Practice Essentials
Central vertigo is vertigo due to a disease originating from the central nervous system (CNS). In clinical practice, it often includes lesions of cranial nerve VIII as well. Individuals with vertigo experience hallucinations of motion of their surroundings.
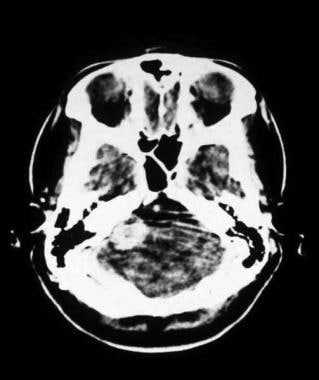
Central vertigo may be caused by hemorrhagic or ischemic insults to the cerebellum (see the image below), the vestibular nuclei, and their connections within the brain stem. Other causes include CNS tumors, infection, trauma, and multiple sclerosis. [1, 2]
 CT scan of a patient with an acute spontaneous cerebellar hemorrhage. The hemorrhage in the right lobe of the cerebellum is partly obscured by bony artifact.
CT scan of a patient with an acute spontaneous cerebellar hemorrhage. The hemorrhage in the right lobe of the cerebellum is partly obscured by bony artifact.
Signs and symptoms
Patients who have conditions known to cause central vertigo do not always complain strictly of vertigo.
Vertigo implies an abnormal sensation of movement or rotation of the patient or their environment. Some patients with central disease may complain of disequilibrium, imbalance, or difficulty maintaining an upright posture. Other important historical factors include the presence of associated symptoms and their nature; the onset, duration, and positional dependence of symptoms; and medical history.
Central vertigo often produces other neurologic symptoms, although this generalization has many exceptions. The symptoms are characterized as follows:
-
Gradual onset
-
Tend to be much less intense than those associated with peripheral vertigo
Diagnosis
The Dix-Hallpike test can help distinguish central vertigo from peripheral vertigo. During the test, the clinician rotates the patient's head 45 degrees to one side and then helps the patient to quickly lie back down. If rotational nystagmus is observed, the test is considered positive for benign positional vertigo. If the test is negative, CNS dysfunction may be indicated. [3]
Managment
Most patients with proven or suspected central vertigo should be admitted to the hospital for further evaluation and treatment under the care of a neurologist or neurosurgeon.
Background
Central vertigo is vertigo due to a disease originating from the central nervous system (CNS). In clinical practice, it often includes lesions of cranial nerve VIII as well. Individuals with vertigo experience hallucinations of motion of their surroundings.
Central vertigo may be caused by hemorrhagic or ischemic insults to the cerebellum (see the image below), the vestibular nuclei, and their connections within the brain stem. Other causes include CNS tumors, infection, trauma, and multiple sclerosis. [1, 2]
 CT scan of a patient with an acute spontaneous cerebellar hemorrhage. The hemorrhage in the right lobe of the cerebellum is partly obscured by bony artifact.
CT scan of a patient with an acute spontaneous cerebellar hemorrhage. The hemorrhage in the right lobe of the cerebellum is partly obscured by bony artifact.
Vertigo due to acoustic neuroma is also included in the broader category of central vertigo. An acoustic neuroma develops within the eighth cranial nerve, usually within the course of the internal auditory canal, yet it often expands into the posterior fossa with secondary effects on other cranial nerves and the brain stem.
Pathophysiology
The brainstem, cerebellum, and peripheral labyrinths are all supplied by the vertebrobasilar arterial system. Thus, the central and peripheral ischemic vertigo syndromes overlap.
Vertebrobasilar arterial system
The basilar artery is formed from the 2 vertebral arteries within the cranium at the level of the medulla. The artery has 3 branches on each side that supply the cerebellum. The posterior inferior cerebellar artery branches from the vertebral artery, while the anterior inferior cerebellar artery and the superior cerebellar artery branch from the basilar artery.
All 3 of the cerebellar arteries may have branches that supply brainstem tissue. A labyrinthine artery on each side branches from the basilar artery and supplies the labyrinth and associated structures via the internal auditory canal. In approximately two thirds of people, the basilar artery ends by bifurcating into the posterior cerebral arteries, with small posterior communicating arteries connecting to the internal carotid system in the circle of Willis.
Arterial occlusion and ischemic infarction
Arterial occlusion and ischemic infarction can result from cardioembolism, embolism of plaque from a vertebral artery, or local arterial thrombosis. One or both vertebral arteries, the basilar artery, or any of the smaller branches may be occluded. Even complete occlusion of a large artery may not result in death because of anastomotic retrograde flow via the circle of Willis and posterior communicating arteries.
Temporary vertebrobasilar ischemia may present as migraine syndrome or transient ischemic attacks (TIAs). While less common than cerebellar infarction, spontaneous cerebellar hemorrhage is an important life-threatening cause of vertigo associated with hypertensive vascular disease and anticoagulation. [4]
Multiple sclerosis
Multiple sclerosis is a demyelinating disease of the CNS. The course generally waxes and wanes, with varying neurologic symptoms and signs. Isolated vertigo may be the initial symptom in approximately 5% of cases (see Multiple Sclerosis).
