Overview
The thyroid gland, located anteriorly in the lower neck, is a pivotal endocrine organ producing thyroxine (T4), triiodothyronine (T3), and calcitonin. These hormones are essential for metabolic regulation, growth, and homeostasis. The gland's anatomical position, proximity, and relations to critical structures, including very rare anomalies such as the non-recurrent laryngeal nerve, significantly influence the postoperative outcomes and iatrogenic complications in various thyroid surgeries. [1]
Ectopic thyroid glands (ETGs) can manifest in various anatomical sites, necessitating accurate identification to prevent misdiagnosis or ineffective management. [2]
Insights into the thyroid gland ontogeny can help in elucidating tumor cell dedifferentiation mechanisms that are potentially driven by reactivated developmental pathways. [3] The endodermal origin of parafollicular cells (C cells) offers crucial insights and therapeutic targets to address aggressive C cell-derived neoplasms that are influenced by the migratory behavior of C cell precursors during their journey to the embryonic thyroid. [3]
Embryology and Development
Organogenesis: The thyroid originates at the pharyngeal floor between the first and second pharyngeal pouches, immediately dorsal to the aortic sac. [1] The thyroid primordium undergoes sequential morphological changes during its organogenesis (see Table 1). [3]
Table 1. Key Steps During Thyroid Gland Organogenesis and Development [3] (Open Table in a new window)
Steps |
Morphological Changes |
|---|---|
1 |
Formation of the thyroid placode begins near the base of the tongue. |
2 |
Transformation of the placode into the thyroid bud occurs near the apical pole of the aortic sac. |
3 |
Caudal migration of the thyroid primordium moves it to a pretracheal position. Initially, the primordium remains connected to the pharyngeal endoderm via the thyroglossal duct. As migration progresses, the thyroglossal duct degenerates, leaving the thyroid primordium encapsulated by mesenchyme, until it reaches the aortic sac. |
4 |
Bifurcation of the primordium - Thyroid tissue extends bilaterally along the pharyngeal arch arteries, accompanied by proliferation of thyroid progenitors. |
5 |
Formation of the left and right thyroid lobes occurs. Lateral lobes develop on either side of the larynx and proximal trachea, connected anteriorly by the thyroid isthmus. Thyroid bilobation also involves fusion with the ultimobranchial body (UBB), which integrates with each lateral thyroid lobe. |
6 |
Folliculogensis - Final morphogenetic stage, during which the thyroid attains its signature histological architecture, coinciding with functional cell differentiation and thyroglobulin synthesis. |
Folliculogensis: It involves three developmental stages, occurring within a specific time frame during gestation (see Table 2). [1]
Table 2. Folliculogensis and Endocrinal Development of the Thyroid Gland at Different Postmenstrual Weeks [1] (Open Table in a new window)
Postmenstrual Weeks |
Stage |
Histological and Endocrinal Changes |
10-18 Weeks |
Stage 1 |
Active folliculogenesis with gradual accumulation of colloid Release of thyroglobulin, serving as the substrate for tyrosine iodination and subsequent synthesis of thyroid hormones T4 and T3 |
18-29 Weeks |
Stage 2 |
Quiescent phase with minimal changes in the epithelium: colloid ratio and follicular size |
Week 29 Onward |
Stage 3 |
Gradual increase in the epithelium: colloid ratio Decrease in follicular size Enhanced stimulation by pituitary-derived thyrotropin (thyroid-stimulating hormone [TSH]) in the third trimester |
Stromal compartment: Vagal neural crest mesenchyme gives rise to the connective tissue capsule and interlobular septa. Perifollicular mesenchyme carries the neurovascular and lymphatic supply to the gland. [1]
Endocrine function:
- Production of fetal thyroid hormone begins later, following the TSH-dependent expression of genes involved in iodide uptake and iodination. [3] However, evidence suggests that stimulation of the fetal thyroid gland by pituitary-derived thyrotropin (TSH) is enhanced in the third trimester. Thus, T4 is present at low levels from postmenstrual weeks 10-22 and begins to increase during postmenstrual weeks 22-40. [1]
- Parafollicular cells or C cells - They are derived from the endoderm and originate from the UBBs. They possess neuroendocrine characteristics and predominantly synthesize calcitonin. [3]
Gross Anatomy
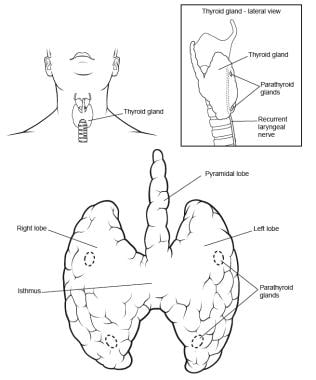
Location: The thyroid is a highly vascular, brownish-red gland located anteriorly in the lower neck, extending from the level of the fifth cervical down to the first thoracic vertebrae.
