Practice Essentials
In 2018, 28.9 million adults (11.6%) were diagnosed with sinusitis. [1] Approximately 2.7 million visits to physician offices with chronic sinusitis as the primary diagnosis occurred in 2018. [2] Acute bacterial rhinosinusitis (ABRS) accounts for 1 in 5 antibiotic prescriptions for adults, making it the fifth most common reason for an antibiotic prescription. Approximately 6-7% of children with respiratory symptoms have acute rhinosinusitis. An estimated 16% of adults are diagnosed with ABRS annually. Given the clinical nature of this diagnosis, there is a possibility of overestimation. An estimated 0.5 to 2.0% of viral rhinosinusitis (VRS) will develop into bacterial infections in adults and 5 to 10% in children. [3]
The number of emergency department visits with chronic sinusitis as the primary diagnosis in 2018 was 234,000. [4]
Sinusitis is characterized by inflammation of the lining of the paranasal sinuses. Because the nasal mucosa is simultaneously involved, and because sinusitis rarely occurs without concurrent rhinitis, rhinosinusitis is the preferred term for this condition. It is more common in females, and the highest incidence is between ages 45 to 64 years.
Signs and symptoms
Clinical findings in acute sinusitis may include the following:
-
Pain over cheek and radiating to frontal region or teeth, increasing with straining or bending down
-
Redness of nose, cheeks, or eyelids
-
Tenderness to pressure over the floor of the frontal sinus immediately above the inner canthus
-
Referred pain to the vertex, temple, or occiput
-
Postnasal discharge
-
A blocked nose
-
Persistent coughing or pharyngeal irritation
-
Facial pain
-
Hyposmia
Symptoms of acute bacterial rhinosinusitis include the following:
-
Facial pain or pressure (especially unilateral)
-
Hyposmia/anosmia
-
Nasal congestion
-
Nasal drainage
-
Postnasal drip
-
Fever
-
Cough
-
Fatigue
-
Maxillary dental pain
-
Ear fullness/pressure
The diagnosis of acute bacterial sinusitis should be entertained under either of the following circumstances:
-
Presence of symptoms or signs of acute rhinosinusitis 10 days or more beyond the onset of upper respiratory symptoms
-
Worsening of symptoms or signs of acute rhinosinusitis within 10 days after an initial improvement
The following signs may be noted on physical examination:
-
Purulent nasal secretions
-
Purulent posterior pharyngeal secretions
-
Mucosal erythema
-
Periorbital edema
-
Tenderness overlying sinuses
-
Air-fluid levels on transillumination of the sinuses (60% reproducibility rate for assessing maxillary sinus disease)
-
Facial erythema
Diagnosis
Acute sinusitis is a clinical diagnosis. However, the evaluation might include the following laboratory tests [5] :
-
Nasal cytology
-
Nasal-sinus biopsy
-
Tests for immunodeficiency, cystic fibrosis, or ciliary dysfunction
Nasal cytology examinations may be useful to elucidate the following entities:
-
Allergic rhinitis [6]
-
Eosinophilia
-
Nasal polyposis
-
Aspirin sensitivity
Tests for immunodeficiency are indicated if history findings indicate recurrent infection; they include the following:
-
Immunoglobulin studies
-
HIV serology
Cultures are not routinely obtained in the evaluation of acute sinusitis but should be obtained in the following cases:
-
Patients in intensive care or with immunocompromise
-
Children not responding to appropriate medical management
-
Patients with complications of sinusitis
In adults, cultures are directed at the middle meatus. Aspiration of the sinus by direct antral puncture is the only accurate way to obtain a culture but is reserved for patients with any of the following:
-
Life-threatening illness
-
Immunocompromise
-
Disease unresponsive to therapy
Computed tomography scanning is the preferred imaging method for rhinosinusitis. A complete sinus CT scan with frontal and coronal planes is used if an alternative diagnosis (eg, tumors) must be excluded. CT scanning is characteristic in allergic fungal sinusitis and is one of the major criteria for diagnosis.
