Overview
The oral cavity represents the first part of the digestive tube. Its primary function is to serve as the entrance of the alimentary tract and initiate the digestive process by salivation and propulsion of the alimentary bolus into the pharynx. [1, 2] It also serves as a secondary respiratory conduit, a site of sound modification for the production of speech, and a chemosensory organ. [2]
The mobility of the lips is also critical to speech production, whistling, singing, playing of wind and brass musical instruments, expectoration, and human behavioral communication (e.g., kissing, smiling, pouting, baring of teeth). [2] Even minor disruptions in the function of the oral cavity can seriously jeopardize an individual's quality of life. [2]
The oral cavity (see the image below) is oval shaped and is separated into the oral vestibule and the oral cavity proper. [3]
-
Oral vestibule - The slit-like space between the lips, cheeks, and the teeth or gums. [4]
-
Oral cavity proper - The region bounded anteriorly by the teeth and gums and extending posteriorly to the oropharyngeal isthmus. [4]
The oral cavity is bound by the lips anteriorly, the cheeks laterally, the floor of the mouth inferiorly, the oropharynx posteriorly, and the palate superiorly. [1] The oropharynx begins superiorly at the junction between the hard palate and the soft palate and inferiorly behind the circumvallate papillae of the tongue. [5] The bony base of the oral cavity is represented by the maxillary and mandibular bones. [6]
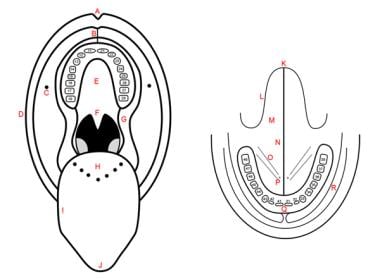 Schematic representation of oral cavity and floor of mouth. A: philtrum; B: upper labial frenulum; C: opening of Stensen's duct; D: labial commissure; E: hard palate; F: soft palate; G: intermaxillary commissure; H: base of tongue; I: lateral border of tongue, dorsal view; J: tip of tongue, dorsal view; K: tip of tongue, ventral view; L: lateral border of tongue, ventral view; M: ventral surface of tongue; N: lingual frenulum; O: floor of mouth; P: opening of Wharton's duct; Q: vestibular gingiva; R: vestibule. Teeth are numbered according to international classification.
Schematic representation of oral cavity and floor of mouth. A: philtrum; B: upper labial frenulum; C: opening of Stensen's duct; D: labial commissure; E: hard palate; F: soft palate; G: intermaxillary commissure; H: base of tongue; I: lateral border of tongue, dorsal view; J: tip of tongue, dorsal view; K: tip of tongue, ventral view; L: lateral border of tongue, ventral view; M: ventral surface of tongue; N: lingual frenulum; O: floor of mouth; P: opening of Wharton's duct; Q: vestibular gingiva; R: vestibule. Teeth are numbered according to international classification.
The oral cavity includes the lips, gingivae, retromolar trigone, teeth, hard palate, cheek mucosa, mobile tongue, and floor of the mouth. The major salivary glands are in close relation with oral cavity structures, although they are not part of the oral cavity. The tongue is part of the oral cavity; its anatomy is specifically described elsewhere (see Tongue Anatomy). The palatine tonsils, soft palate, tongue base, and posterior pharyngeal walls are part of the oropharynx; the oropharynx is not part of the oral cavity.
Gross Anatomy: Oral Vestibule
The oral vestibule is bounded externally by the lips and the cheeks and internally by the alveolar processes and the teeth. When the teeth are in occlusion, the vestibule communicates with the oral cavity proper via the intermaxillary commissure behind the last molar teeth.
