Practice Essentials
Multiple endocrine neoplasia type 1 (MEN1) is an endocrine tumor syndrome caused by inactivating mutations of the MEN1 tumor suppressor gene at the 11q13 locus. Although usually inherited as an autosomal dominant disorder, MEN1 can also occur sporadically (without a family history) as a result of new mutations.
MEN1 predisposes to the development of tumors in target neuroendocrine tissues. Type 2 multiple endocrine neoplasia (MEN2), in contrast, is caused by mutations in the RET proto-oncogene and typically presents as medullary thyroid carcinoma, hyperparathyroidism, or pheochromocytoma.
MEN1 is characterized by the combination of parathyroid tumors, pancreatic islet cell tumors, and anterior pituitary tumors (see the images below). Most MEN1 tumors are not aggressive, and many of them (particularly nonfunctioning tumors) follow a long-term indolent course, remaining asymptomatic for years. Nevertheless, patients with untreated MEN1 have a decreased life expectancy, with a 50% probability of death by age 50 years. [1, 2]
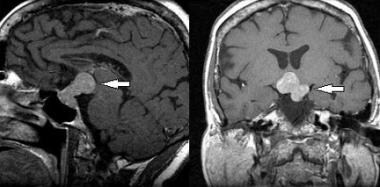 Multiple endocrine neoplasia type 1 (MEN1). Sagittal (left image) and coronal (right image), T1-weighted magnetic resonance images of the brain in a patient with MEN1 show a pituitary macroadenoma (arrows).
Multiple endocrine neoplasia type 1 (MEN1). Sagittal (left image) and coronal (right image), T1-weighted magnetic resonance images of the brain in a patient with MEN1 show a pituitary macroadenoma (arrows).
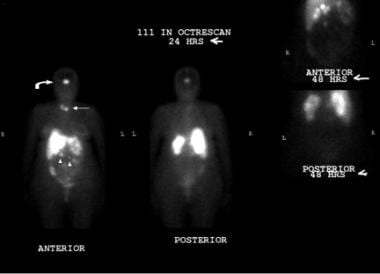 Multiple endocrine neoplasia type 1 (MEN1). Indium-111 (111In) octreotide scan in a patient with MEN1 demonstrates abnormal activity in the pituitary macroadenoma (curved arrow), parathyroid adenoma (straight arrow), and gastrinoma metastases throughout the abdomen (arrowheads).
Multiple endocrine neoplasia type 1 (MEN1). Indium-111 (111In) octreotide scan in a patient with MEN1 demonstrates abnormal activity in the pituitary macroadenoma (curved arrow), parathyroid adenoma (straight arrow), and gastrinoma metastases throughout the abdomen (arrowheads).
In 1954, Wermer was the first to describe the syndrome as a distinct clinical entity. The disorder was initially known as Wermer syndrome.
Pathophysiology
Parathyroid tumors
Primary hyperparathyroidism, due to hyperplasia and/or adenoma of parathyroid glands, is the most common manifestation of multiple endocrine neoplasia type 1 (MEN1) and occurs in approximately 90% of all patients. [3]
Primary hyperparathyroidism in MEN1 can have a long-term asymptomatic course and is usually diagnosed by the incidental finding of elevated serum parathyroid hormone level in a patient with hypercalcemia or, in some cases, with normocalcemia. Clinical manifestations can include hypercalcemia, nephrolithiasis, and bone abnormalities (osteitis fibrosa cystica). Common symptoms associated with hypercalcemia include polydipsia, polyuria, constipation, and generalized malaise.
Primary hyperparathyroidism in MEN1 differs from non-MEN1 primary hyperparathyroidism in the following ways [4] :
-
Earlier age at onset (20-25 years)
-
Involvement of multiple parathyroid glands
-
High recurrence rate of hypercalcemia after parathyroidectomy (50% by 8-12 years after surgery)
Pancreatic islet cell tumors (neuroendocrine tumors)
Pancreatic islet cell tumors represent the second most common manifestation of MEN1, occurring in 30-80% of patients. Islet cell tumors encompass the following [1] :
-
Gastrinomas
-
Glucagonomas
-
Vasoactive intestinal polypeptidomas (VIPomas)
-
Pancreatic polypeptidomas (PPomas).
Tumors are often multicentric and may undergo malignant transformation. These tumors can produce peptides and biogenic amines.
However, nonfunctioning pancreatic endocrine tumors are the most common enteropancreatic neuroendocrine tumor. Nonfunctioning tumors do not secrete hormone, or they may release hormonally inactive peptides such as pancreatic polypeptide (PP), chromogranin A, neurotensin, neuro-specific enolase, or ghrelin.