Appearance: The gland varies from an H to a U shape and is formed by two elongated lateral lobes with superior and inferior poles connected by a median isthmus. The lobes of the thyroid gland appear conical, each measuring usually 5 cm in length, with its greatest transverse and anteroposterior extents being 3 cm and 2 cm, respectively. Their ascending apices diverge laterally to align with the oblique lines on the laminae of the thyroid cartilage, while their bases are positioned at the level of the fourth or fifth tracheal cartilage (see the image below). [1] The isthmus measures 1.25 cm transversely and vertically and is usually anterior to the second and third tracheal cartilages, although it can be higher or even sometimes lower because its site and size vary greatly. [1] It is encountered during routine tracheotomy and must be retracted (superiorly or inferiorly) or divided. Occasionally, the isthmus is absent, and the gland exists as two distinct lobes. The video below depicts an ultrasonographic view of the right lobe of the thyroid gland. [4, 5]
The video below depicts an ultrasonographic view of the right lobe of the thyroid gland.
Although thyroid weight varies, it averages 25-30 g in adults (it is slightly heavier in women). The gland enlarges during menstruation and pregnancy.

A conical pyramidal lobe often ascends from the isthmus or the adjacent part of either lobe (more often the left) toward the hyoid bone, to which it may be attached by a fibrous or fibromuscular band, the levator of the thyroid gland (musculus levator glandulae thyroideae). [1] Usually, two pairs of parathyroid glands lie in proximity to the thyroid gland. (See also Embryology of the Thyroid and Parathyroids.)
Zuckerkandl's tubercle is a normal thyroid protuberance arising from the posterior or lateral lobes of the thyroid gland. [1] It is regarded as a consistent anatomical landmark for identifying the recurrent laryngeal nerve and the superior parathyroid gland. Usually, it extends into the tracheoesophageal groove or posterior to the esophagus. [6] Recognition of the Zuckerkandl's tubercle's anatomical and morphological features is vital to avoid its misidentification as a neoplasm or lymph node in computed tomography (CT) imaging and to prevent unnecessary biopsies. Incomplete excision during thyroidectomy may result in persistent or recurrent pathology. [6]
Innervation of the Thyroid
Principal innervation of the thyroid gland derives from the autonomic nervous system. Parasympathetic fibers come from the vagus nerves, and sympathetic fibers are derived from the superior, middle, and inferior cervical sympathetic ganglia. Postganglionic fibers from the inferior cervical ganglion form a plexus on the inferior thyroid artery, which accompanies the artery to the thyroid gland. This plexus communicates with the recurrent laryngeal nerve, the external branch of the superior laryngeal nerve, the superior cardiac nerve, and the plexus on the common carotid artery. [1]
Autonomic nervous regulation of the glandular secretion is not clearly understood, but most of the effect is postulated to be on blood vessels, hence the perfusion rates of the glands.