The vestibule is shaped like a horseshoe and includes features such as the buccal and labial sulci. These sulci are formed by reflections of oral mucosa from the alveolar processes onto the cheeks and lips, creating gutters that are clinically significant during dental procedures. [7, 8]
The vestibule plays a role in containing food during mastication, aided by muscles such as the buccinator which helps keep food between the teeth. It also houses the opening of the parotid duct opposite the upper second molar, which secretes saliva into this space. [7, 8]
Lips
The longer upper lip and shorter lower lip are connected to each other by the labial commissures at the corners of the mouth. The lips are separated from the cheeks by the nasolabial fold. [1] The lip has an interior pale wet vermilion and an outer darker dry vermilion, separated from each other by a red line; there is also a white line on the outside which is purely a cutaneous part of the lip (see the image below). [6]
The upper lip features a central depression called the philtrum, bordered by symmetrical paramedian vertical ridges known as philtral ridges. These structures are supported by unique dermal collagen and dense elastic tissue. The inferior margin of the philtrum forms part of the cupid's bow, with a fleshy prominence referred to as the tubercle or procheilon. [9]
The orbicularis oris muscle plays a critical role in lip movement and expression. It forms part of the structural support for both lips and contributes to their shape and function during speech and eating. [9]
Cheeks (mucosa)
The cheeks are a musculomembranous structure and are limited superiorly and inferiorly by the upper and lower vestibules, anteriorly by the labial commissure, and posteriorly by the retromolar trigone and the intermaxillary commissure. [6] The inner surface of each lip is connected in the middle line to the corresponding gum by a fold of mucous membrane, the labial frenulum. The upper labial frenulum (see the first image below) is larger than the lower labial frenulum (see the second image below). [10]
The retrocommissural region is situated between the labial commissure and the opening of Stensen's duct (the drainage duct of the parotid gland), located opposite the second upper molar (see the images below). Stensen's duct runs through the buccinator muscle. A horizontal slightly elevated streak (called the linea alba or occlusal line) traverses this region level with the biting plane. [6]
 Opening of Stensen's duct opposite second upper molar (arrow). Asterisk indicates retromolar trigone.
Opening of Stensen's duct opposite second upper molar (arrow). Asterisk indicates retromolar trigone.
The buccinator muscle forms the muscular framework of the cheek and is also a muscle of facial expression. It is covered by the buccal fat pad, which smoothens the cheek contour by filling in the depression and the anterior border of the masseter. The masseter muscle covers the buccinator. [1] Other muscles also contribute to the formation of the cheek such as the zygomaticus, risorius, and platysma. [10]
Gums and alveolar process
The gingiva (or gum) is a fibroepithelial mucosal tissue that surrounds the teeth and covers the alveolar jawbone. The gingiva is composed of oral epithelium, sulcular epithelium, and junctional epithelium. The junctional epithelium is essential for maintaining the attachment between the teeth and the gums. It acts as a barrier to both mechanical trauma and microbiological insult, contributing to the innate immune response in periodontal tissues. [11]
The alveolar process, also known as the alveolar bone, is an essential component of the jaw that houses the tooth sockets (alveoli) in both the maxilla and mandible. It is composed of two main parts: the alveolar bone proper — lining the tooth sockets — and the supporting alveolar bone. The alveolar bone proper is a primarily compact bone and is referred to as the lamina dura when viewed radiographically. This compact bone contains numerous small openings, known as Volkmann's canals, which allow for vascular communication between the alveolar bone and periodontal ligament (PDL). [12] The alveolar process is the tooth-bearing area of the jaws. It is composed of a dense outer cortex (known as the cortical plate) and looser inner trabecular (or medullary) bone. The area of the cortical bone that lines the dental socket (or alveolus) is called the lamina dura.
The alveolar process is covered by gums within the mouth and terminates roughly along the line of the mandibular canal. It is composed of a compact bone, also called the cribriform plate due to its perforations, and a trabecular (or medullary) bone. The cortical plates of the compact bone are found on the facial and lingual surfaces of the alveolar bone and are thicker around the posterior teeth compared with the anterior teeth. [12]
The alveolar bone consists of approximately 65% inorganic material by weight, primarily calcium hydroxyapatite crystals. The remaining 35% is organic material composed of collagenous and noncollagenous proteins. Cellular components include osteoblasts, osteocytes, and osteoclasts, which are involved in bone formation and remodeling. [12]
The integrity of the alveolar process is crucial for dental health as it provides structural support for teeth. Bone remodeling in this area involves a balance between resorption by osteoclasts and formation by osteoblasts. [12]
Retromolar trigone
The retromolar trigone is a small triangular-shaped subsite of the oral cavity. It is the portion of mucosa that lies behind the third molar tooth, covering the anterior ramus of the mandible. The base of the triangle is posterior to the last inferior molar tooth; the apex is in continuity with the tuberosity of the maxilla behind the last upper molar tooth. The retromolar trigone is bounded laterally by the gingival buccal sulcus and medially by the anterior tonsillar pillar.