Management
Treatment of acute sinusitis consists of providing adequate drainage of the involved sinus and appropriate systemic treatment of the likely bacterial pathogens. Drainage can be achieved surgically with sinus puncture and irrigation techniques. Options for medical drainage are as follows:
-
Oral alpha-adrenergic vasoconstrictors (eg, pseudoephedrine, and phenylephrine) for 10-14 days
-
Topical vasoconstrictors (eg, oxymetazoline hydrochloride) for a maximum of 3-5 days
Antibiotic treatment usually is given for 14 days. Usual first-line therapy is with one of the following:
-
Amoxicillin, at double the usual dose (80-90 mg/kg/d), especially in areas with known Streptococcus pneumoniae resistance
-
Clarithromycin
-
Azithromycin
Second-line antibiotic should be considered for patients with any of the following:
-
Residence in communities with a high incidence of resistant organisms
-
Failure to respond within 48-72 hours of commencement of therapy
-
Persistence of symptoms beyond 10-14 days
The most commonly used second-line therapies include the following:
-
Amoxicillin-clavulanate
-
Second- or third-generation cephalosporins (eg, cefuroxime, cefpodoxime, cefdinir)
-
Macrolides (ie, clarithromycin)
-
Fluoroquinolones (eg, ciprofloxacin, levofloxacin, moxifloxacin)
-
Clindamycin
Antibiotic selection with respect to previous antibiotic use and disease severity is as follows:
-
Adults with mild disease who have not received antibiotics: Amoxicillin/clavulanate, amoxicillin (1.5-3.5 g/day), cefpodoxime proxetil, or cefuroxime is recommended as initial therapy.
-
Adults with mild disease who have had antibiotics in the previous 4-6 weeks and adults with moderate disease: Amoxicillin/clavulanate, amoxicillin (3-3.5 g), cefpodoxime proxetil, or cefixime is recommended.
-
Adults with moderate disease who have received antibiotics in the previous 4-6 weeks: Amoxicillin/clavulanate, levofloxacin, moxifloxacin, or doxycycline is recommended.
Symptomatic or adjunctive therapies may include the following:
-
Humidification/vaporizer
-
Warm compresses
-
Adequate hydration
-
Smoking cessation
-
Balanced nutrition
-
Nonnarcotic analgesia
Background
Sinusitis is characterized by inflammation of the lining of the paranasal sinuses. Because the nasal mucosa is simultaneously involved and because sinusitis rarely occurs without concurrent rhinitis, rhinosinusitis is the preferred term for this condition. [7]
Rhinosinusitis may be further classified according to the anatomic site (maxillary, ethmoidal, frontal, sphenoidal), pathogenic organism (viral, bacterial, fungal), presence of complication (orbital, intracranial), and associated factors (nasal polyposis, immunosuppression, anatomic variants).
Acute sinusitis is a clinical diagnosis; thus, an understanding of its presentation is of paramount importance in differentiating this entity from allergic or vasomotor rhinitis and common upper respiratory infections. No specific clinical symptom or sign is sensitive or specific for acute sinusitis, so the overall clinical impression should be used to guide management.
The primary goals of management of acute sinusitis are to eradicate the infection, decrease the severity and duration of symptoms, and prevent complications. Most patients with acute sinusitis are treated in the primary care setting. Further evaluation by an otolaryngologist is recommended in any of the following cases:
-
When continued deterioration occurs with appropriate antibiotic therapy
-
When episodes of sinusitis recur
-
When symptoms persist after 2 courses of antibiotic therapy
-
When comorbid immunodeficiency, nosocomial infection, or complications of sinusitis are present
Definition of acute rhinosinusitis
Many classifications, both clinical and radiological, have been proposed in the literature to define acute sinusitis. Although no consensus on the precise definition exists, subacute sinusitis represents a temporal progression of symptoms for 4-12 weeks. Recurrent acute sinusitis is diagnosed when 2-4 episodes of infection occur per year with at least 8 weeks between episodes and, as in acute sinusitis, the sinus mucosa completely normalizes between attacks. [8] Chronic sinusitis is the persistence of insidious symptomatology beyond 12 weeks, with or without acute exacerbations. [9]
Anatomy
To properly diagnose and treat infectious disorders of the paranasal sinuses, the clinician should have knowledge of the developmental milestones. The development of the paranasal sinuses begins in the third week of gestation and continues until early adulthood.
Development of paranasal sinuses
During the third week of embryonic development, proliferation and medial migration of ectodermal cells form the notochord. After the heart tube and pericardium have rotated from the cranial position to lie anteriorly, the notochord, which initially is in the caudal region of the embryonic disc, rotates to lie posterior to the primitive foregut. The paraxial layer of mesenchyme, which lies adjacent to the notochord, differentiates into the somite ridges, intermediate cell mass, and lateral plate mesoderm. From these mesodermal structures, the branchial arches develop, the first of which gives rise to internal nasal structures.