Microscopic Structure
Under the middle layer of deep cervical fascia, the thyroid has an inner true capsule, which is thin and adheres closely to the gland. Extensions of this capsule within the substance of the gland form numerous septae, which divide it into lobes and irregularly shaped and sized lobules. The lobules are composed of spherical, cyst-like follicles, the functional and structural units of the gland. Each follicle has the following features: [1]
-
A layer of simple epithelium resting on a basal lamina and enclosing a colloid-filled cavity (see the image below)
-
Colloid is mainly made up of iodinated glycoprotein called iodothyroglobulin, which is the inactive stored form of the active thyroid hormones, triiodothyronine (T3) and thyroxine (T4), produced by the follicular epithelial cells. [1] It stains pink on hematoxylin and eosin stain.
-
The follicles are surrounded by connective tissue stroma containing dense plexuses of fenestrated capillaries, extensive lymphatic networks, and sympathetic nerve fibers that supply the arterioles and capillaries. [1]
Epithelial cells are of two types: principal cells (i.e., follicular) and parafollicular cells (i.e., C, clear, light cells). Follicular cells are responsible for the formation of the colloid (iodothyroglobulin), whereas parafollicular cells produce the hormone calcitonin.
Follicular cells: Follicular cells show morphological variations, ranging from squamous or low cuboidal to columnar, based on their activity level, which is primarily regulated by circulating TSH (thyrotropin). Based on their activity and morphological appearance, they are classified into the resting and active follicles (see Table 3}. [1] Follicles showing differing levels of activity may coexist.
Table 3. Morphological and Functional Differences Between Resting and Active Follicular Cells [1] (Open Table in a new window)
Feature |
Resting Follicular Cells |
Active Follicular Cells |
|---|---|---|
Size of Follicles |
Large |
Smaller |
Epithelium |
Lined by squamous or low cuboidal epithelium |
Lined by columnar epithelium |
Luminal Colloid |
Abundant |
Reduced |
Apical Microvilli |
Short |
Elongated and often branched on TSH stimulation |
Functional Polarization |
Less pronounced |
Highly polarized |
Endocytosis of Colloid at the Luminal Epithelium |
Minimal |
High, induced by TSH secretion |
Cytoplasmic Processes |
Absent or minimal |
Extended into the luminal colloid to sequester droplets |
Intracellular Colloid Droplets |
Rare |
Abundant, containing iodinated thyroglobulin |
Thyroid Hormone (T3 and T4) Release |
Limited |
Active release at the cell base, exported via capillaries and lymphatics |
Effects of Prolonged TSH Levels |
No significant hypertrophy |
Follicular cell hypertrophy, progressive colloid resorption, and increased stromal vascularity |
C cells: The thyroid parenchyma contains C (clear) cells, named for their pale-staining cytoplasm. They are predominantly located in the middle third of each lateral thyroid lobe and are typically found scattered within thyroid follicles, lying inside the basal lamina but not extending to the follicle lumen. Occasionally, they form clusters in the interfollicular stroma and are hence also known as parafollicular cells. They are part of the amine precursor uptake and decarboxylation neuroendocrine system. These cells produce calcitonin, which lowers blood calcium by inhibiting bone resorption and calcium reabsorption from renal tubules. [1]
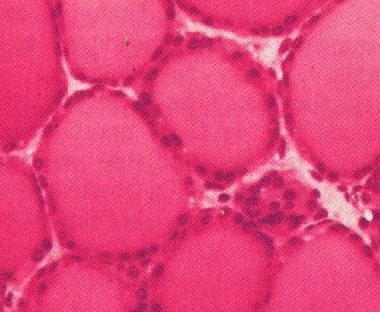 Follicles of the thyroid gland, consisting of a layer of simple epithelium enclosing a colloid-filled cavity.
Follicles of the thyroid gland, consisting of a layer of simple epithelium enclosing a colloid-filled cavity.