Studies have highlighted the presence of minor salivary glands within this region, termed the "retromolar gland." These glands are bound by structures such as the superior pharyngeal constrictor muscle and the tendon of the buccinator muscle. They are not continuous with adjacent spaces such as the pterygomandibular or parapharyngeal spaces, although they are separated from the surrounding structures by loose connective tissue. [13]
The retromolar trigone's anatomical location makes it significant in clinical contexts, particularly in relation to oral cavity cancers. Tumors originating in this area tend to be aggressive due to their proximity to critical structures such as the mandible and maxilla, often necessitating comprehensive treatment approaches, including surgery and radiotherapy. [14]
Teeth
The teeth are calcified structures whose main purpose is mastication. Each tooth is composed of a crown, which is the exposed portion above the gumline, and a root, which is embedded in the jawbone.
Deciduous teeth (also referred to as primary or temporary teeth) are the first to emerge in the oral cavity and are progressively replaced by permanent (or adult) dentition. There are 20 deciduous teeth, comprising eight molars, four canines (or cuspids), and eight incisors. The permanent dentition consists of 32 teeth: 12 molars (including four so-called wisdom teeth or third molars), eight premolars (or bicuspids), four canines, and eight incisors.
Incisors have a thin occlusal edge, a somewhat flat crown, and a single root. Their main purpose is to cut food. Canines have a pointed shape and a single long root. Their main function is to pierce and tear food.
The occlusal (or masticatory) surface of molars and premolars is characterized by pointed structures named cusps. Premolars usually have one or two cusps and one or two roots. Molars usually have 4-5 cusps and 2-3 roots, the shape of which is highly variable. The purpose of molars and premolars is to grind and crush food.
Gross Anatomy: Oral Cavity Proper
Hard palate
The palate is the horseshoe-shaped, domed roof of the oral cavity. It is divided into a hard portion and a soft portion. The hard palate belongs to the oral cavity and separates it from the nasal cavities. The soft palate belongs to the oropharynx and separates it from the nasopharynx.
The hard palate is concave, and this concavity is occupied mostly by the tongue when it is at rest. The hard palate is subdivided into the primary and secondary palates. [15] The primary palate is separated from the secondary palate by a small depression behind the central incisors termed the incisive fossa, where the incisive foramen opens.
The anterior two third portion of the hard palate is formed by the incisive bone — premaxilla — and the palatine processes of the maxilla. The horizontal plates of the palatine bone form the posterior third. The secondary palate presents a midline elevated suture line termed the median or palatine raphe. The hard palate also has transverse ridges (or rugae) on the anterior third that serve to retain the food bolus. [15, 3]
Soft palate
The soft palate marks the beginning of the oropharynx and is the movable posterior third of the palate. It forms an incomplete septum between the mouth and the pharynx. It is marked by a median raphe and is continuous with the roof of the mouth and the mucous membrane of the nasal floor (see the image below).
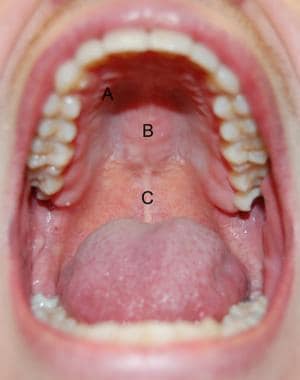 Hard and soft palates. A: transverse rugae of hard palate; B: median raphe of hard palate; C: median raphe of soft palate.
Hard and soft palates. A: transverse rugae of hard palate; B: median raphe of hard palate; C: median raphe of soft palate.
When the soft palate is relaxed, its anterior surface is concave and its posterior surface is convex. The anterior aponeurotic portion is attached to the posterior border of the hard palate, and the posterior muscular portion hangs between the mouth and the pharynx and is termed the palatine velum (or velopharynx). [10, 15]
The velum is prolonged by a median-free process termed the uvula and two bilateral processes termed the palatoglossal and palatopharyngeal arches or pillars, which join the soft palate to the tongue and pharynx, respectively. [15] The fauces represents the space between the cavity of the mouth and the oropharynx. They are bounded superiorly by the soft palate, inferiorly by the root of the tongue, and laterally by the pillars of the fauces.
