Practice Essentials
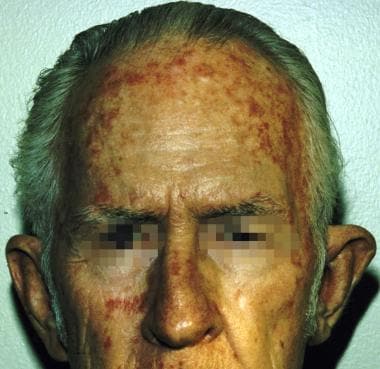
Actinic keratosis (AK) is an ultraviolet (UV) light–induced skin lesion that may progress to invasive squamous cell carcinoma (SCC). It is by far the most common lesion with malignant potential to arise on the skin. Actinic keratosis is seen in fair-skinned persons on skin areas that have had long-term sun exposure. [1] In Australia, the country with the highest skin cancer rate in the world, the prevalence of actinic keratosis among adults older than 40 years has been reported to range from 40-60%. In the United States, actinic keratosis represents the second most frequent reason for patients to visit a dermatologist. [2, 3] See the image below.
An actinic keratosis may follow 1 of 3 paths: It may regress, persist unchanged, or progress to invasive SCC. The percentage that progress to invasive SCC remains unknown, and estimates have varied from as low as 0.1% to as high as 10%. [4, 5]
A study by Criscione and colleagues of 7784 actinic keratoses in a high-risk population found that nearly 65% of primary SCCs and 36% of primary basal cell carcinomas arise from clinically diagnosed actinic keratoses. Furthermore, risk of progression of actinic keratosis to SCC was 0.60% at 1 year and 2.57% at 4 years, which is 6-8 times more frequent than had been reported in some prior studies. [6]
Although it is impossible to predict which course an individual lesion will follow, most patients have many lesions, so assessing risk becomes more significant and aids in tailoring treatments. Overall, actinic keratoses can be safely and effectively eradicated, and, therefore, therapy is warranted.
Signs and symptoms
Actinic keratoses develop as follows:
-
The lesions begin as small, rough spots that are easier felt than seen and that have what is often described as a sandpaperlike texture [7]
-
With time, the lesions enlarge, usually becoming red and scaly
The typical patient with actinic keratoses is an elderly, fair-skinned, sun-sensitive person. [10] The lesions arise in areas of long-term sun exposure, including the face and ears, and bald scalp in men, as well as the dorsal forearms and hands. [1, 11]
Patients may develop multiple lesions within a single anatomic site, to the extent that the lesions coalesce and produce confluent actinic keratosis over a relatively large area. The following variants can occur [12] :
-
Brown (pigmented actinic keratosis)
-
Atrophic
-
Bowenoid
-
Lichen planus–like
-
Exaggerated hyperkeratosis - Produces a hornlike projection, known as a cutaneous horn, above the skin surface
The image below is a typical depiction of actinic keratosis.
See Presentation for more detail.
Diagnosis
Histology
A skin biopsy is indicated to confirm the diagnosis and to rule out invasive SCC for suspicious or more advanced lesions (ie, those with more pronounced hyperkeratosis, increased erythema, or induration or nodularity). [13, 14] A biopsy is also indicated for recurrent lesions or those that are unresponsive to therapy.
Actinic keratosis is characterized by dysplasia and architectural disorder of the epidermis, as follows [7] :
-
Abnormal keratinocytes of the basal layer that are variable in size and shape
-
Altered cellular polarity
-
Nuclear atypia
-
Hyperkeratosis and parakeratosis of the epidermis
-
Irregular acanthosis may be present
In general, hair follicles, sebaceous glands, and apocrine and eccrine ducts are not involved. [7]
Fluorescence
Fluorescence with the use of a photosensitizing drug (methyl ester of 5-aminolevulinic acid [ALA], a precursor of protoporphyrin) commonly used in photodynamic therapy (PDT) has been described as a diagnostic tool for actinic keratosis. [15] Areas of involvement, including occult areas of abnormal skin, emit a pink fluorescence with a Wood lamp or PDT lamp. [15]
See Workup for more detail.
