Practice Essentials
The use of the term folliculitis has been challenged for this disorder because hair follicles are not seen on the palms or the soles, which may be affected. Three variants of this disorder have been described: classic eosinophilic pustular folliculitis (as originally described by Ofuji), HIV-associated eosinophilic pustular folliculitis, and infantile eosinophilic pustular folliculitis. Some investigators prefer to consider these three distinct disorders. Of the three, the infantile variety is by far the least characterized. Because the exact nature of these conditions is unknown, whether these conditions are three interrelated forms of a single disease or three distinct dermatoses is unclear. These conditions share a common pathologic feature, namely a noninfectious eosinophilic infiltration of the hair follicles. A possible fourth subtype occurring 2-3 months after hematopoietic stem cell transplantation has been described in adults. [1]
 Widespread hyperpigmented patches on the back and the arms in a patient with eosinophilic pustular folliculitis. Courtesy of Professor T. Nishikawa, Department of Dermatology, Keio University School of Medicine, Tokyo, Japan.
Widespread hyperpigmented patches on the back and the arms in a patient with eosinophilic pustular folliculitis. Courtesy of Professor T. Nishikawa, Department of Dermatology, Keio University School of Medicine, Tokyo, Japan.
Signs and symptoms
The distribution tends to be a seborrheic one on the head and the trunk. About a fifth of patients have palmar and/or plantar plaques, which may be the first sign appearing weeks or months before other clinical features.
Lesions are less commonly pruritic with the classic type than in the other 2 forms.
Patients with eosinophilic pustular folliculitis in the classic form have chronically recurrent crops of sterile follicular papulopustules with peripheral extension and central clearing. [2, 3] Small papules tend to enlarge and coalesce into large plaques. [4] They may be acneiform. [5]
Papulopustules with or without plaques tend to favor the face and the trunk as shown below, although the extremities may also be involved. With the classic form, the palms and the soles may also be affected. In children, the scalp, particularly at the vertex, is most frequently involved.
 A patchy lesion on the cheek in a patient with eosinophilic pustular folliculitis. Courtesy of Professor T. Nishikawa, Department of Dermatology, Keio University School of Medicine, Tokyo, Japan.
A patchy lesion on the cheek in a patient with eosinophilic pustular folliculitis. Courtesy of Professor T. Nishikawa, Department of Dermatology, Keio University School of Medicine, Tokyo, Japan.
Some patients may have features of coexistent Ofuji disease and eosinophilic lymphoid granuloma (Kimura disease). [6]
Individual papulopustules may be larger in the classic form, up to 20-50 mm in diameter, rather than the 1-3 mm in diameter seen in patients with HIV disease and in infants; peripheral extension with central clearing may be much less frequent in these 2 forms than in the classic one, which often has an erythematous base. The latter tends to heal more commonly with postinflammatory hyperpigmentation.
No systemic involvement is evident, although a peripheral leukocytosis and eosinophilia may be seen. Atypical features, such as nonfollicular papules and urticarial plaques, are often evident in patients with HIV disease and in infants.
Diagnostics
Cytologic smears show abundant eosinophils.
In the classic form, mild-to-moderate leukocytosis and eosinophilia are often evident. The latter is seen in about one half of patients.
With HIV disease, the CD4 count is often less than 300 cells/µL.
Infants with this disorder may have an elevated serum immunoglobulin E level with reduced serum immunoglobulin G and immunoglobulin A levels and diminished neutrophil chemotactic activity.
Because childhood eosinophilic pustular folliculitis may be associated with AIDS, lymphoma, leukemia, and other hematologic diseases, a thorough systemic evaluation is indicated. [7]
Take skin swabs for microscopy and culture and scrapings for mycologic analysis when a microbial infection or superinfection is suspected.
Consider HIV- and non–HIV-related causes of immunodeficiency.
When vesicles predominate, perilesional skin may be examined with direct immunofluorescence, and serum may be evaluated with indirect immunofluorescence on healthy human skin and/or desmoglein 1/desmoglein 3 enzyme-linked immunosorbent assay to exclude pemphigus foliaceus or pemphigus vulgaris. Both of these conditions might initially be evident as pemphigus herpetiformis, thus looking like eosinophilic pustular folliculitis both clinically and histopathologically.