The palatine tonsils are located in the tonsillar sinuses (or fossae) of the oropharynx, which is bounded by the palatoglossal and palatopharyngeal arches and the tongue. They are thoroughly described elsewhere (see Tonsil and Adenoid Anatomy). [15]
While swallowing, the soft palate is initially tensed to squeeze the bolus of food between the tongue and the pharynx before it is elevated so as to block the nasal passages while the bolus is propelled into the pharynx. [15]
Floor of the mouth
The floor of the mouth forms the inferior limit of the oral cavity. It is often compared to a quadrangular pyramid with a posterior base. Superficially, it is separated into three zones: the anterior floor of the mouth located anterior to the lingual frenulum and the two sublingual folds located between the lateral tongue and the mandibular gingiva. [6]
The sublingual papillae (also referred to as caruncles or folds) can be identified on both sides of the frenulum in the anterior part of the floor of mouth when the tip of the tongue is raised (see the image below). [15] The excretory duct of the submandibular gland (Wharton's duct) runs in the floor of the mouth along the medial border of the sublingual gland to pierce the surface of the mouth at the paramedian sublingual caruncle. The sublingual glands have multiple small ducts that drain directly into the floor of the mouth. [6] The mylohyoid and geniohyoid muscles form a muscular sling that supports other structures in this area. The mylohyoid muscle separates the sublingual space above from the submandibular space below. [16]
Tongue and major salivary glands
The tongue is a mobile muscular organ that occupies a major part of the oral cavity and part of the oropharynx. Its main functions are pushing food into the oropharynx during swallowing and forming words while speaking, although it is also involved in mastication, taste, and oral cleansing. [15] The macroscopic and microscopic anatomy, musculature, nerve supply, and vasculature of the tongue are specifically addressed elsewhere (see Tongue Anatomy).
The major salivary glands are large paired exocrine glands that communicate with the mouth and pour their secretions into its cavity. They comprise the parotid, submandibular (or submaxillary), and sublingual glands.
Microscopic Anatomy
Because food is physically broken down in the oral cavity, this region is lined by a protective, nonkeratinized, stratified squamous epithelium, which also lines the inner surface of the lips. [17] The oral cavity proper is lined by a masticatory mucosa (gingiva and hard palate), a lining mucosa (lips, cheeks, alveolar mucosal surface, floor of the mouth, inferior surface of the tongue, and soft palate), and a specialized mucosa (dorsal surface of the tongue). The histologic structure of the tongue is addressed elsewhere (see Tongue Anatomy). [18]
Lips
The outer lip (outer vermilion) is lined with skin. The epidermis is composed of stratified squamous, keratinized epithelium, which provides a protective barrier. This layer lacks sweat and sebaceous glands, which is why the lips can become dry more easily. [19] Beneath the epidermis, the dermis is composed of sebaceous glands, hair follicles, sweat glands, arrector pili muscles, and the neurovascular bundle on the lip periphery. [17] However, it is important to note that the vermilion border itself lacks these glands. [19]
The inner lip (interior vermilion) is lined with a stratified squamous, nonkeratinized epithelium. Under the epithelium is a lamina propria, the counterpart of the dermis. Tubuloacinar labial glands are found in the submucosa. These are predominantly mucous; their secretion moistens the oral mucosa, and their small ducts open into the oral cavity. [17]
The core of the lip contains fibers of the striated orbicularis oris muscle. [17] It is a striated skeletal muscle responsible for lip movements such as puckering and closing. This muscle interacts with surrounding muscles such as the zygomaticus major and depressor anguli oris to assist in expressions, speech, and feeding. [19]
The lips are richly supplied with blood vessels, which contribute to their color and are involved in thermoregulation. The labial arteries are significant in this regard. With age, there can be changes such as thinning of the epidermal layer and loss of collagen and elastin in the dermis. These changes contribute to reduced elasticity and volume of the lips over time. [19]
Cheeks
Lining mucosa is found on the cheeks. It covers the striated muscle and major salivary glands. The epithelium of the lining mucosa is nonkeratinized, although it can be parakeratinized in some places. Parakeratinized epithelium is similar to keratinized epithelium, except that the superficial cells do not lose their nuclei.
The nonkeratinized lining epithelium is thicker than keratinized epithelium. It consists of a stratum basale (a single layer of cells on basal lamina), a stratum spinosum (several cells thick), and a stratum superficiale (the most superficial layer). The cells of the mucosal epithelium include keratinocytes, Langerhans cells, melanocytes, and Merkel cells. [18]
The underlying lamina propria is a thick papillary layer of loose connective tissue that contains blood vessels, nerves that send axon endings into the epithelium, and encapsulated sensory endings in some papillae. The lining mucosa has fewer and shorter papillae so that it can adjust to the movement of its underlying muscles. [18]
The distinct submucosa of the lining mucosa contains large bands of collagen and elastic fibers that bind the mucosa to the underlying muscles. It also contains many minor salivary glands of the lips, tongue, and cheeks, which are predominantly mucous. The submucosa contains the larger blood vessels, nerves, and lymphatics that supply the lamina propria. [18]
Teeth
The teeth are composed of four distinct and unique tissues.