The paranasal sinuses develop in conjunction with the palate from changes in the lateral wall of the nasal cavity. At 40 weeks' gestation, 2 horizontal grooves develop in the mesenchyme of the lateral wall of the nasal cavity. Proliferation of maxilloturbinate mesenchyme between these grooves results in an outpouching of tissue medially into the nasal lumen. This outpouching is the precursor of the middle and inferior meatus as well as the inferior turbinate. Ethmoidoturbinate folds develop superiorly to give rise to the middle and superior turbinates. Once the turbinate structures are established, sinus development begins and continues until early adult life.
The sinuses open into the nose via small openings called ostia. [10] The maxillary and ethmoid sinuses form at 3-4 months' gestation. Thus, an infant is born with 3-4 ethmoid cells and tiny teardrop-shaped maxillary sinuses. By the teenage years, each maxillary sinus progressively enlarges to an adult capacity of 15 mL. In healthy individuals, the ethmoid sinuses increase in number to 18-20, and each drains by an individual ostium that is 1-2 mm in diameter.
The frontal sinus develops from an anterior ethmoid cell and moves to its supraorbital position when the individual is aged 6-7 years. Frontal sinuses may begin to develop at this age but usually do not appear radiologically until the individual is aged approximately 12 years. The maxillary, anterior ethmoid, and frontal sinuses drain into the middle meatus; the posterior ethmoid and sphenoid sinuses drain into the superior meatus (see the image below).
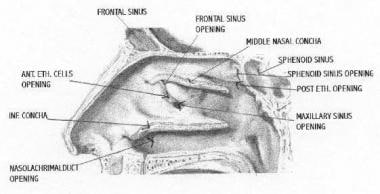 Sagittal section of the lateral nasal wall demonstrating openings of paranasal sinuses. Conchae have been cut to depict details of meatal structures.
Sagittal section of the lateral nasal wall demonstrating openings of paranasal sinuses. Conchae have been cut to depict details of meatal structures.
Structure and function of paranasal sinuses
The paranasal sinuses are air-filled bony cavities that extend from the skull base to the alveolar process and laterally from the nasal cavity to the inferomedial aspect of the orbit and the zygoma. The sinus cavities are lined with pseudostratified, ciliated, columnar epithelium that is contiguous, via ostia, with the lining of the nasal cavity. This epithelium contains a number of mucus-producing goblet cells. These goblet cells in the epithelium and the submucosal seromucous glands contribute to the airway surface liquid, [11] which is 5-100 μm thick and covers the epithelium.
Anterior and posterior ethmoid sinuses are composed of multiple air cells separated by thin bony partitions. Each cell is drained by an independent ostium that measures only 1-2 mm in diameter. These small openings are readily clogged by secretions or are occluded by swelling of the nasal mucosa. The sphenoid sinuses sit immediately anterior to the pituitary fossa and just behind the posterior ethmoid.
The arterial supply of the paranasal sinuses is from branches of the internal and external carotid arteries, whereas the venous and lymphatic drainage path is through the sinus ostia into the nasal cavity plexus. In addition, venous drainage occurs through valveless vessels corresponding to the arterial supply.
All sinus ostia drain into the nares at locations beneath the middle and superior turbinates. The posterior ethmoid and sphenoid sinuses drain into the superior meatus below the superior turbinate. The ostia of the maxillary, anterior ethmoid, and frontal sinuses share a common site of drainage within the middle meatus. This region is called the ostiomeatal complex and can be visualized by coronal CT scan. The common drainage pathway of the frontal, maxillary, and anterior ethmoid sinuses within the middle meatus allows relatively localized mucosal infection processes to promote infection in all these sinuses.
The successful maintenance of sinus drainage represents a complicated interaction between ciliary action, mucus viscosity, size of sinus ostia, and orientation of body structures. Ciliary beat at the rate of 8-15 Hz is continuously moved by the cilia at a speed of 6 mm/min. The ciliary action can be affected due to local factors, such as infection and local hypoxia that is associated with complete occlusion of sinus ostia. The sinus mucosa has less secretory and vasomotor function than the nasal cavity does. Cilia are concentrated near and beat toward the natural sinus ostia. Blockage of the ostium results in stasis of mucous flow, which can lead to development of disease.