Histologic findings
Examine fresh, unexcoriated papulovesicles histologically, ideally in serial sections. Transverse sectioning may be needed if routine vertical sections give equivocal results as depicted below. Use routine hematoxylin and eosin stain as well as special stains for fungi and bacteria.
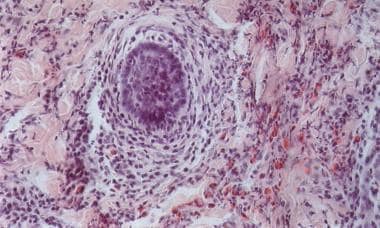 Transverse section from a 21-year-old man with eosinophilic pustular folliculitis. A perifollicular inflammatory infiltrate containing numerous eosinophils is present (hematoxylin and eosin, original magnification X400).
Transverse section from a 21-year-old man with eosinophilic pustular folliculitis. A perifollicular inflammatory infiltrate containing numerous eosinophils is present (hematoxylin and eosin, original magnification X400).
Subcorneal pustules of predominately eosinophils may be evident in the epidermis and the outer root sheath of hair follicles. Hair and sebaceous gland structures may be infiltrated with eosinophils, plus a few neutrophils and mononuclear cells (see the image below).
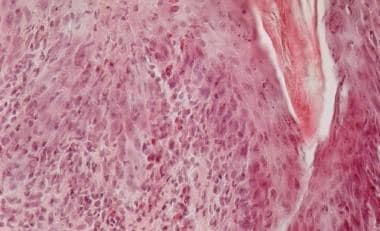 Vertical section from a 3-year-old girl with eosinophilic pustular folliculitis. A perifollicular inflammatory infiltrate containing eosinophils is present (hematoxylin and eosin, original magnification X200).
Vertical section from a 3-year-old girl with eosinophilic pustular folliculitis. A perifollicular inflammatory infiltrate containing eosinophils is present (hematoxylin and eosin, original magnification X200).
A patchy sebaceous lysis is observed in certain cases of HIV-related eosinophilic pustular folliculitis. Follicular eosinophilic abscesses are infrequently observed in HIV-associated cases of Ofuji disease. Infantile eosinophilic pustular folliculitis of the scalp may show an interfollicular dermal infiltrate with a substantial admixture of eosinophils and flame figures but not follicular spongiosis or degeneration.
Sometimes, mucin deposition can be observed in the hair follicles. Histopathologic study may reveal the coexistence of Ofuji disease and follicular mucinosis in patients with or without concomitant HIV infection. The lymphocytes in the HIV-associated type are predominately CD8+ lymphocytes.
Palmar and plantar plaques show subcorneal or intraepidermal eosinophilic abscesses and spongiosis. Small foci of acantholysis may be seen in individual cases of eosinophilic pustular folliculitis.
Management
Also see Medication.
A variety of options have been described with variable results.
In classic cases, common options for treatment include indomethacin (orally or topically) [8, 9] and its newer derivative acemetacin, [10] dapsone, topical and systemic steroids, isotretinoin, itraconazole, permethrin, interferon, and antibiotics. [11] The experience of Japanese dermatologists is that indomethacin is by far the most effective in the classic form, although the mode of its action in this disease is still poorly understood. [12] A multivariable analysis showed that females were more likely than males to exhibit a complete response to oral indomethacin. [13] Naproxen has also been used with some success. [14]
Narrowband UVB phototherapy may be effective. [15] Ultraviolet therapy with ultraviolet B or with ultraviolet A and psoralen plus ultraviolet A may be beneficial. [16, 17]
One may use topical itraconazole cream first in patients with HIV-associated disease, adding an oral sedating antihistamine for bedtime use if pruritus is severe. Cetirizine seems to be a favorite because of its preferential effect on eosinophils, [18] with some preferring 4 mg of cyproheptadine at bedtime.
In patients with HIV-associated disease, antiretroviral therapy tends to greatly diminish or even eliminate the severity of this disorder.