Thyroid neoplasms:
- Thyroid cancers are usually differentiated and arise from the follicular cells. A majority of differentiated thyroid cancers arise de novo. After excision, any residual tissue or tumor can be treated with radioactive iodine, as the cells retain the capacity to trap and incorporate iodine into the tyrosine residues of thyroglobulin. Routine follow-up is done by serum thyroglobulin measurements. [1]
- Medullary thyroid cancer arises from C cells. It is a rare malignancy that may be familial and associated with multiple endocrine neoplasia syndromes, such as MEN2A, when occurring alongside a pheochromocytoma and primary hyperparathyroidism. Post excision, patients are monitored clinically and via serial serum measurements of plasma calcitonin levels. [1]
Fascia and Ligament
Fascia: The thyroid gland is ensheathed by the visceral fascia, a division of the middle layer of deep cervical fascia, which attaches it firmly to the laryngoskeleton. This visceral layer divides into two layers at the posterior border of the gland. The anterior layer covers the entire medial surface of each lobe. At, or just above, the isthmus, this layer is conspicuously thickened to form the lateral ligament of the thyroid gland , which attaches the gland to the trachea and the lower part of the cricoid cartilage. The posterior layer passes behind the esophagus and pharynx to become attached to the prevertebral fascia. A compartment is thus formed on each side of the midline, lateral to the trachea and esophagus; it contains fat, the recurrent laryngeal nerve, and terminal parts of the inferior thyroid artery. The nerve may be lateral or medial to the lateral ligament of the thyroid gland and sometimes may be embedded in it. [6]
Ligaments of the thyroid gland: The anterior suspensory ligament extends from the superior-medial aspect of each thyroid lobe to the cricoid and thyroid cartilage. The posteromedial aspect of the gland is attached to the side of the cricoid cartilage, first and second tracheal ring, by the posterior suspensory ligament (i.e., Berry's ligament). This firm attachment of the gland to the laryngoskeleton is responsible for the movement of the thyroid gland and related structures during swallowing.
On its way to the larynx, the recurrent laryngeal nerve usually passes deep to the Berry's ligament or between the main ligament and its lateral leaf. Deep to the ligament, but lateral to the nerve, is a posteromedial portion of the thyroid lobe, which may be overlooked during thyroidectomy
Strap Muscles
The lateral surface of the thyroid is covered by the sternothyroid muscle, and its attachment to the oblique line of the thyroid cartilage prevents the superior pole from extending superiorly under the thyrohyoid muscle. More anteriorly are the sternohyoid and superior belly of the omohyoid muscle, overlapped inferiorly by the anterior border of the sternocleidomastoid muscle. The sternohyoid and sternothyroid muscles are joined in the midline by an avascular fascia that must be incised to retract the strap muscle laterally in order to access the thyroid gland during thyroidectomy. If strap muscles are to be transected for better exposure, do so high in the neck, because the motor nerve supply from the ansa cervicalis enters these muscles inferiorly.
Relations and Surfaces of the Thyroid Gland
Lateral (superficial) surface: It is covered by the sternothyroid muscle whose attachment to the oblique thyroid line restricts the upper pole of the gland from extending onto the thyrohyoid. [1]
Posterolateral surface: This is adjacent to the carotid sheath and overlaps the common carotid artery.
Medial surface: It is adapted to the larynx and trachea. The superior pole contacts the inferior pharyngeal constrictor and the posterior part of the cricothyroid muscle, which separates it from the posterior part of the thyroid lamina and the side of the cricoid cartilage. The external branch of the superior laryngeal nerve is medial to this portion of the gland and supplies the cricothyroid muscle. Inferiorly, it is related to the trachea, the recurrent laryngeal nerve, and the esophagus (closer to the left). [1]
Anterior relations: [1]
- Sternohyoid and the superior belly of the omohyoid muscle lie anteriorly, overlapped inferiorly by the anterior border of the sternocleidomastoid muscle.
- The anterior border of the gland is thin and slants down medially near the anterior branch of the superior thyroid artery.