Acoustic neuromas
Acoustic neuromas are Schwann cell tumors that usually originate on the vestibular division of the eighth cranial nerve in the proximal internal auditory canal. [5] Usually unilateral in development, bilateral acoustic neuromas do occur in young adults, although rarely, in association with neurofibromatosis type 2. If untreated, an acoustic neuroma may expand into the cerebellopontine angle and compress facial and other cranial nerves. [6] If it compresses the brainstem, ataxia, gait disturbances, spasticity, and weakness from long-tract effects may result. See the image below.
 CT scan of a patient with a large acoustic neuroma on the right side of the brainstem. The scan was performed after injection of intravenous contrast, which is critical for identifying tumors with CT imaging.
CT scan of a patient with a large acoustic neuroma on the right side of the brainstem. The scan was performed after injection of intravenous contrast, which is critical for identifying tumors with CT imaging.
Other causes
Isolated vertigo due to CNS infection, such as a microabscess, or temporal lobe seizures is rare and is not discussed in this article. Vertigo and dizziness are common complications of head and neck trauma. Traumatic central vertigo may be caused by petechial hemorrhages in the vestibular nuclei of the brainstem. These may result from shearing forces on the brainstem. [7]
Epidemiology
Frequency
Approximately 795,000 people in the United States have strokes each year. About 87% of these strokes are ischemic, and 1.5% of ischemic strokes affect primarily the cerebellum. [8] Ratio of ischemic to hemorrhagic cerebellar strokes is 3–5:1. [9] Up to 10% of patients with an isolated cerebellar infarction present with only isolated vertigo and imbalance. [10] Incidence of multiple sclerosis ranges from 10–80/100,000 per year, depending on the latitude. About 3000 cases of acoustic neuroma are diagnosed each year in the United States.
Mortality/morbidity
Vascular injuries and infarcts in the posterior circulation can cause severe permanent debilitating disease. The excellent recovery typical of acute vertigo caused by peripheral disease should not necessarily be expected in central vertigo.
-
A study of the rate and predictors of CNS disease in emergency department patients with dizziness, vertigo, or imbalance found that most cases were benign, although a substantial fraction of patients had serious neurologic disease. Of 907 patients experiencing dizziness (mean age, 59 years; 58% women [n=529]), 49 (5%) had a serious neurologic diagnosis, including 37 cerebrovascular events. Dizziness was often caused by benign conditions, such as peripheral vertigo (294 patients [32%]) or orthostatic hypotension (121 patients [13%]). [11]
-
In one series, cerebellar infarctions had mortality rates of 7% and 17% when associated with the superior cerebellar artery and posterior inferior cerebellar artery distributions, respectively. [12] Infarctions in the latter distribution are associated more commonly with a mass effect and compression of the brain stem and the fourth ventricle. In another series of patients with cerebellar infarction and mass effect, mortality rate was 17% despite aggressive neurosurgical and medical management. [13]
-
In one series of 94 patients with cerebellar hemorrhage, 20 presented with a Glasgow Coma Scale (GCS; see the Glasgow Coma Scale calculator) score less than 8, indicating significantly impaired consciousness. Mortality rate in the remaining patients who presented with GCS score higher than 8 was 20%. [4]
-
Acoustic neuroma has a low rate of mortality once diagnosed. The tumor often may be removed with preservation of facial nerve function, but unilateral hearing loss is common.
Demographics
Incidence of cerebrovascular disease is slightly higher in men than in women. In one series of patients with cerebellar infarction, the ratio of men to women was about 2:1. Multiple sclerosis is about twice as common in women as in men.
Incidence of stroke increases with age. The mean age of patients with cerebellar infarction in one series was 65 years, with half of the cases occurring in those aged 60–80 years. [9] In one series, the mean age of patients with cerebellar hematoma was 70 years. [4]
Prognosis
Prognosis for patients with central vertigo depends on the underlying disease and is highly variable.
Neurosurgical advancements have improved the prognosis for many serious conditions. This magnifies the importance of identifying these patients in the emergency setting.
The prognosis of infarction of the basilar or vertebral arteries is poor. In one series, 45% of patients presented in coma. Importantly, half of the patients in this series had prodromal symptoms, including vertigo, which cleared completely in the 6 months prior to the stroke. [14]
The prognosis for patients with spontaneous cerebellar hemorrhage is poor. Neurologic deterioration in these patients is associated independently with a hematoma in the central vermian area of the cerebellum and with secondary hydrocephalus. [4]
-
CT scan of a patient with an acute spontaneous cerebellar hemorrhage. The hemorrhage in the right lobe of the cerebellum is partly obscured by bony artifact.
-
MRI of a patient with an acute cerebellar hemorrhage less than 24 hours after presentation. MRI allows better resolution than CT scan without bony artifact. MRI is preferred over CT scan for imaging lesions in the posterior fossa.
-
CT scan of a patient with a large acoustic neuroma on the right side of the brainstem. The scan was performed after injection of intravenous contrast, which is critical for identifying tumors with CT imaging.
-
A CT slice through the brain of a patient with an acoustic neuroma. This slice reveals a level of the brain higher than the acoustic neuroma. The dilated third and lateral ventricles provide gross evidence of obstructive hydrocephalus due to pressure exerted by the tumor on the brainstem. A ventriculostomy, seen as a white circle in the right lateral ventricle, has been placed in an attempt to drain cerebrospinal fluid and relieve the excessive pressure above the brainstem.