Especially small (< 2 cm) nonfunctional pNETs pose a challenge to treating physicians. The relatively recent availability and further increased use of sensitive radiological screening methods has allowed the diagnosis of these nonfunctional pancreatic tumors. These tumors are important to diagnose, since by the age of 80 the penetrance of pNETs is over 80% and metastatic disease is the most important cause of MEN1-related mortality. [5, 6]
Gastrinomas, seen in the image below, are the most common functional pancreatic neuroendocrine tumors and occur in 40-55% of patients. [7] The development of gastrinomas is preceded by multifocal hyperplasia of the gastrin-producing cells.
 Multiple endocrine neoplasia type 1 (MEN1). Computed tomography (CT) scan of the pancreas in a patient with MEN1 and a gastrinoma shows a pancreatic head mass (large, white arrow), as well as a low-attenuating lesion in the liver (small, black arrowhead) that indicates metastases. Note the calcifications of the right renal medullary pyramids (medullary nephrocalcinosis; black arrows) in this nonenhanced CT scan.
Multiple endocrine neoplasia type 1 (MEN1). Computed tomography (CT) scan of the pancreas in a patient with MEN1 and a gastrinoma shows a pancreatic head mass (large, white arrow), as well as a low-attenuating lesion in the liver (small, black arrowhead) that indicates metastases. Note the calcifications of the right renal medullary pyramids (medullary nephrocalcinosis; black arrows) in this nonenhanced CT scan.
Compared with non-MEN1 gastrinomas in Zollinger-Ellison syndrome (ZES), the gastrinomas in MEN1 are more often small (< 0.5 cm), multicentric, and located in the duodenum, thus diminishing the probability of surgical cure. The features predictive of poor prognosis include pancreatic location of lesions, metastases, ectopic Cushing syndrome, and height of gastrin levels.
About 20-30% of patients with ZES have MEN1. In MEN1 patients, ZES appears to develop only in those with primary hyperparathyroidism. [1] Longstanding MEN1 and ZES may lead to the development of gastric carcinoid tumors that may be aggressive. [8]
Insulinomas are the second most common functioning pancreatic neuroendocrine tumor in MEN1, developing at young age (< 35 years) in approximately 10-30% of patients. Insulinomas in MEN1 can manifest as single pancreatic macroadenoma (>2 cm) or, more commonly, as multiple microadenomas (< 2 cm) scattered along the entire pancreas. [9] Insulinomas (see the images below) can be multicentric and can metastasize either to regional lymph nodes or to the liver. [1]
 Multiple endocrine neoplasia type 1 (MEN1). Endoscopic ultrasonogram in a patient with an insulinoma. The hypoechoic neoplasm (arrows) is seen in the body of the pancreas anterior to the splenic vein (SV). (From: Rosch T, Lightdale CJ, Botet JF, et al. Localization of pancreatic endocrine tumors by endoscopic ultrasonography. N Engl J Med. Jun 25 1992;326(26):1721-6.)
Multiple endocrine neoplasia type 1 (MEN1). Endoscopic ultrasonogram in a patient with an insulinoma. The hypoechoic neoplasm (arrows) is seen in the body of the pancreas anterior to the splenic vein (SV). (From: Rosch T, Lightdale CJ, Botet JF, et al. Localization of pancreatic endocrine tumors by endoscopic ultrasonography. N Engl J Med. Jun 25 1992;326(26):1721-6.)
 Multiple endocrine neoplasia type 1 (MEN1). Computed tomography (CT) scan image with oral and intravenous contrast in a patient with biochemical evidence of insulinoma. The 3-cm contrast-enhancing neoplasm (arrow) is seen in the tail of the pancreas (P) posterior to the stomach (S) (From: Yeo CJ. Islet cell tumors of the pancreas. In: Niederhuber JE, ed. Current Therapy in Oncology. St. Louis, Mo: Mosby-Year Book; 1993: 272.)
Multiple endocrine neoplasia type 1 (MEN1). Computed tomography (CT) scan image with oral and intravenous contrast in a patient with biochemical evidence of insulinoma. The 3-cm contrast-enhancing neoplasm (arrow) is seen in the tail of the pancreas (P) posterior to the stomach (S) (From: Yeo CJ. Islet cell tumors of the pancreas. In: Niederhuber JE, ed. Current Therapy in Oncology. St. Louis, Mo: Mosby-Year Book; 1993: 272.)
Glucagonomas occur rarely (< 3%) in patients with MEN1 and can present silently or with hyperglycemia. Few patients show the typical skin lesions, known as necrolytic migratory erythema. Other presenting symptoms can be anemia, stomatitis, and weight loss, but these are often absent.