Enamel: This is the outermost layer covering the crown of the tooth. Enamel is the hardest and most mineralized tissue in the human body, composed primarily of hydroxyapatite crystals. It is acellular, which contributes to its inability to regenerate once damaged, but is exceptionally resistant to wear and decay. It is structured into enamel rods, which are tightly packed, rod-shaped units extending from the dentin-enamel junction (DEJ) to the surface. [20]
Pulp: The central portion of each tooth is composed of the second tissue, the pulp. The pulp is a fibrovascular tissue containing odontoblasts whose purpose is innervation, vascularization, and repair.
Dentin: Beneath the enamel and around the pulp lies the dentin, which makes up the bulk of each tooth. It is less mineralized than enamel but more so than bones, containing about 70% hydroxyapatite, 20% organic material (predominantly collagen), and 10% water. The dentin consists of calcified tissue containing numerous microscopic channels known as dentinal tubules, which harbor odontoblastic processes. These tubules contribute to dentin's sensitivity and play a role in reparative mechanisms. [21]
Cementum: The fourth dental tissue, cementum, consists of a thin layer of calcified tissue covering the dental root. The apical portion of the tooth is covered by cellular cementum, whereas the remainder is covered by acellular cementum. The PDL fibers embedded in the cementum are known as Sharpey's fibers and are crucial for tooth stability within the jawbone. Cementum contains collagen and is similar in composition to bones, although it lacks vascularization. [22]
DEJ is a vital interface where mechanical stresses are absorbed. it is uniquely structured to resist crack propagation, with enamel rods oriented perpendicularly to enhance its strength. Studies have highlighted the role of DEJ in distributing forces and preventing enamel fractures by redirecting cracks into dentin, which possesses greater toughness owing to crack bridging mechanisms. [23]
Gums and alveolar process
The gums are lined with masticatory mucosa. This mucosa has a keratinized and, in some areas, a parakeratinized stratified squamous epithelium. The underlying lamina propria contains blood vessels and nerves (sensory receptors and Meissner's corpuscles). The lamina propria is rich in collagen fibers, cells, and ground substance, with fibroblasts being the predominant cell type. These fibroblasts are crucial in the formation of collagen fibers and ground substance present in the connective tissue. [24]
Deep to the lamina propria is a reticular layer of dense connective tissue. The reticular layer blends with the periosteum; thus, no submucosa exists. [18]
The gingiva receives its blood supply primarily from supraperiosteal vessels, which are complemented by vessels from the PDL and interdental septa. The gingival plexus, a network of postcapillary venules, extends from the coronal to apical termination of the junctional epithelium. [25]
The alveolar mucosal surface consists of lining mucosa covering the alveolar bone. This structure provides attachment for Sharpey's fibers, part of the PDL, which are inserted at right angles into the bone. These fibers are thicker in diameter than those in the cementum. [26, 27]
The alveolar bone comprises both cortical and trabecular bone. Cortical bone forms plates on the facial and lingual surfaces of the alveolar bone, while trabecular bone includes cancellous bone located between these cortical plates. The alveolar crest is slightly apical to the cementoenamel junction and maintains uniform height along healthy jaws. [26, 27]
Hard and soft palate
The hard palate is also lined with masticatory mucosa. In the palatine raphe, the mucosa also adheres firmly to the periosteum, and no submucosa exists. In the other regions of the hard palate, a submucosa that contains thick collagenous bands extending from the mucosa to the bone underlies the lamina propria. The submucosa contains adipose tissue anteriorly and mucous glands posteriorly. [18]
The soft palate is covered with lining mucosa similar to that described above.
Floor of the mouth
The floor of the mouth is covered with lining mucosa similar to that described above.
Minor salivary glands
The basic structure of a salivary gland is that of a branching duct that has the principal secretory cells (the acinar cells) at the proximal ends of the branches and an opening into the oral cavity at the other end of a single collecting duct. Four morphologically and functionally varying segments exist in each basic salivary gland unit: acinus, intercalated duct, striated duct, and excretory duct. Two types of cells exist in each segment: abluminal cells and luminal cells.
Abluminal cells are myoepithelial cells in the acinus and intercalated duct and basal cells in the striated and excretory ducts. Acinar cells may be serous or mucinous, depending on the chemical composition of the saliva produced by a specific gland. Parotid glands are mostly serous, submandibular glands are mixed (predominantly serous), sublingual glands are mixed (predominantly mucous), and minor salivary glands are mixed (predominantly mucous), except in the palate, where the glands are mostly mucinous, and in the tongue (see below). [28]
The oral cavity is scattered with 500-1000 minor salivary glands within the mucosa and submucosa of the cheeks, lips, floor of the mouth, hard and soft palates, retromolar trigone, and tongue; the anterior hard palate and gingivae are devoid of these glands.