The exact function of the paranasal sinuses is not well understood. The possible roles of the sinuses may include reducing the weight of the skull; dampening pressure; humidifying and warming inspired air; absorbing heat and insulating the brain; aiding in sound resonance; providing mechanical rigidity; and increasing the olfactory surface area.
Pathophysiology
The sinuses normally are sterile under physiologic conditions. Secretions produced in the sinuses flow by ciliary action through the ostia and drain into the nasal cavity. In the healthy individual, flow of sinus secretions always is unidirectional (ie, toward the ostia), which prevents back contamination of the sinuses. In most individuals, the maxillary sinus has a single ostium (2.5 mm in diameter, 5 mm2 in cross-sectional area) serving as the only outflow tract for drainage. This slender conduit sits high on the medial wall of the sinus cavity in a nondependent position. Most likely, the edema of the mucosa at these 1- to 3-mm openings becomes congested by some means (eg, allergy, viruses, chemical irritation) that causes obstruction of the outflow tract stasis of secretions with negative pressure, leading to infection by bacteria.
Retained mucus, when infected, leads to sinusitis. Another mechanism hypothesizes that because the sinuses are continuous with the nasal cavity, colonized bacteria in the nasopharynx may contaminate the otherwise sterile sinuses. These bacteria usually are removed by mucociliary clearance; thus, if mucociliary clearance is altered, bacteria may be inoculated and infection may occur, leading to sinusitis. [10, 12]
Data are available that support the fact that healthy sinuses are colonized. The bacterial flora of noninflamed sinuses were studied for aerobic and anaerobic bacteria in 12 adults who underwent corrective surgery for septal deviation. [13] Organisms were recovered from all aspirates, with an average of 4 isolates per sinus aspirate. The predominant anaerobic isolates were Prevotella, Porphyromonas, Fusobacterium and Peptostreptococcus species. The most common aerobic bacteria were S pyogenes, S aureus, S pneumonia, and H influenzae. In another study, specimens were processed for aerobic bacteria only, and Staphylococcus species and alpha-hemolytic streptococci were isolated. [14] Organisms were recovered in 20% of maxillary sinuses of patients who underwent surgical repositioning of the maxilla.
In contrast, another report of aspirates of 12 volunteers with no sinus disease showed no bacterial growth. [15] Jiang et al evaluated the bacteriology of maxillary sinuses with normal endoscopic findings. [16] Organisms were recovered from 14 (47%) of 30 swab specimens and 7 (41%) of 17 of mucosal specimens. Gordts et al reported the microbiology of the middle meatus in normal adults and children. [17] This study noted in 52 patients that 75% had bacterial isolates present, most commonly coagulase-negative staphylococci (CNS) (35%), Corynebacterium species (23%), and S aureus (8%) in adults. Low numbers of these species were present. In children, the most common organisms were H influenzae (40%), M catarrhalis (34%), and S pneumoniae (50%), a marked difference from findings in adults. Nonhemolytic streptococci and Moraxella species were absent in adults.
The pathophysiology of rhinosinusitis is related to 3 factors:
-
Obstruction of sinus drainage pathways (sinus ostia)
-
Ciliary impairment
-
Altered mucus quantity and quality
Obstruction of sinus drainage
Obstruction of the natural sinus ostia prevents normal mucus drainage. The ostia can be blocked by mucosal swelling or local causes (eg, trauma, rhinitis), as well as by certain inflammation-associated systemic disorders and immune disorders. Systemic diseases that result in decreased mucociliary clearance, including cystic fibrosis, respiratory allergies, and primary ciliary dyskinesia (Kartagener syndrome), can be predisposing factors for acute sinusitis in rare cases. Patients with immunodeficiencies (eg, agammaglobulinemia, combined variable immunodeficiency, and immunodeficiency with reduced immunoglobulin G [IgG]– and immunoglobulin A [IgA]–bearing cells) also are at increased risk of developing acute sinusitis.
Mechanical obstruction because of nasal polyps, foreign bodies, deviated septa, or tumors also can lead to ostial blockage. In particular, anatomic variations that narrow the ostiomeatal complex, including septal deviation, paradoxical middle turbinates, and Haller cells, make this area more sensitive to obstruction from mucosal inflammation. Usually, the margins of the edematous mucosa have a scalloped appearance, but in severe cases, mucus may completely fill a sinus, making it difficult to distinguish an allergic process from infectious sinusitis. Characteristically, all of the paranasal sinuses are affected and the adjacent nasal turbinates are swollen. Air-fluid levels and bone erosion are not features of uncomplicated allergic sinusitis; however, swollen mucosa in a poorly draining sinus is more susceptible to secondary bacterial infection.