Management
Treatment consists of the following categories:
-
Medical therapy - including pharmacologic treatment and PDT
-
Surgical destruction of the lesion
Pharmacologic treatment
Medications approved by the US Food and Drug Administration (FDA) for the treatment of actinic keratosis include the following [16, 17, 18] :
-
Topical 5-fluorouracil (5-FU)
-
Imiquimod cream
-
Topical diclofenac gel
-
Tirbanibulin ointment
Photodynamic therapy
PDT uses a light-sensitizing compound that preferentially accumulates in actinic keratosis cells, where it can be activated by the appropriate wavelength of light. Delta-aminolevulinic acid is a component of the heme biosynthetic pathway that accumulates preferentially in dysplastic cells. Once inside these cells, it is enzymatically converted to protoporphyrin IX, a potent photosensitizer. With exposure to light of an appropriate wavelength, oxygen free radicals are generated and cell death results. [19]
Surgery
Types of surgery used in the eradication of actinic keratoses include the following [20, 21, 22] :
-
Cryosurgery
-
Curettage, shave excision, and conventional excision - For lesions suggestive of invasive cancer
-
Cosmetic resurfacing procedures - Including medium and deep chemical peels, dermabrasion, and ablative laser resurfacing
See Treatment and Medication for more detail.
Pathophysiology
Actinic keratoses most often arise on fair-skinned people in areas of long-term sun exposure, such as the face, ears, bald scalp, forearms, and backs of the hands. [1] However, they may occur on any area that is repeatedly exposed to the sun, such as the back, the chest, and the legs. Long-term UV light exposure is implicated as the cause from both epidemiologic observations and molecular analysis of tumor cells. [1, 23]
Actinic keratosis frequency correlates with cumulative UV exposure. [1] Therefore, the frequency of actinic keratosis increases with each decade of life, is greater in residents of sunny countries closer to the equator, and is greater in persons with outdoor occupations. [10, 1] DNA analysis of the cells within actinic keratoses shows characteristic UV-induced mutations in key genes, including TP53 and deletion of the gene coding for p16 tumor suppressor protein. [23, 24, 25]
Development of actinic keratoses may occur as early as the third or fourth decade of life in patients who live in areas of high solar radiation, are fair-skinned, and do not use sunscreen for photoprotection. [1] Usually, patients demonstrate a background of solar-damaged skin, with telangiectasias, elastosis, and pigmented lentigines. [7]
In both histologic and molecular parameters, actinic keratoses share features with squamous cell carcinoma, [26] and over time, a small percentage of actinic keratoses may transform into invasive squamous cell carcinoma. According to one study of almost 7000 patients, the length of time for this transformation to occur was approximately 2 years. [27]
Actinic keratosis is an epidermal lesion characterized by aggregates of atypical, pleomorphic keratinocytes at the basal layer that may extend upwards to involve the granular and cornified layers. [26] The epidermis itself shows an abnormal architecture, with acanthosis, parakeratosis, and dyskeratosis. Cellular atypia is present, and the keratinocytes vary in size and shape; mitotic figures are present. [26] This presentation may resemble Bowen disease or carcinoma in situ, and the distinction between the two is a matter of degree (extent of the lesion) rather than differences in individual cells. [26]
Etiology
As the term "actinic" indicates, actinic keratoses are induced by UV light. Both epidemiologic observations and molecular biologic characteristics of the tumor cells suggest that UV light is sufficient by itself to induce actinic keratosis. [23, 25] Sensitivity to UV light is inherited; actinic keratoses occur more frequently in fair, redheaded, or blonde patients who burn frequently and tan poorly. [1] Increased sun exposure and higher-intensity exposure increase the chance of actinic keratosis development. Immunosuppression following organ transplantation dramatically increases the risk of developing actinic keratoses [28] ; however, actinic keratoses do not occur without sun exposure.
