck, or female genitalia and those who develop liver tumors
-
Patients with karyotype with spontaneous chromosome breaks
-
Patients with unexplained macrocytosis and an elevated fetal hemoglobin level
Following studies are indicated in patients with Fanconi anemia:
-
Endocrine studies for the following conditions:
Short stature (growth hormone deficiency)
Glucose intolerance
Pubertal delay
Evaluation of undescended testes
-
Imaging studies to evaluate the following conditions:
Hepatic structural abnormalities: Hepatic Ultrasonography
Orthopedic anomalies: Skeletal X-ray
Genitourinary abnormalities: Ultrasonography/ CT-Scan Abdomen
Head anomalies: CT-Scan of the Head
-
Cardiac defects: Echocardiography
-
Serum chemistries for liver and kidney function
-
Hearing test
The following tests should be performed in patients with Fanconi anemia, receiving red cell transfusion therapy:
-
Ferritin level assay; other assays for iron overload include superconductivity quantum interference device (SQUID) and MRI T2* (liver and heart, if available).
-
Liver enzyme assay
A survey of family members of patients with Fanconi anemia is indicated for the following:
-
To rule out Fanconi anemia in other family members
-
To type family members to determine the potential availability of an HLA-matched sibling for future consideration of bone marrow transplantation
-
To provide genetic counseling to parents and patient
Prospective counseling and screening in patients with Fanconi syndrome includes cancer surveillance.
Close monitoring of patients who are managed conservatively with blood product transfusion or on androgen therapy is indicated. In addition patients who underwent successful stem cell transplantation. Evaluation of hematologic parameters and clinical surveillance of the patient to look for early signs of MDS/AML or other non hematopoietic malignancies.
Histologic Findings in Bone Marrow Failure Syndromes
The histologic findings in aplastic anemia include pancytopenia and a hypocellular bone marrow revealed by bone marrow biopsy. Aplastic anemia is classified as a normochromic, normocytic anemia, although some patients have macrocytosis. Residual leukocytes are morphologically normal, but the number and size of platelets are decreased. The reticulocyte count is also inappropriately decreased. The bone marrow reveals decreased hematopoiesis, and in its severe form, only a few lymphocytes, plasma cells, and mast cells may be evident. The bone marrow is replaced by fat. The different cell lines may be variably affected, and in some cases, a small amount of erythropoiesis may be evident. The iron-binding capacity is usually fully saturated, and an iron stain of the bone marrow reveals normal to increased iron stores.
Previously, the term hypoplastic anemia was differentiated from aplastic anemia and used to describe mild pancytopenia and hypocellularity of the marrow.
Aplastic anemia is currently defined as mild or severe, based on the severity of the pancytopenia and the degree of cellularity of the bone marrow. Patients with mild aplasia may have a prolonged course or a complete spontaneous recovery. They may also progress into a severe aplastic anemia. Patients with severe aplastic anemia have only a 15-20% chance of spontaneous recovery and are likely to have a fulminate course with early death without successful treatment.
Workup should include studies that attempt to identify the possible cause of the aplasia, including tests for paroxysmal nocturnal hemoglobinuria, systemic lupus erythematosus, hepatitis, infectious mononucleosis, and pregnancy in females of childbearing age. Cytogenetic analysis should attempt to identify patients with hypocellular myelodysplastic syndrome and those patients with underlying chromosomal fragility states, such as Fanconi aplastic anemia. Flow cytometry enhances identification of an underlying paroxysmal nocturnal hemoglobinuria and abnormal lymphocyte subsets.
The evaluation of a congenital disorder should include radiography of the hands, wrists, and kidneys. Additional work-up and testing is needed for patient management. Complete erythrocyte typing should be established before transfusion. The patient’s cytomegalovirus (CMV) history should be determined serologically to provide appropriate transfusion products and to determine an appropriate hematopoietic stem cell transplant donor. Immediate human leukocyte antigen (HLA) typing of the patient and family should be undertaken to determine the availability of a potential sibling transplant donor. On rare occasions, a parent may be a suitable donor. Typing should include serologic typing for HLA-A, HLA-B, and HLA-DR. If a search for an unrelated donor is to be pursued, molecular typing for HLA-DR should also be performed.