Hypoxia within the obstructed sinus is thought to cause ciliary dysfunction and alterations in mucus production, further impairing the normal mechanism for mucus clearance.
Impaired ciliary function
Contrary to earlier models of sinus physiology, the drainage patterns of the paranasal sinuses depend not on gravity but on the mucociliary transport mechanism. The metachronous coordination of the ciliated columnar epithelial cells propels the sinus contents toward the natural sinus ostia. Any disruption of the ciliary function results in fluid accumulation within the sinus. Poor ciliary function can result from the loss of ciliated epithelial cells; high airflow; viral, bacterial, or environmental ciliotoxins; inflammatory mediators; contact between 2 mucosal surfaces; scars; and Kartagener syndrome. [18]
Ciliary action can be affected by genetic factors, such as Kartagener syndrome. Kartagener syndrome is associated with immobile cilia and hence the retention of secretions and predisposition to sinus infection. Ciliary function also is reduced in the presence of low pH, anoxia, cigarette smoke, chemical toxins, dehydration, and drugs (eg, anticholinergic medications and antihistamines).
Exposure to bacterial toxins can reduce ciliary function. Approximately 10% of cases of acute sinusitis result from direct inoculation of the sinus with a large amount of bacteria. Dental abscesses or procedures that result in communication between the oral cavity and sinus can produce sinusitis by this mechanism. Additionally, ciliary action can be affected after certain viral infections.
Several other factors can lead to impaired ciliary function. Cold air is said to stun the ciliary epithelium, leading to impaired ciliary movement and retention of secretions in the sinus cavities. On the contrary, inhaling dry air desiccates the sinus mucous coat, leading to reduced secretions. Any mass lesion with the nasal air passages and sinuses, such as polyps, foreign bodies, tumors, and mucosal swelling from rhinitis, may block the ostia and predispose to retained secretions and subsequent infection. Facial trauma or large inoculations from swimming can produce sinusitis as well. Drinking alcohol also can cause nasal and sinus mucosa to swell and cause impairment of mucous drainage.
Altered quality and quantity of mucus
Sinonasal secretions play an important role in the pathophysiology of rhinosinusitis. The mucous blanket that lines the paranasal sinuses contains mucoglycoproteins, immunoglobulins, and inflammatory cells. It consists of 2 layers: (1) an inner serous layer (ie, sol phase) in which cilia recover from their active beat and (2) an outer, more viscous layer (ie, gel phase), which is transported by the ciliary beat. Proper balance between the inner sol phase and outer gel phase is of critical importance for normal mucociliary clearance.
If the composition of mucus is changed, so that the mucus produced is more viscous (eg, as in cystic fibrosis), transport toward the ostia considerably slows, and the gel layer becomes demonstrably thicker. This results in a collection of thick mucus that is retained in the sinus for varying periods. In the presence of a lack of secretions or a loss of humidity at the surface that cannot be compensated for by mucous glands or goblet cells, the mucus becomes increasingly viscous, and the sol phase may become extremely thin, thus allowing the gel phase to have intense contact with the cilia and impede their action. Overproduction of mucus can overwhelm the mucociliary clearance system, resulting in retained secretions within the sinuses.
Acute sinusitis in the intensive care setting
Acute sinusitis in the intensive care population is a distinct entity, occurring in 18-32% of patients with prolonged periods of intubation, and usually is diagnosed during the evaluation of unexplained fever. Cases in which the cause is obstruction are usually evident and can include the presence of prolonged nasogastric or nasotracheal intubation. Moreover, patients in an intensive care setting generally are debilitated, predisposing them to septic complications, including sinusitis. Finally, sinusitis in intensive care settings is associated with nasal catheter placement.
Etiology
Purulent sinusitis can occur when ciliary clearance of sinus secretions decreases or when the sinus ostium becomes obstructed, which leads to retention of secretions, negative sinus pressure, and reduction of oxygen partial pressure. This environment is then suitable for growth of pathogenic organisms. Factors that predispose the sinuses to obstruction and decreased ciliary function are allergic, nonallergic, or viral insults, which produce inflammation of the nasal and sinus mucosa and result in ciliary dysmotility and sinus obstruction.