The lobules of the minor salivary glands are 1-5 mm in size and are separated from one another by connective tissue. Glands in the posterior hard palate are more numerous and more confluent. Most lobules have individual excretory ducts that open into the oral cavity, but they are not usually perceptible. [28]
In the tongue, lips, and buccal mucosa, lobules of the salivary gland tissue are located beneath the mucosal epithelium and within the deeper skeletal muscles. These glands are unencapsulated. [28]
The posterior hard palate contains pure mucous type acini without serous cells. In the tongue, Blandin and Nunn glands are located on the anterior ventral portion and are of the mucinous type. The posterior dorsal and lateral portions contain serous glands called von Ebner glands. [28]
Musculature of Mastication
Movements of the mandible are mainly produced by the four muscles of mastication: the masseter, temporalis, lateral pterygoid, and medial pterygoid muscles. All these muscles come from the mesoderm of the first pharyngeal arch, and their innervation is therefore supplied by the anterior trunk of the mandibular nerve (cranial nerve V3). [15]
The masseter is a quadrangular muscle that has a deep part and a superficial part. The deep portion originates from the inferior surface of the zygomatic arch and descends almost vertically to insert onto the lateral surface of the ramus. The superficial portion arises from the zygomatic bone anterior to the temporozygomatic suture and descends inferiorly and posteriorly to insert onto the angle of the mandible. The main action of the masseter is mandibular elevation. Some superficial fibers also have a limited role in mandibular protrusion. [29]
The temporalis is a broad triangular muscle that originates from the floor of the temporal fossa and from the deep surface of the temporal fascia. It inserts on the tip and medial surface of the coronoid process and on the anterior border of the ramus of the mandible. Its main action is to elevate the mandible. Some horizontal fibers are also involved in mandibular retraction. [15]
The lateral pterygoid muscle is a two-headed triangular muscle that has two distinct origins: the infratemporal surface and crest of the greater wing of the sphenoid and the lateral surface of the lateral pterygoid plate. The upper head inserts onto the joint capsule and articular disc of the temporomandibular joint. The inferior head attaches to the anteromedial aspect of the neck of the condyle. The bilateral contraction of this muscle causes protraction of the mandible and depression of the chin. Unilateral contraction moves the jaw contralaterally. [15]
The medial pterygoid muscle is also a two-headed muscle; it originates from the medial surface of the lateral pterygoid plate and the pyramidal process of the palatine bone and from the maxillary tuberosity. It inserts onto the medial surface of the ramus of the mandible. Its main role is mandibular elevation, in synergy with the masseter muscle. It also contributes to mandibular protrusion. [15]
Mandibular depression is mainly produced by gravity. The suprahyoid and infrahyoid muscles, whose chief roles are to raise and depress the hyoid bone and the larynx, respectively, may also participate in mandibular depression. [15]
Blood Supply and Lymphatic Drainage
Blood is supplied to the oral vestibule and oral cavity via branches of the external carotid artery (facial, maxillary, and lingual). The terminal branches of the arteries often anastomose freely, including anastomoses across the midline with their contralateral partners. [15]
The facial artery provides the major arterial supply to the lips. It branches out into the superior and inferior labial arteries 1 cm lateral to the corner of the mouth. The superior labial artery supplies the upper lip. The inferior nasal artery supplies the lower lip. These arteries anastomose with each other to form an arterial ring.
The angular artery, a terminal branch of the facial artery, supplies the superior part of the cheek. [15] The facial vein provides venous drainage to the lips. It joins with a communication of the retromandibular vein to form the common facial vein and terminates in the internal jugular vein at the level of the hyoid bone. [15]
The maxillary artery is the larger of the two terminal branches of the external carotid and supplies the cheek mucosa, teeth, gingivae, and palate. It arises behind the mandibular neck and is at first embedded in the substance of the parotid gland. As it emerges, it is divided into three portions: mandibular, pterygoid, and pterygopalatine. [15]
The mandibular portion of the maxillary artery gives off the inferior alveolar artery, which enters the mandible and supplies the mandibular teeth, chin, and mylohyoid muscle. [15]
The pterygoid portion branches out into the masseteric artery, which supplies the masseter; the deep temporal arteries, which supply the temporalis muscle; the pterygoid branches, which supply the pterygoid muscles; and the buccal artery, which supplies the buccal fat pad, buccinator, and buccal oral mucosa. [15]
The pterygopalatine portion of the maxillary artery branches into the posterior superior alveolar artery, the infraorbital artery, the artery of the pterygoid canal, the pharyngeal branch, the descending palatine artery, and the sphenopalatine artery.