Posterior relations: [1]
- The posterior border is rounded and related inferiorly to the inferior thyroid artery and its anastomosis with the posterior branch of the superior thyroid artery.
- On the left side, the lower end of the posterior border lies near the thoracic duct. Parathyroid glands are usually related to the posterior border.
Isthmus: It is covered by the sternothyroid muscle, separated by pretracheal fascia. It is more superficially covered by the sternohyoid muscle, anterior jugular veins, fascia, and skin. Superior thyroid arteries anastomose along its upper border and inferior thyroid veins leave the gland at its lower border. [1]
Vascular Anatomy and Laryngeal Innervation
The arterial supply to the thyroid gland comes from the superior and inferior thyroid arteries and, occasionally, from the thyroid ima artery. These arteries have abundant collateral anastomoses with each other, ipsilaterally and contralaterally. The thyroid ima is a single vessel that, when present, originates from the aortic arch or the brachiocephalic (innominate) artery and enters the thyroid gland at the inferior border of the isthmus (see the image below).
Superior thyroid artery and superior laryngeal nerve
The superior thyroid artery is the first branch of the external carotid artery. It arises from the anterior surface of the external carotid just below the level of the greater cornu of the hyoid bone. [1] In rare cases, it may arise from the common carotid artery just before its bifurcation. It vascularizes the thyroid gland and some adjacent skin. [4]
Course: The superior thyroid artery descends medially to the larynx under the cover of the omohyoid and sternohyoid muscles. The artery runs superficially on the anterior border of the lateral lobe, sending a branch deep into the gland before curving toward the isthmus, where it anastomoses with the contralateral artery. It gives off anterior, posterior, and lateral branches to the thyroid (see Table 4).
Table 4. Branches of the Superior Thyroid Artery to the Thyroid: Course, Area Supplied, and Anastomosis [1] (Open Table in a new window)
Branch |
Course |
Supplied Area |
Anastomosis |
|---|---|---|---|
Anterior |
Runs along the medial side of the upper pole of the lateral lobe |
Mainly the anterior surface |
With contralateral fellow above the isthmus |
Posterior |
Descends on the posterior border |
Medial and lateral surfaces |
With inferior thyroid artery |
Lateral |
Occasionally supplies the lateral surface |
Lateral surface |
Relations: Cephalad to the superior pole, the external branch of the superior laryngeal nerve runs with the superior thyroid artery before turning medially to supply the cricothyroid muscle. High ligation of the superior thyroid artery during thyroidectomy places this nerve at risk of inadvertent iatrogenic injury, which can impair vocal cord function, causing dysphonia by altering pitch regulation. The cricothyroid artery, a potentially bothersome branch of the superior thyroid artery, runs cephalad to the upper pole and toward the midline on the cricothyroid ligament. This vessel can be lacerated during emergent cricothyroidotomy. [7]
Inferior thyroid artery and recurrent laryngeal nerve
The inferior thyroid artery arises from the thyrocervical trunk, a branch of the first part of the subclavian artery.
Course: It ascends vertically and then curves medially to enter the tracheoesophageal groove in a plane posterior to the carotid sheath. Near its origin on the left side, the artery is crossed anteriorly by the thoracic duct, as the latter curves inferolaterally to its termination. [1] As it nears the thyroid gland, the artery usually passes behind the recurrent laryngeal nerve. The artery is not accompanied by the inferior thyroid vein. [1] Together with the inferior thyroid and common carotid arteries, the recurrent laryngeal nerve forms one of the sides of Beahr's triangle. Most of its branches penetrate the posterior aspect of the lateral lobe, as shown below.
The inferior thyroid artery has a variable branching pattern and is closely associated with the recurrent laryngeal nerve (seen in the image below). The latter also ascends in the tracheoesophageal groove and enters the larynx between the inferior cornu of the thyroid cartilage and the arch of the cricoid. The recurrent laryngeal nerve can be found after it emerges from the superior thoracic outlet, in a triangle bounded laterally by the common carotid artery, medially by the trachea, and superiorly by the thyroid lobe.