Human parvovirus B19 (PVB19) infection may cause mild pancytopenia characterized by transient and spontaneous recovery in healthy subjects. Severe aplastic anemia is associated with PVB19 infection in patients without an underlying disease.
Management for Inherited Bone Marrow Failure Syndromes
Table 1. Treatment for Respective Bone Marrow Failure Syndromes (Open Table in a new window)
Syndrome |
When to Treat |
Pharmaceutical Treatment |
Transfusions |
Stem Cell Transplant |
Spontaneous Improvement |
Fanconi anemia |
Hemoglobin level < 8 g/dL, ANC < 1000/mcL, or platelets < 30,000/mcL |
Androgens, usually (eg, oxymetholone 2-5 mg/kg/d PO); granulocyte-colony stimulating factor (G-CSF): 5 mg/kg/d SC |
Packed red cells or platelet as needed |
Bone marrow or cord blood |
Rare |
Dyskeratosis congenita |
Hemoglobin level < 8 g/dL, ANC < 1000/mcL, or platelets < 30,000/mcL |
Androgens, usually (eg, oxymetholone 2-5 mg/kg/d PO); G-CSF: 5 mg/kg/d SC |
Packed red cells or platelet as needed |
Packed red cells or platelet as needed |
Rare |
Diamond-Blackfan anemia |
Hemoglobin level < 8 g/dL |
Prednisone: 2-5 mg/kg/d PO |
Packed red cells |
Bone marrow or cord blood |
Approximately 25% of cases |
Shwachman-Diamond syndrome |
ANC < 1000/mcL |
G-CSF: 5-10 mg/kg/d SC |
... |
Bone marrow or cord blood |
No |
Severe congenital neutropenia |
ANC < 1000/mcL |
G-CSF: 5-10 mg/kg/d SC |
... |
Bone marrow or cord blood |
No |
Thrombocytopenia absent radii (TAR) syndrome |
Platelets < 15,000/mcL |
None |
Platelets as needed |
Bone marrow or cord blood |
Most patients |
Amegakaryocytic thrombocytopenia |
Hemoglobin level < 8 g/dL, ANC < 1000/mcL, or platelets < 30,000/mcL |
Androgens, usually (eg, oxymetholone 2-5 mg/kg/d PO) G-CSF: 5 mg/kg/d SC |
Packed red cells or platelets as needed |
Bone marrow or cord blood |
No |
Consultations
These are as follows:
-
Hematologists should manage patients with bone marrow failure syndromes.
-
An infectious disease specialist may be necessary.
-
In severe cases, early consideration for bone marrow transplantation should be initiated
Prognosis
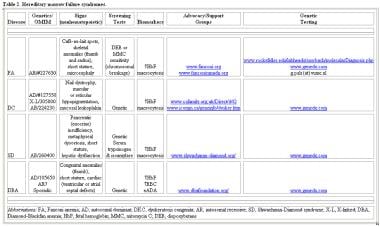
Table 2. Risk of Neoplasia in Inherited Bone Marrow Failure Syndromes (Open Table in a new window)
Syndrome |
Leukemia |
Solid Tumors |
Fanconi anemia |
Acute myeloid leukemia (AML) |
Head and neck squamous cell carcinoma; gynecologic, esophageal, and brain tumors One of these genes |
Dyskeratosis congenita |
AML |
Head and neck tumors and anogenital carcinomasOne of these genes |
Diamond-Blackfan anemia |
AML |
Osteogenic sarcomas |
Shwachman-Diamond syndrome |
AML |
None |
Severe congenital neutropenia |
AML |
None |
Thrombocytopenia absent radii (TAR) syndrome |
AML |
None |
Table 3. Relative risk of Acute Myeloid Leukemia/Myelodysplastic Syndrome in Bone Marrow Failure Syndromes (Open Table in a new window)
Cytopenia |
Disorder |
Mutation |
Relative risk AML/MDS |
Pancytopenia |
Fanconi anemia |
DNA repair |
30-40% |
Thrombocytopenia |
Amegakaryocytic Thrombocytopenia |
Cytokine receptor |
55% |
Anemia |
Diamond-Blackfan anemia |
Ribosomal biogenesis |
1% |
Neutropenia |
Severe congenital neutropenia |
Proteinase |
21% |
Patients with Fanconi anemia are at increased risk of developing malignancies including AML, MDS, head/neck cancers, and gynecologic malignancies; the relative risk (RR) of developing specific solid tumors and AML/MDS ranges from several hundred-fold to several thousand-fold compared with the general population. [61, 62]
Patients with Diamond-Blackfan anemia (DBA) are also at increased risk of developing malignancies; a longitudinal study of 72 patients with DBA reported 4 cases of AML between 15–30 years after diagnosis of DBA. [63] Osteogenic sarcoma has also been reported in patients with DBA.