The posterior superior alveolar artery supplies the maxillary molar and premolars and the adjacent gingiva. The infraorbital artery supplies the maxillary canines and incisors and the skin of the infraorbital region of the face. The descending palatine artery descends through the palatine canal and divides into the greater and lesser palatine arteries to supply the mucosa and glands of the hard and soft palate. The sphenopalatine artery traverses the sphenopalatine foramen to supply the anteriormost palate. [15]
The deep facial vein, which originates from the pterygoid venous plexus, drains most of the areas supplied by the maxillary artery. It enters the posterior aspect of the facial vein, which terminates in the internal jugular vein. [15]
The lingual artery, its branches, and the lingual veins provide circulation to the tongue and the floor of the mouth. All the lingual veins terminate, directly or indirectly, in the internal jugular vein after merging into the common trunk for lingual and facial veins. [15]
All lymphatics from the head and neck drain directly or indirectly into the deep cervical lymph nodes. Lymph from these nodes then drains into the jugular lymphatic trunk, which joins the thoracic duct on the left side and the internal jugular vein or brachiocephalic vein on the right side. [15]
The skin of the cheeks drains to parotid and submandibular lymph nodes. [29] The upper lip and the lateral parts of the lower lip drain to the submandibular lymph nodes. Lymph from the central part of the lower lip drains to the submental lymph nodes. [15] Lymph from the mucous membrane of the cheek drains to the submandibular nodes and the upper deep cervical nodes. Superficial cervical nodes may also be involved.
Both surfaces of the lower gingivae and the outer surface of the upper gingivae drain into the submandibular lymph nodes. The inner surface of the upper gums is drained with the vessels of the hard and soft palates to the upper deep cervical lymph nodes. The floor of the mouth drains via lymphatics that pierce the mylohyoid muscle to reach the submental nodes anteriorly or the submandibular nodes posteriorly. [29]
Innervation
Sensory innervation to the lips, cheeks, gingivae, teeth, hard palate, and floor of the mouth is provided by the trigeminal nerve (cranial nerve V), more specifically the maxillary (V2) and mandibular (V3) divisions of this nerve. Branches of V3 also supply the four muscles of mastication, but the motor innervation of the buccinator and orbicularis oris muscles is supplied by the buccal branch of the facial nerve (VII). [15]
In the upper jaw, the buccal and gingival mucosa are supplied by both the maxillary and mandibular divisions; in the lower jaw, they are supplied only by the mandibular division. [29]
The maxillary nerve (V2) leaves the cranium through the foramen rotundum in the sphenoid and enters the pterygopalatine fossa, where it gives off branches to the pterygopalatine ganglion and enters the inferior orbital fissure. It gives off the zygomatic nerve and passes into the infraorbital groove as the infraorbital nerve. [15]
The posterior and middle superior alveolar nerves arise from the maxillary nerve, and the anterior superior alveolar nerve arises from the infraorbital nerve. These nerves supply the maxillary molars. The gingival branch arises from the posterior superior alveolar nerve and supplies the mucosa of the gingiva and that of the cheek near the upper molars. [15]
The infraorbital branch of the maxillary nerve gives off palatine branches. This nerve also supplies the mucosa of the upper lip and labial vestibule. [15]
The mandibular nerve (V3) descends through the foramen ovale into the infratemporal fossa and divides into the auriculotemporal, inferior alveolar, lingual, and buccal nerves.
The inferior alveolar nerve enters the mandibular foramen, passes through the mandibular canal, and forms the inferior dental plexus. The inferior dental plexus sends branches to all mandibular teeth on its side. The mental nerve is another branch of the plexus that supplies the skin and mucous membrane of the lower lip and the vestibular gingiva of the mandibular incisors. The lingual nerve lies anterior to the inferior alveolar nerve and provides sensory innervation to the floor of the mouth and the lingual gingiva. [15]
Natural Variants
Fordyce granules
Fordyce granules are visible sebaceous glands that are not associated with hair follicles. They can sometimes be found in the submucosa lateral to the corner of the mouth and in the cheeks opposite the molar teeth.