Relations between the terminal branches of the artery and the recurrent laryngeal nerve are highly variable. The right nerve can be anterior, posterior, or amongst the branches of the artery while the left nerve is usually posterior, though occasionally it lies anterior to it. On the left side, since the recurrent laryngeal nerve loops around the artery of the sixth branchial arch (aortic arch), it is 45° to the midline in its ascent from the chest to the neck. Conversely, on the right side, it is more superficial and lateral as it loops around the fourth branchial arch artery (subclavian) in the neck. These anatomical differences in course are critical in thyroid surgery and are reversed in cases of dextrocardia. [1]
The relationship between the nerve and the inferior thyroid artery is highly variable, as demonstrated by the classic work of Reed, who in 1943 described 28 variations in this relationship. The nerve can be found deep to the inferior thyroid artery (40%), superficially (20%), or between branches of the artery (35%). [8] Significantly, the relationship between nerve and artery on one side of the neck is similar to that found on the other side in only 17% of the population. Furthermore, at the level of the inferior thyroid artery, branches of the recurrent laryngeal nerve that are extralaryngeal may be present (5%). Preservation of all of those branches is important during thyroidectomy. Another hint to the location of the recurrent laryngeal nerve is the Zuckerkandl's tubercle, an extension of the thyroid, which is close to the Berry's ligament. [9] On rare occasions, the recurrent laryngeal nerve may pass directly from the vagus to the larynx, close to the superior thyroid vessels. This formation is nearly always observed on the right side and is associated with a retroesophageal subclavian artery. However, the formation can occur on the left side in cases of transposition of the great vessels.
Venous Drainage and Lymphatics
Veins: Three pairs of veins provide venous drainage for the thyroid gland (see the image below).
- The superior thyroid vein emerges from the upper part of the gland, ascends along the superior thyroid artery, and drains into the internal jugular vein. [1]
- The middle thyroid vein collects blood from the lower part of the gland; it emerges from the lateral surface of the gland, follows a direct course laterally, and drains into the internal jugular vein. [1]
- The inferior thyroid veins originate in a glandular venous plexus that connects with the middle and superior thyroid veins. These veins form a pretracheal plexus and follow different paths on each side. The right inferior thyroid vein descends obliquely across the brachiocephalic artery to join the right brachiocephalic vein at its junction with the superior vena cava. The left inferior vein descends to join the left brachiocephalic vein. The inferior thyroid veins often open via a common trunk into the superior vena cava or left brachiocephalic vein. They drain the esophageal, tracheal, and inferior laryngeal veins and have valves at their terminations. [1] Occasionally, both inferior veins form a common trunk called the thyroid ima vein, which empties into the left brachiocephalic vein.
Lymphatic drainage of the thyroid gland is extensive and flows multidirectionally. Immediate lymphatic drainage courses to the periglandular nodes; to the prelaryngeal (Delphian), pretracheal, and paratracheal nodes along the recurrent laryngeal nerve; and then to mediastinal lymph nodes. Thyroid lymphatic vessels connect within the gland and tracheal plexus. They proceed to prelaryngeal nodes above the thyroid isthmus and pretracheal and paratracheal nodes (level VI). [1]
- Major lymphatic drainage occurs in middle and lower jugular lymph nodes in levels III and IV and posterior triangle nodes in level Vb.
- Minor drainage occurs in pretracheal and paratracheal nodes in level VI and superior mediastinal nodes in level VII.
- Laterally, drainage occurs to deep cervical nodes (level IV) via vessels along superior thyroid veins.
- Some vessels drain into brachiocephalic nodes near the thymus in the superior mediastinum (level VII).
- Thyroid lymphatics can also drain directly to the thoracic duct without an intervening node. [1]
Regional metastases of thyroid carcinoma can also be found laterally, higher in the neck along the internal jugular vein. This can be explained by tumor invasion of the pretracheal and paratracheal nodes, causing an obstruction of normal lymph flow.