VIPomas occur in less than 1% of MEN1 patients. Presenting symptoms can include watery diarrhea, hypokalemia, and achlorhydria (WDHA syndrome). Tumors secreting pancreatic polypeptide (PPomas) may not produce clinical manifestations; alternatively, PPomas may be nonsecretory.
Growth hormone–releasing hormone tumors (GHRHomas) have been reported in patients with MEN1. GHRHomas most commonly arise in the lungs, followed by the pancreas and small intestine. [1]
Pituitary tumors
MEN1-associated anterior pituitary tumors most commonly secrete prolactin (60%), followed by tumors that secrete growth hormone (25%). Less than 5% secrete corticotropin and others are nonfunctional. [1] Compared with non-MEN1 pituitary tumors, MEN1 pituitary tumors tend to be larger (macroadenomas) and more aggressive, with a higher rate of infiltration of tumor cells into normal pituitary tissue. MEN1-associated pituitary tumors are less responsive to therapy. However, there is no distinct histological difference between MEN1 and non-MEN1 pituitary tumors. [10]
Other tumors associated with MEN1
Neuroendocrine (carcinoid) tumors can occur in patients with MEN1 and may be located in the bronchi, gastrointestinal tract, pancreas, and thymus. Thymic carcinoids associated with MEN1 are often nonfunctional and aggressive. [11] In women, bronchial carcinoids are most common. Carcinoids can actively secrete hormones such as serotonin, somatostatin, corticotropin, and growth hormone.
Cutaneous expression of MEN1 is common. Subcutaneous lipomas are found in one third of MEN1 patients. These lesions have loss of heterozygosity for band 11q12-12 and are associated with defective globular (G) protein function. Lipomas in MEN1 can also be retroperitoneal, visceral, or pleural. The presence of facial angiofibromas and collagenomas may allow presymptomatic diagnosis of MEN1 in relatives of diagnosed patients. [1]
Adrenal tumors occur in 20-40% of patients with MEN1. These tumors are most often benign and consist of nonfunctional cortical adenomas or diffuse or nodular hyperplasia. Adrenal cortical carcinomas are rare in MEN1 patients, but larger adrenal tumors (>1 cm) are more likely to undergo malignant transformation, so annual adrenal imaging in patients with known adrenal tumors is recommended. [1]
Thyroid adenomas occur in 5-30% of patients and have no specific MEN1-reported clinical significance. Meningiomas and other central nervous system tumors have been reported.
Thymic neuroendocrine tumor (TH-NET) is a rare but fatal component of MEN1 that accounts for almost 20% of MEN1-associated mortality. In a single-center study plus systematic review and meta-analysis, the pool estimate of TH-NET prevalence was 3.7%, with a male predominance of almost 4:1; male predominance and history of smoking were more common in American and European series compared with Asian reports. Median age at diagnosis was 43 years. [12]
Compared with the general population, females with MEN1 were found to have a 2-3 times higher risk for breast cancer at younger age and showed to have loss of heterozygosity (LOH) at the MEN1 locus [13]
Etiology
The putative gene for MEN1 has been localized to band 11q13 and codes for the menin protein. Menin is involved with regulation of transcription and genome stability. Loss of heterozygosity for this region is associated with MEN1, suggesting that the gene has tumor suppression function. Patients inherit one mutated copy of the gene and require a somatic mutation of the second copy for tumor development. MEN1 is an autosomal dominant disorder, but sporadic mutations also occur. A study from Italy that was based on a large MEN1 database identified 99 mutations, ranging from nonsense to missense and different slicing site mutations. [14]
Epidemiology
Random postmortem studies report a prevalence of multiple endocrine neoplasia type 1 (MEN1) of 0.25%. [1] However, in patients with clinical manifestations associated with MEN1, such as primary hyperparathyroidism, the reported prevalence is 1-18%. From 16-38% of patients harboring one or more gastrinomas have MEN1, and 3% of patients with pituitary tumors have MEN1. [15, 16]
The MEN1 gene has a high penetrance. By age 20 years, the gene is 50% penetrant and by age 40 years, 95% penetrant. Patients younger than 5 years have not been identified as manifesting the typical features associated with the MEN1 gene carrier status, and, thus, the gene is likely nonpenetrant before this age. [1, 3]
Mortality/Morbidity
Patients with multiple endocrine neoplasia type 1 (MEN1) have a decreased life expectancy, with a 50% probability of death by age 50 years. Half the deaths result directly from a malignant process or the sequela of an endocrine disorder. In a Dutch study, median survival in patients with an identified mutation in the MEN1 gene was estimated at 73 years, versus 87 years in mutation-negative patients diagnosed on the basis of having two of the three main MEN1 manifestations (primary hyperparathyroidism, duodenopancreatic neuroendocrine tumors, and pituitary tumors). [17]
Malignant pancreatic neuroendocrine tumors and thymic carcinoid tumors have been associated with a marked increase in the risk of death in MEN1 patients. [7] In a study of patients who underwent resection of a MEN1-related pancreatic neuroendocrine tumor, van Beek et al reported that the rate of liver metastases–free survival was significantly lower in patients with nonfunctioning tumors than in patients with insulinomas; estimated 10-year rates were 63% versus 87%, respectively. [18]
The rationale for an aggressive surveillance approach in MEN1 patients and asymptomatic carriers is based on the presumption that the early pre-symptomatic detection of MEN1 neoplasias may reduce the assoicated mortality. [1]
Individuals with MEN1 report a high degree of financial burden, negative financial events, and unemployment. All these factors were associated with worse health-related quality of life. Persistent hypercalcemia after parathyroid surgery was associated with higher levels of anxiety, depression, fatigue, and decreased social functioning. Patients diagnosed at a younger age (< 45 years) reported worse physical and social functioning. [19]
Race-, sex-, and age-related demographics
No racial differences have been found. The female-to-male incidence is approximately equal.