Some patients with HIV-associated Ofuji disease may respond to oral metronidazole.
Background
In 1965, Ise and Ofuji described a 42-year-old Japanese housewife with a possible follicular variant of subcorneal pustular dermatosis. [19] The patient had crops of follicular pustules on her back, face, chest, and upper arms representing histologic subcorneal pustulosis of the upper hair follicles as depicted below. The patient also had a leukocytosis of 14,100 white cells/µL, 8% of which were eosinophils. In 1970, Ofuji et al described 3 additional patients and proposed that this new entity be called eosinophilic pustular folliculitis (EPF). [20]
Pathophysiology
A histologic resemblance exists between eosinophilic pustular folliculitis and fungal folliculitis. Some investigators have speculated that eosinophilic pustular folliculitis is due to hyperreactivity to dermatophytes or saprophytic fungi, such as Pityrosporum ovale, in association with a disordered immune system. This concept is supported by the favorable therapeutic response of some patients to oral itraconazole therapy.
The follicle mite, Demodex, has also been considered a possible triggering agent. In certain patients, a combination of Pityrosporum species and Demodex species might play a role in the pathogenesis of the disease. An aberrant helper T-cell type 2 immune response to a follicular antigen, such as Demodex, might be involved in the pathogenesis of HIV-associated eosinophilic pustular folliculitis (see the image below). Eosinophilic pustular folliculitis has been described in atopic children [21] with hypersensitivity to Dermatophagoides pteronyssinus. Some authorities have suggested that patients with eosinophilic pustular folliculitis should be screened for the presence of coexisting Th2-mediated disorders. [22]
 A 51-year-old Japanese man without a concomitant HIV infection with pustular eosinophilic folliculitis. Courtesy of Professor Akimichi Morita, Nagoya City University Medical School, Nagoya, Japan.
A 51-year-old Japanese man without a concomitant HIV infection with pustular eosinophilic folliculitis. Courtesy of Professor Akimichi Morita, Nagoya City University Medical School, Nagoya, Japan.
An anaerobic organism similar in morphology to Leptotrichia buccalis has been found in one biopsy specimen of a patient with HIV-associated Ofuji disease; the disease responded to oral metronidazole. Others believe that at least the HIV-associated form is an autoimmune disorder with the sebaceous gland cell or a constituent of sebum serving as an autoantigen.
A single case has been reported of a patient with Ofuji disease with pemphiguslike antibody detected by direct immunofluorescence on both lesional skin and healthy skin and by indirect immunofluorescence on human skin but not on guinea pig esophagus. [23] Yet another patient with Ofuji disease and high titers of circulating immunoglobulin G and immunoglobulin M antibodies to the cytoplasm of the basal cells of the epidermis and the outer sheath of hair follicles has also been described. [24]
Another theory is that eosinophilic chemotactic factors from skin surface lipids may be involved. [25] A selective migration of leukocyte factor antigen-1–positive eosinophils and lymphocytes to hair follicles may be explained by intercellular adhesion molecule-1 expression by keratinocytes on follicular epithelium but not on epidermis. The expression of endothelial-leukocyte adhesion molecule-1 and vascular cell adhesion molecule-1 by vascular endothelium around hair follicles may also explain this migration. The overexpression of the interleukins (ILs)–36β, IL-36γ, and IL-36Ra, chemoattractive cytokines for eosinophils and neutrophils, is an important component of the inflammatory response of eosinophilic pustular folliculitis. [26]
Eosinophils infiltrating into the dermis and the follicular epidermis express neuronal nitric oxide synthase. [27] Activated eosinophils release major basic protein with subsequent tissue damage. In addition to degranulating eosinophils, degranulating mast cells are present in the skin of most patients with HIV-associated eosinophilic folliculitis, which suggests a role for both of these cell types in the pathogenesis of this disease.