Imaging
Ultrasound: The gland's superficial location facilitates sonographic examination and fine needle aspiration cytology. [1]
CT scans: They are instrumental in identifying the position and morphological characteristics of the Zuckerkandl's tubercle, distinguishing it from other nodules or nodule-like regions. CT is also crucial for detecting ETGs that migrate to intracranial, thoracic, abdominopelvic, or concealed locations. [2]
Magnetic resonance imaging (MRI): High vascularity of the thyroid gland leads to an intense contrast enhancement and increased signal on T2-weighted images. [1]
Radionuclide imaging or thyroid static imaging: [2] It is done with technetium-99m (99mTc) pertechnetate, iodine-123 or iodine-131. The radionuclide 99mTc is trapped by the thyroid similar to iodine without getting organified. It provides morphological information and the location of ETGs. Functional information about the thyroid gland (particularly about ectopic thyroid tissue) can be obtained with the use of iodine-123 or iodine-131, which is trapped and organified. [1]
However, current imaging techniques, including ultrasound, CT, and MRI, do not resolve the follicular nature of the thyroid gland, presenting it as a homogeneous texture.
Natural Variants
Ectopic Thyroid Gland
ETG is a rare congenital embryonic developmental disorder. Most ETGs involve a single ectopic thyroid tissue, with double or triple occurrences being rare. [2]
Location: Ectopic thyroid tissue is typically found along the thyroglossal duct pathway, laterally in the neck, or in remote regions such as the tongue (lingual thyroid), mediastinum, and subdiaphragmatic organs. The most common site for ectopic thyroid tissue is the base of the tongue, especially at the foramen cecum, where it may represent the sole thyroid tissue. [3] Rarely, ETGs are detected in the liver, ovaries, and adrenal glands. [2]
Classification: Based on their ontogeny, ETGs are classified into two types: [2]
- Aberrant thyroid gland: Lacks thyroid tissue in the normal cervical position; seen in about 25% of cases
- Accessory thyroid gland: Coexists with the normal thyroid in the neck; is more common
Etiology: Mutations in genes such as TITF1, Tg, PAX8, and FOXE1, involved in thyroid maturation and differentiation, contribute to abnormal thyroid morphogenesis and migration. [2]
The clinical presentation of ETGs is typically nonspecific and insidious, with most patients remaining asymptomatic. Symptoms depend on size, location, pathology type, and thyroid function. Lingual ETG can cause dysphagia, hoarseness, and coughing. Tracheal ETG may present with dyspnea and hemoptysis. Thoracic ETG can lead to dysphagia and superior vena cava syndrome, while abdominopelvic ETG may cause bleeding, abdominal pain, and obstructive jaundice. [2]
Functional characteristics: ETGs often present with hypothyroidism due to reduced iodine uptake, though hyperthyroidism can occur. They have a low incidence of malignancy and lack distinct pathological features. Most ETGs are benign and symptom-free, but monitoring or management is essential due to potential symptoms and malignancy risks. [2]
Thyroglossal Cysts
Remnants of the thyroglossal duct may persist as accessory nodules or cysts of thyroid tissue between the isthmus and the foramen cecum of the tongue base.
-
Thyroid gland, anterior and lateral views.
-
Follicles of the thyroid gland, consisting of a layer of simple epithelium enclosing a colloid-filled cavity.
-
Distribution of thyroid arteries with associated laryngeal nerve, anterior view.
-
Distribution of thyroid arteries with associated laryngeal nerve, posterior view.
-
Distribution of thyroid veins.
-
Sonogram of a normal right lobe of the thyroid gland. Video courtesy of David L Francis, MD.
-
Distribution of thyroid arteries with associated laryngeal nerve, posterior view.
-
Thyroid gland and arterial supply and relationship to recurrent laryngeal nerves, anterior view.
-
Thyroid veins, anterior view.