Age-related aspects of MEN1 include the following:
-
The peak incidence of symptoms in MEN1 is during the third decade of life in women and during the fourth decade of life in men. The reported age range is 5-81 years.
-
Hyperparathyroidism, the most common feature in MEN1, occurs at an earlier age (20-25 years) than in non-MEN1 patients (55 years).
-
MEN1-associated gastrinomas usually develop after age 30 years.
-
MEN1-associated insulinomas typicaly occur in those younger than 40 years but many have appeared in patients younger than 20 years.
-
Pituitary tumors and neuroendocrine tumors can occur as early as age 5 years.
-
In the study by de Laat et al, the median age for developing the first main MEN1 manifestation was 10 years later in mutation-negative than mutation-positive patients. [17]
-
Multiple endocrine neoplasia type 1 (MEN1). Sagittal (left image) and coronal (right image), T1-weighted magnetic resonance images of the brain in a patient with MEN1 show a pituitary macroadenoma (arrows).
-
Multiple endocrine neoplasia type 1 (MEN1). Indium-111 (111In) octreotide scan in a patient with MEN1 demonstrates abnormal activity in the pituitary macroadenoma (curved arrow), parathyroid adenoma (straight arrow), and gastrinoma metastases throughout the abdomen (arrowheads).
-
Multiple endocrine neoplasia type 1 (MEN1). Technetium-99m sestamibi scan (99mTc MIBI) in a patient with MEN1 demonstrates persistent abnormal activity of the inferior right parathyroid gland that is consistent with an adenoma.
-
Multiple endocrine neoplasia type 1 (MEN1). Computed tomography (CT) scan of the pancreas in a patient with MEN1 and a gastrinoma shows a pancreatic head mass (large, white arrow), as well as a low-attenuating lesion in the liver (small, black arrowhead) that indicates metastases. Note the calcifications of the right renal medullary pyramids (medullary nephrocalcinosis; black arrows) in this nonenhanced CT scan.
-
Multiple endocrine neoplasia type 1 (MEN1). Endoscopic ultrasonogram in a patient with an insulinoma. The hypoechoic neoplasm (arrows) is seen in the body of the pancreas anterior to the splenic vein (SV). (From: Rosch T, Lightdale CJ, Botet JF, et al. Localization of pancreatic endocrine tumors by endoscopic ultrasonography. N Engl J Med. Jun 25 1992;326(26):1721-6.)
-
Multiple endocrine neoplasia type 1 (MEN1). Computed tomography (CT) scan image with oral and intravenous contrast in a patient with biochemical evidence of insulinoma. The 3-cm contrast-enhancing neoplasm (arrow) is seen in the tail of the pancreas (P) posterior to the stomach (S) (From: Yeo CJ. Islet cell tumors of the pancreas. In: Niederhuber JE, ed. Current Therapy in Oncology. St. Louis, Mo: Mosby-Year Book; 1993: 272.)
-
Multiple endocrine neoplasia type 1 (MEN1). Anteroposterior radiographic view of the right hand in a patient with MEN1 and primary hyperparathyroidism shows subperiosteal bone resorption along the radial aspects of the middle phalanges (arrows).
-
Multiple endocrine neoplasia type 1 (MEN1). Bilateral, anteroposterior radiographic views of the hands in a patient with MEN1 and primary hyperparathyroidism show subperiosteal bone resorption along the radial aspects of the middle phalanges.