Torus
Torus palatinus and torus mandibularis are benign bony outgrowths of the palate and mandible (see the image below). Tori of the oral cavity occur in 3-56% of adults and are more common in women, Asians, and Inuits. They usually manifest in the second decade and continue to grow throughout life.
Torus palatinus is found in the midline of the hard palate, and torus mandibularis is found on the lingual surface of the anterior mandible, primarily in the premolar region. Patients with tori are asymptomatic unless the torus interferes with denture placement or eating. Treatment is reserved for symptomatic patients and is accomplished by surgical removal from underlying cortical bone with osteotomes or burrs. Tori may recur, and malignant transformation has not been described. [30]
Pathophysiologic Variants
Premalignant lesions
Oral cancer is more likely to occur in leukoplakia and erythroplakia (see the image below). Both conditions are diagnoses of exclusion, representing, respectively, a white patch and a fiery red patch that cannot be categorized as any other disease. (See Premalignant Conditions of the Oral Cavity.)
Squamous cell carcinoma
Oral cavity cancers, most of which are squamous cell carcinomas, account for around 3% of all cancers (see the image below). In some regions of the world, such as Southeast Asia, they account for up to 30-40% of all malignancies. Most affected patients are middle-aged or older men. Alcohol and tobacco use are widely accepted risk factors, and there is increasing evidence on the role of human papillomavirus (HPV) in the development of this disease. Despite advances in treatment, 5-year survival rates still hover around 50-60%. [30]
Cleft lip and palate
Cleft lip and palate are among the most common congenital anomalies. Cleft lip and palate occur approximately once every 1000 Caucasian births, and isolated cleft palate occurs once every 2000 births. Kernohan's classification is the system that is most widely used to classify cleft lip and palate according to disease severity.
Cleft lip may be unilateral or bilateral. Cleft palate may be complete, with extension into the nasal cavity, or submucosal, with a preserved palatal mucosa. The primary cleft palate is anterior to the incisive foramen, and the secondary cleft palate is posterior to it. Isolated cleft palates may be associated with syndromes such as Pierre-Marie-Robin sequence, Stickler syndrome, Treacher-Collins syndrome, Apert syndrome, 22q11 anomalies, and many others.
Feeding assistance, airway compromise, and middle ear disease must be evaluated. Patients can be treated surgically at approximately 3 months of age for the lip and at 12 months for the palate. [30]
Tumors of minor salivary glands
Salivary gland neoplasms make up 6% of all head and neck tumors and most commonly appear in the sixth decade of life (see the image below). Most salivary gland tumors arise in the parotid and submandibular glands, and fewer than 10% of tumors arise in the minor salivary glands. Most minor salivary gland tumors are malignant, usually manifesting as painless masses on the palate or floor of the mouth. Diagnosis is made through fine-needle aspiration biopsy, and the primary treatment is surgical.
-
Schematic representation of oral cavity and floor of mouth. A: philtrum; B: upper labial frenulum; C: opening of Stensen's duct; D: labial commissure; E: hard palate; F: soft palate; G: intermaxillary commissure; H: base of tongue; I: lateral border of tongue, dorsal view; J: tip of tongue, dorsal view; K: tip of tongue, ventral view; L: lateral border of tongue, ventral view; M: ventral surface of tongue; N: lingual frenulum; O: floor of mouth; P: opening of Wharton's duct; Q: vestibular gingiva; R: vestibule. Teeth are numbered according to international classification.
-
Lips. Arrow indicates red line, which separates dry vermilion from wet vermilion.
-
Upper vestibule (upper lip everted). Arrow indicates upper labial frenulum.
-
Lower vestibule (lower lip everted). Arrow indicates lower labial frenulum.
-
Opening of Stensen's duct opposite second upper molar (arrow). Asterisk indicates retromolar trigone.
-
Linea alba (arrow).
-
Hard and soft palates. A: transverse rugae of hard palate; B: median raphe of hard palate; C: median raphe of soft palate.
-
Floor of mouth. A: lingual frenulum; B: sublingual papillae.
-
Torus palatinus.
-
Leukoplakia on the soft palate.
-
Squamous cell carcinoma of the floor of mouth.
-
Pleomorphic adenoma of the hard palate.
-
Mouth of 3-year-old patient. Bottom of mouth is bordered by tongue. Superior border of mouth is hard and soft palate. Lateral aspects of mouth are inside linings of cheeks. Cheeks contain ducts that empty saliva of parotid glands into mouth. If tongue is lifted, floor of mouth is visible with ducts that empty saliva of submandibular glands into mouth. Video courtesy of Dr. Ravi Elluru.










