Background
Globe rupture occurs when the integrity of the outer membranes of the eye is disrupted by blunt or penetrating trauma. Any full-thickness injury to the cornea, sclera, or both is considered an open globe injury and is approached in the same manner in the acute setting. Globe rupture is an ophthalmologic emergency and requires definitive management by an ophthalmologist. Although the globe's position within the orbit protects it from injury in many situations, damage to the posterior segment of the eye is associated with a very high frequency of permanent visual loss. Prompt recognition and ophthalmologic intervention are essential to maximizing functional outcome. [1, 2]
Globe rupture secondary to trauma is shown in the image below.
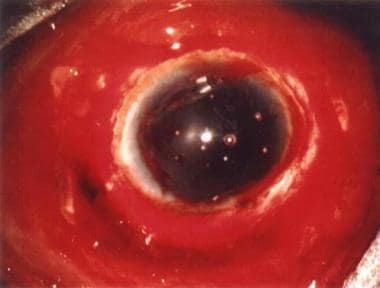 Operating microscope view of a globe rupture secondary to blunt trauma by a fist. Notice the dark arc in the bottom of the photo representing the ciliary body visible through the scleral breach. Subconjunctival hemorrhage of this severity should raise suspicion of occult globe rupture. Photo courtesy of Brian C Mulrooney, MD.
Operating microscope view of a globe rupture secondary to blunt trauma by a fist. Notice the dark arc in the bottom of the photo representing the ciliary body visible through the scleral breach. Subconjunctival hemorrhage of this severity should raise suspicion of occult globe rupture. Photo courtesy of Brian C Mulrooney, MD.
Pathophysiology
Globe rupture may occur when a blunt object impacts the orbit, compressing the globe along the anterior-posterior axis causing an elevation in intraocular pressure to a point that the sclera tears. [3] The rupture site most commonly is near the globe’s equator posterior to the insertion of the rectus muscles, which is where the sclera is weakest and thinnest. [4] Sharp objects or those traveling at high velocity may perforate the globe directly. Small foreign bodies may penetrate the eye and remain within the globe. The possibility of globe rupture should be considered and ruled out during the evaluation of all blunt and penetrating orbital traumas as well as in all cases involving high-speed projectiles with potential for ocular penetration.
Epidemiology
Frequency
United States
More than 2 million eye injuries occur in the United States annually, with more than 40,000 resulting in some degree of permanent visual impairment. Trauma to the eye represents approximately 3% of all ED visits in the United States. [5] Approximately 34% of ophthalmic presentations in the emergency department are related to trauma, whereas the remaining 66% are unrelated to injury. [6] Anterior lacerations causing open globe injuries are most common in men (80%). Globe ruptures are most common in women (70%) and usually caused from falls [7] .
Mortality/Morbidity
Globe rupture and posterior segment injury have always been associated with a high frequency of visual loss. Approximately 30-40% of monocular blindness cases result from ocular trauma. [8] With modern diagnostic techniques, surgical approaches, and rehabilitation, many eyes can be salvaged with retention of vision. [9]
Patients should not be given a hopeful prognosis until full, usually operative, evaluation is complete. Achieving or maintaining useful vision depends on several prognostic factors, such as the severity of the initial trauma, involvement of ocular structures, preoperative visual acuity, and timely diagnosis and treatment. [10]
Race
No racial predilection exists for globe rupture.
Sex
Because of occupational and recreational preferences, most globe rupture injuries are found in men (78.6%). [11] Men are more likely to experience penetrating injuries (69.9%), whereas women present more often with blunt globe rupture (68.1%). [11] Anterior lacerations causing open globe injuries are most common in men (80%). Globe ruptures are most common in women (70%) and usually caused from falls [7] .
Age
Globe rupture typically occurs at a younger age in men (median age, 36 y) than in women (median age, 73 y). [11]
A high percentage of globe rupture occurrences are in adolescent boys.
Children < 5 have poorer visual outcomes with open globe injuries. [7] .
Prognosis
The prognosis depends largely on the extent of injury and the time from injury until appropriate surgical treatment.
In a study by Lee et al, the charts of 62 patients aged 16 years and younger who had been treated for open globe injuries were reviewed. [12] In addition to location and extent of injury, unfavorable outcomes were also related to the initial presentation of hyphema, vitreous hemorrhage, retinal detachment, cornea wound across the pupil, and endophthalmitis.
In a retrospective review, Esmaeli et al studied 176 cases of ruptured globe to identify clinical and histopathologic factors that may predict ocular survival and final visual acuity after penetrating ocular trauma. Predictors of excellent final visual acuity (20/60 or better) were initial visual acuity of 20/200 or better, wound location anterior to the plane of insertion of the 4 rectus muscles, wound length 10 mm or less, and sharp mechanism of injury. Poor visual acuity at first visit, rupture globe, zone III injuries, history of penetrating keratoplasty, retinal detachment, vitreous hemorrhage, and dislocation of crystalline lens were found to be poor prognostic factors. [10]
The prognosis should be guarded until after surgical evaluation.
Patient Education
For patient education resources, see the Eye and Vision Center, as well as Subconjunctival Hemorrhage (Bleeding in Eye).
-
Operating microscope view of a globe rupture secondary to blunt trauma by a fist. Notice the dark arc in the bottom of the photo representing the ciliary body visible through the scleral breach. Subconjunctival hemorrhage of this severity should raise suspicion of occult globe rupture. Photo courtesy of Brian C Mulrooney, MD.