Patients with dyskeratosis congenita (DKC) are at increased risk for hematologic and solid malignancies, with a cumulative incidence approaching 50% at age 50 years. [64, 65]
Patients with severe congenital neutropenia (SCN) are increased risk of myelodysplastic and leukemic transformation. About 90% of patients respond to G-CSF administration with a subsequent decrease in sepsis-related mortality to almost 1% per year during the first decade of life. [66] However, G-CSF poor and nonresponders remain at particularly high risk for hematopoietic dysplasia/malignancy with a cumulative incidence of 21% following 10 years of G-CSF therapy and increases significantly thereafter.{Re84}
North American registry data suggest a relative plateau in the hematologic malignancy risk after 10–15 years, similar to Fanconi anemia and DKC. [67] SCN pathology and the degree of severity that predisposes to malignancy as the incidence of MDS/AML transformation at 10 years was only 15% for patients without neutropenia on G-CSF compared with 34% for patients with persistent neutrophil counts below 2100/mcL despite high doses (>8 mcg/kg/d) of G-CSF. Prolonged use of G-CSF therapy is controversial to predispose to malignant transformation. However, large cohorts of other patients receiving chronic G-CSF therapy for cyclic and idiopathic neutropenia have not reported malignant transformation. [68] Additionally, risk of malignant transformation in patients with SCN receiving high doses of G-CSF does not appear to be greater than other bone marrow failure syndromes with high malignancy rates such as Fanconi anemia and DKC. [67]
Patients with Shwachman-Diamond syndrome (SDS) have an increased risk of development of MDS and AML. The French SCN registry recorded a 19% cumulative incidence of MDS/AML by age 20 years of in 55 patients with SDS; this incidence increased to 36% by age 30 years. [69] In contrast, the NCIs IBMF registry of 17 patients with SDS followed for a cumulative duration of 274 person-years did not observe any malignancy development. [70]
The prognosis of bone marrow failure depends on the duration of the marrow function abnormality. Most inherited forms of bone marrow failure, such as Fanconi anemia, are associated with transformation into leukemia several years later. Viral-induced bone marrow failure, such as seen with parvovirus infection, are usually self-limiting. Acquired idiopathic aplastic anemia is usually permanent and life threatening. Half of all patients who do not respond to treatment die within one year following diagnosis.
-
Inherited bone marrow failure syndrome (genetics known and presumed).
-
Hereditary marrow failure syndromes.
-
Clonality of the stem cell compartment during evolution of myelodysplastic syndromes and other bone marrow failure syndromes.
-
Bone marrow section from a 7-year-old girl with idiopathic acquired aplastic anemia. Hematopoietic cells are almost totally absent. Sinuses and capillaries are prominent. Iron-laden macrophages reflecting increased iron stores from repeated RBC transfusions are present.
-
Findings in marrow failure syndromes.
-
Radiographic findings in marrow failure syndrome.