Etiology
The cause of eosinophilic pustular folliculitis is unknown. Possible etiologies are discussed in Pathophysiology. Reports have described Asian patients in whom eosinophilic pustular folliculitis seemed to be associated with silicone tissue augmentation [28] or autologous peripheral blood stem cell transplantation. [1, 29]
A middle-aged Japanese woman has been described in whom eosinophilic pustular folliculitis was induced by a combination of allopurinol and timepidium bromide as suggested by the results of an oral provocation test with both drugs. [30] Moreover, allopurinol alone seemed to induce generalized eosinophilic pustular folliculitis. [31]
Eosinophilic pustular folliculitis associated with pregnancy has been described. [32, 33]
A middle-aged man with eosinophilic pustular folliculitis apparently associated with hepatitis C virus infection has also been reported. [22]
Hyperimmunoglobulin E syndrome may be evident as eosinophilic pustular folliculitis. [34] Other additional linkages of eosinophilic pustular folliculitis besides HIV infection include the Sézary syndrome and cutaneous angiosarcoma. [35, 36, 37]
Atypical eosinophilic pustular folliculitis was linked with use of the antimetabolite capecitabine. [38]
Eosinophilic folliculitis associated with wearing protective gear during the coronavirus disease 2019 (COVID-19) pandemic has been described. [39]
Epidemiology
Frequency
This is an uncommon disorder, except in the AIDS population. The peak incidence of the classic disease is in the second to fourth decades. The peak incidence is usually in the first year of life for the infantile form; eosinophilic pustular folliculitis may be congenital in infantile cases. [40] It may be seen at any age with HIV disease, with an incidence of almost 10% in one survey. Eosinophilic pustular folliculitis is most frequent in association with a low CD4 count.
Race
All races are affected. The classic form described by Ofuji mainly occurs in Japanese people in Japan. HIV infection is the most common medical condition associated with eosinophilic pustular folliculitis, at least in Whites.
Sex
Eosinophilic pustular folliculitis is more common in men than in women, although a survey confirmed these data for all but classic eosinophilic pustular folliculitis cases, in which the incidence was the same in both sexes. [41] With HIV disease, an overwhelming male prevalence exists.
Even in infants, the disease occurs more often in boys than in girls.
A male predominance was observed in those with extrafacial eosinophilic pustular folliculitis, with the immunosuppression-associated type more common among them. [42]
Prognosis
The main morbidity is chronic persistent pruritus, which, especially in the HIV-related form, can interfere with activities of daily living.
Unfortunately, the classic/Japanese form of this condition usually continues for years with recurrent relapses and remissions. Some patients have achieved long-lasting remissions with indomethacin alone or in combination with dapsone.
Patients with HIV-associated disease may benefit from highly active antiretroviral therapy. Treatment that restores immunity in individuals with HIV infection may clear their skin lesions, which otherwise are chronic and persistent. In the absence of improvement of the underlying immunodeficiency, HIV-associated eosinophilic folliculitis usually does not respond to any treatment; even with ultraviolet B and psoralen plus ultraviolet A phototherapy, the skin lesions recur on discontinuation of phototherapy.
Eosinophilic pustulosis of the scalp in infancy/childhood is a self-limited, albeit recurrent, dermatosis that can be relieved by topical corticosteroids.
-
A patchy lesion on the cheek in a patient with eosinophilic pustular folliculitis. Courtesy of Professor T. Nishikawa, Department of Dermatology, Keio University School of Medicine, Tokyo, Japan.
-
Widespread hyperpigmented patches on the back and the arms in a patient with eosinophilic pustular folliculitis. Courtesy of Professor T. Nishikawa, Department of Dermatology, Keio University School of Medicine, Tokyo, Japan.
-
A 51-year-old Japanese man without a concomitant HIV infection with pustular eosinophilic folliculitis. Courtesy of Professor Akimichi Morita, Nagoya City University Medical School, Nagoya, Japan.
-
Transverse section from a 21-year-old man with eosinophilic pustular folliculitis. A perifollicular inflammatory infiltrate containing numerous eosinophils is present (hematoxylin and eosin, original magnification X400).
-
Vertical section from a 3-year-old girl with eosinophilic pustular folliculitis. A perifollicular inflammatory infiltrate containing eosinophils is present (hematoxylin and eosin, original magnification X200).