Additional studies have shown an association between cutaneous human papillomavirus and actinic keratosis. [29, 30, 31] The role of human papillomavirus in skin tumorigenesis was discovered the 1950s, and the group of known human papillomavirus types associated with skin tumorigenesis has been classified as beta-papillomavirus. [30]
Beta-papillomavirus DNA has been identified in healthy skin and in squamous cell carcinoma, basal cell carcinoma, and actinic keratosis. A 2007 study suggested that only a small association exists between beta-papillomavirus and actinic keratosis; however, persons with beta-papillomavirus infection plus age over 60 years, fair skin, or high sun exposure had markedly higher risk for actinic keratoses than persons without the combination of beta-papillomavirus infection with any of those risk factors. [30]
Epidemiology
United States
Actinic keratosis occurs primarily in Whites, and the frequency correlates with cumulative UV exposure [1] and therefore with age, proximity to the equator, and outdoor occupation. Actinic keratoses are seen more often in men than in women and have also been correlated with a high-fat diet. [10, 32] Overall, the rate in the United States population is estimated to range from 11-26%. [3]
International
The prevalence is highest in Australia, where much of the population is light-skinned and outdoor sports are very popular activities. [33] Overall, actinic keratosis is estimated to be present in 40-60% of the Australian population older than 40 years. [3]
Although in Korea the incidence of actinic keratosis is not as high as among Whites, it has been increasing from 17.9 to 54.0 per 100,000 person-years between 2006 and 2015 with higher prevalence among older populations (1.95 per 10,000 persons in individuals in their 40s compared to 31.81 per 10,000 persons in individuals in their 80s). Because Korea is a fast-aging society, the incidence of actinic keratosis is expected to continue to increase in the future. [34]
Race
The prevalence of actinic keratosis is much higher in individuals with fair skin and blue eyes and is lower in individuals with darker skin types. [10] Actinic keratosis is relatively nonexistent in Black skin. [35] Patients with actinic keratoses tend to have Fitzpatrick type I or II skin, which burns and does not tan. [1] The prevalence is reduced precipitously in persons with Fitzpatrick types III, IV, and V skin and is nonexistent in those with Fitzpatrick type VI skin. [35] Although the incidence of cutaneous malignancies in darker-skinned individuals is much lower than in White persons, UV exposure may still play a role in the etiology of squamous and basal cell carcinoma; screening and sun safety education should still be promoted because cutaneous malignancies in darker-skinned individuals can be very aggressive. [35]
Sex
The prevalence of actinic keratosis is higher in men than in women. [1] This is theorized to result from a greater likelihood that men have an outdoor occupation and thus have greater cumulative UV exposure. [10]
Age
One of the most important determinants of actinic keratosis risk is age, particularly in combination with other strong predictors, including cumulative sun exposure, place of birth, occupation, and skin type. [10, 1] Actinic keratoses can occur in persons aged 20-30 years, but they are more common in those aged 50 years and older. [1]
Prognosis
The prognosis for actinic keratosis is good. With continuing surveillance and treatment, these lesions can be managed individually. Lesions begin as barely perceivable rough spots of skin, better felt than seen. [7, 15] Early lesions feel like sandpaper; later lesions become erythematous, scaly plaques that may enlarge to several centimeters. [7, 1] Lesions may remain unchanged for years, may spontaneously regress, or may progress to invasive squamous cell carcinoma. [4, 5]
Most actinic keratoses do not progress to invasive squamous cell carcinoma; however, most invasive squamous cell carcinomas have evidence of a preexisting actinic keratosis. [1, 5] Invasive squamous cell carcinoma may produce significant morbidity by direct extension into facial structures. In less than 10% of cases, invasive squamous cell carcinoma may metastasize, with a low 5-year survival rate. [36, 37] Development into invasive squamous cell carcinomas can be prevented by aggressive therapy and sun protection. However, the prognosis in a person with long-term exposure is more guarded because of the multitude of their lesions.
Patients with extensive involvement unresponsive to cryosurgery and topical therapy may benefit from skin resurfacing by dermabrasion, [22] chemical peeling, or laser resurfacing. [21]
Patient Education
Instruct patients to practice sun safety, such as the use of sunscreen and protective clothing, and to limit outdoor activity from 10 AM to 3 PM. [38]
-
Actinic keratosis. Courtesy of Hon Pak, MD.
-
Actinic keratosis during treatment with topical 5-fluorouracil. Courtesy of Hon Pak, MD.
-
Actinic keratosis right after treatment with topical 5-fluorouracil. Courtesy of Hon Pak, MD.
-
Erythematous, scaly lesions on the temple area, typical of actinic keratosis.