In individuals with recurrent or persistent sinusitis, suspect other predisposing conditions such as cystic fibrosis, ciliary dyskinesia, allergic inflammation, immunodeficiency, or an anatomic problem. [8] These predisposing factors also are cited by the 2005 practice parameter for diagnosis and management of sinusitis issued by the American Academy of Allergy, Asthma and Immunology (AAAAI), as are cocaine addiction and nasal polyps and other causes of ostiomeatal obstruction. [5]
Acute viral rhinosinusitis
The vast majority of rhinosinusitis episodes are caused by viral infection. Most viral upper respiratory tract infections are caused by rhinovirus, but coronavirus, influenza A and B, parainfluenza, respiratory syncytial virus, adenovirus, and enterovirus are also causative agents. Rhinovirus, influenza, and parainfluenza viruses are the primary pathogens in 3-15% of patients with acute sinusitis. In about 0.5-2% of cases, viral sinusitis can progress to acute bacterial sinusitis. [19, 20]
Viral upper respiratory tract infections are the most important risk factor for the development of acute bacterial sinusitis. [21] Approximately 90% of patients who have viral upper respiratory tract infections have sinus involvement, but only 5-10% of these patients have bacterial superinfection requiring antimicrobial treatment. [22]
Acute bacterial rhinosinusitis
Acute bacterial rhinosinusitis very frequently is associated with viral upper respiratory tract infection, although allergy, trauma, neoplasms, granulomatous and inflammatory diseases, midline destructive disease, environmental factors, dental infection, and anatomic variation, which may impair normal mucociliary clearance, may predispose to bacterial infection.
S aureus is a common pathogen in sphenoid sinusitis. The vaccination of children with the 7-valent pneumococcal vaccine introduced in 2000 in the United States brought about the decline in the recovery rate of S pneumoniae and an increase in H influenza. [23, 24] In addition, the rate of recovery of S pneumoniae penicillin-resistant strains was different after vaccination.
P aeruginosa and other gram-negative rods have been recovered in acute sinusitis of nosocomial origin (especially in patients who have nasal tubes or catheters), immunocompromised persons, patients with HIV infection, and those with cystic fibrosis.
Sixty-six percent of patients with acute sinusitis grow at least 1 pathogenic bacterial species on sinus aspirates, whereas 26-30% percent of patients have multiple predominant bacterial species. The bacteria most commonly involved in acute sinusitis are part of the normal nasal flora. These bacteria can become sinus pathogens when they are deposited into the sinuses by sneezing, coughing, or direct invasion under conditions that optimize their growth.
The most common pathogens isolated from maxillary sinus cultures in patients with acute bacterial rhinosinusitis include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis.Streptococcus pyogenes, Staphylococcus aureus, and anaerobes are less commonly associated with acute bacterial rhinosinusitis; they have been found in fewer than 10% of patients with acute bacterial sinusitis, despite the ample environment available for their growth. The exceptions are in sinusitis resulting from a dental source and in patients with chronic sinus disease, in whom anaerobic organisms are usually isolated.
S pneumoniae are gram-positive, catalase-negative, facultatively anaerobic cocci that account for 20-43% of acute bacterial rhinosinusitis cases in adults. The rise of antimicrobial resistance in S pneumoniae is a major concern.
A 1998 surveillance study of respiratory tract isolates estimated that 12.3% of S pneumoniae isolates obtained from the paranasal sinuses had intermediate resistance to penicillin; 37.4% were penicillin-resistant. The paranasal sinuses represented the anatomic location with the highest resistance rate. [25] Resistance to macrolide, clindamycin, trimethoprim-sulfamethoxazole, and doxycycline was more common in isolates with intermediate penicillin resistance and those that were penicillin-resistant.
H influenzae are gram-negative, facultatively anaerobic bacilli. H influenza type B was a leading cause of meningitis until the widespread use of the vaccine. Nontypeable strains of H influenzae are responsible for 22-35% of acute bacterial rhinosinusitis cases in adults. Beta-lactamase production is the mechanism of antimicrobial resistance for this organism. Of isolates from the paranasal sinus, 32.7% were found to be beta-lactamase–positive for H influenza; other reports suggest a rate of 44%.
M catarrhalis are gram-negative, oxidase-positive, aerobic diplococci. M catarrhalis is the responsible pathogen in 2-10% of acute bacterial rhinosinusitis cases in adults. Beta-lactamase production also is the mechanism of antimicrobial resistance for M catarrhalis. Of isolates from the paranasal sinus, 98% were found to be beta-lactamase–positive for M catarrhalis.
S aureus, though accounting for 10% of episodes of acute bacterial rhinosinusitis, now is recognized as an increasingly common pathogen in acute bacterial rhinosinusitis. [26] Whereas methicillin-resistant S aureus (MRSA) still represents a minority of episodes of S aureus rhinosinusitis, increasing trends of drug-resistant S aureus may alter future treatment recommendations. [27]
Gram-negative organisms, including Pseudomonas aeruginosa (15.9%), Escherichia coli (7.6%), Proteus mirabilis (7.2%), Klebsiella pneumoniae, and Enterobacter species, predominate in nosocomial sinusitis, accounting for 60% of cases. Polymicrobial invasion is seen in 25-100% of cultures. The other pathogenic organisms found in nosocomial patients are gram-positive organisms (31%) and fungi (8.5%).
Acute invasive fungal rhinosinusitis
Rarely, sinusitis is caused by fungi. Fungal sinusitis (eg, allergic fungal sinusitis) may appear similar to lower airway disorder and allergic bronchopulmonary aspergillosis. [28]
Fungal agents associated with this condition include Aspergillus and Alternaria species. Bipolaris and Curvularia species are the most common fungi recovered in allergic fungal sinusitis, accounting for 60% and 20%, respectively, in most studies. Curvularia species is occasionally reported as the most common causative organism in the deep southern United States.
Epidemiology
Sinusitis affects 1 out of every 7 adults in the United States, with more than 30 million individuals diagnosed each year. Sinusitis is more common from early fall to early spring. Rhinosinusitis affects an estimated 35 million people per year in the United States and accounts for close to 16 million office visits per year. [29]
According to the National Ambulatory Medical Care Survey (NAMCS), approximately 14% of adults report having an episode of rhinosinusitis each year, and it is the fifth most common diagnosis for which antibiotics are prescribed, accounting for 0.4% of ambulatory diagnoses. [30]
In 1996, Americans spent approximately $3.39 billion treating rhinosinusitis. [31] The economic burden of acute sinusitis in children is $1.77 billion per year. [31]
International prevalence
Acute sinusitis affects 3 in 1000 people in the United Kingdom. Chronic sinusitis affects 1 in 1000 people. Sinusitis is more common in winter than in summer. Rhinoviral infections are prevalent in autumn and spring. Coronaviral infection occurs mostly from December to March.
Acute sinusitis in children
An average child is likely to have 6-8 colds (ie, upper respiratory tract infections) per year, and approximately 0.5-2% of upper respiratory tract infections in adults and 6-13% of viral upper respiratory tract infections in children are complicated by the development of acute bacterial sinusitis. [32, 33]
Sex distribution for acute sinusitis
Women have more episodes of infective sinusitis than men because they tend to have more close contact with young children. The rate in women is 20.3%, compared with 11.5% in men.
Prognosis
Sinusitis does not cause any significant mortality by itself. However, complicated sinusitis may lead to morbidity and, in rare cases, mortality.
Approximately 40% of acute sinusitis cases resolve spontaneously without antibiotics. The spontaneous cure for viral sinusitis is 98%. Patients with acute sinusitis, when treated with appropriate antibiotics, usually show prompt improvement. The relapse rate after successful treatment is less than 5%.
In the absence of response within 48 hours or worsening of symptoms, reevaluate the patient. Untreated or inadequately treated rhinosinusitis may lead to complications such as meningitis, cavernous sinus thrombophlebitis, orbital cellulitis or abscess, and brain abscess.
In patients with allergic rhinitis, aggressive treatment of nasal symptoms and signs of mucosal edema, which can cause obstruction of the sinus outflow tracts, may decrease secondary sinusitis. If the adenoids are chronically infected, removing them eliminates a nidus of infection and can decrease sinus infection.
-
Sagittal section of the lateral nasal wall demonstrating openings of paranasal sinuses. Conchae have been cut to depict details of meatal structures.
-
Air-fluid level (arrow) in the maxillary sinus suggests sinusitis.
-
CT cuts for a limited CT study.






