Background
Severe iodine deficiency results in impaired thyroid hormone synthesis and/or thyroid enlargement (goiter). Population effects of severe iodine deficiency, termed iodine deficiency disorders (IDDs), include endemic goiter, hypothyroidism, cretinism, decreased fertility rate, increased infant mortality, and intellectual disability. [1]
Iodine is a chemical element. It is found in trace amounts in the human body, in which its only known function is in the synthesis of thyroid hormones. Iodine is obtained primarily through the diet but is also a component of some medications, such as radiology contrast agents, iodophor cleansers, and amiodarone.
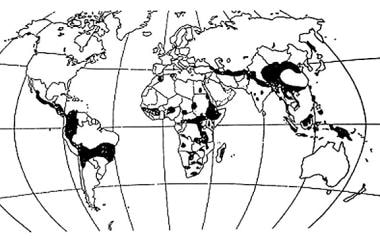
Worldwide, the soil in large geographic areas is deficient in iodine. Twenty-nine percent of the world’s population, living in approximately 130 countries, is estimated to live in areas of deficiency (see image below). [2] This occurs primarily in mountainous regions such as the Himalayas, the European Alps, and the Andes, where iodine has been washed away by glaciation and flooding. Iodine deficiency also occurs in lowland regions far from the oceans, such as central Africa and Eastern Europe. Persons who consume only locally produced foods in these areas are at risk for IDD, [2, 3, 4] with infants, pregnant women, and those in low-resource regions particularly impacted. See the distribution of iodine deficiency in the image below.
In 2001, the World Health Organization (WHO), United Nations Children's Fund (UNICEF) and International Council for Control of Iodine Deficiency Disorders (ICCIDD) developed a system for classifying iodine deficiency based upon the median urinary iodine concentration in a population (See Table 1. below). [3]
Table 1. Iodine Deficiency Classification (Open Table in a new window)
Iodine Deficiency |
None |
Mild |
Moderate |
Severe |
Median urine iodine, mcg/L |
>100 |
50-99 |
20-49 |
< 20 |
Goiter prevalence |
< 5% |
5-20% |
20-30% |
>30% |
Neonatal thyroid-stimulating hormone (TSH), >5 IU/mL whole blood |
< 3% |
3-20% |
20-40% |
>40% |
Cretinism |
0 |
0 |
+ |
+ |
Adapted from the World Health Organization (WHO)/United Nations Children's Fund (UNICEF)/International Council for Control of Iodine Deficiency Disorders (ICCIDD). |
||||
Normal dietary iodine intake is between 90-150 mcg/day (higher in pregnant and lactating women). The US Institute of Medicine’s (IOM’s) recommended dietary allowance (RDA) of iodine is as follows:
-
Adults and adolescents: 150 mcg/day
-
Pregnant women: 220 mcg/day
-
Lactating women: 290 mcg/day
-
Children aged 1-11 years: 90-120 mcg/day
-
Infants: Adequate intake is 110-130 mcg/day
WHO’s recommendations are similar for adults and adolescents but vary for infants, children, and pregnant and lactating women as follows [3] :
-
Pregnant and lactating women: 250 mcg/day
-
Children aged 6-12 years: 120 mcg/day
-
Infants to 6 years: 90 mcg/day
Sources of dietary iodine
In areas where iodine is not added to the water supply or food products meant for humans or domesticated animals, the primary sources of dietary iodine are saltwater fish, seaweed, and trace amounts in grains. The upper limit of safe daily iodine intake is 1100 mcg/day for adults; it is lower for children. [5, 6, 7, 8]
In the United States, iodine has been voluntarily supplemented in table salt 45 mcg iodine/g salt. [9] Salt was selected as the medium for iodine supplementation because intake is uniform across all socioeconomic strata and across seasons of the year, supplementation is achieved using simple technology, and the program is inexpensive. The estimated annual cost of iodine supplementation of salt in the United States is $0.04 per person.
Other major sources of dietary iodine in the United States are egg yolks, milk, and milk products because of iodine supplementation in chicken feed, the treatment of milk cows and cattle with supplemental dietary iodine to prevent hoof rot and increase fertility, and the use of iodophor cleaners by the dairy industry. Bread is also a significant source of dietary iodine in the United States. [10]
Changes in US iodine intake
In the early 1900s, the Great Lakes, Appalachian, and northwestern regions of the United States were endemic regions for IDD, but since the iodization of salt and other foods in the 1920s, dietary iodine levels generally have been adequate. However, sustaining these iodization programs has become a concern.
Data collected in the United States by National Health and Nutrition Examination Survey I (NHANES I) for the years 1971-1974 showed that the median urinary iodine level was 320 mcg/L, reflecting adequate dietary iodine intake. [11] However, by the time of NHANES III (1988-1994), the median urinary iodine value had fallen to 145 mcg/L.
The reduction in US dietary iodine intake since the 1970s has likely been the result of the removal of iodate conditioners in store-bought breads, widely publicized recommendations for reduced salt and egg intake for blood pressure and cholesterol control, the increasing use of noniodized salt in manufactured or premade convenience foods, decreased iodine supplementation of cattle feed, poor education about the medical necessity of using iodized salt, and reduction in the number of meals made at home. [11, 12, 13]
The NHANES surveys of 2001-2002, 2005-2006, 2007-2008, and 2009-2010 showed that US dietary iodine intake has stabilized. [12, 13] Although the most recent NHANES survey reveals adequate iodine intake in the general US population, certain groups have an insufficient intake of iodine, such as pregnant women, who were found to have a median urinary iodine concentration of 125 mcg/L. [14]
Population-based assessment and treatment
In population-based assessments, iodine sufficiency can be determined based on the results of a spot urine test for iodine and creatinine. [12] Supplementation can be achieved by using iodized salt in cooking or a once-daily multiple vitamin containing sodium iodide. [5, 15]
Pediatric considerations
Infants do not have much stored intrathyroidal iodine, with much of their iodine intake coming from human milk. [16] (A systematic review suggested that in the first 6 months of lactation, breast milk iodine concentrations of about 150 mcg/L may achieve or exceed infant iodine equilibrium, potentially preventing effects of iodine deficiency on neurologic growth and development. [16] ) However, iodine stores within the thyroid increase with age in pediatric patients. Therefore, infants and young children tend to have higher 131I uptake than adults. Additionally, newborns and young infants are much more severely affected by iodine deficiency than adults and are more likely to become overtly hypothyroid.
Prenatal considerations
Women with severe iodine deficiency are more likely to experience infertility, and pregnancy in this group is more likely to result in miscarriage or congenital anomalies. Thyroid hormones are essential for fetal brain growth and development, and severe maternal iodine deficiency may lead to intellectual disability and growth retardation or cretinism in offspring, and even mild maternal iodine deficiency has been associated with lower IQ in children. [17] Even in areas of borderline iodine intake, as many as 10% of women may develop goiter during pregnancy.
Pathophysiology
Dietary iodine is taken up readily through the gut in the form of iodide. From the circulation, it is concentrated in the thyroid gland by means of an energy-dependent sodium-iodide symporter. In the follicle cells of the thyroid gland, 4 atoms of iodine are incorporated into each molecule of thyroxine (T4) and 3 atoms into each molecule of triiodothyronine (T3). These hormones are essential for neuronal development, sexual development, and growth and for regulating the metabolic rate, body heat, and energy.
When dietary iodine intake is inadequate for thyroid hormone synthesis, the serum T4 level initially falls and a number of processes ensue to restore adequate thyroid hormone production. The pituitary gland senses low levels of circulating T4 and releases more thyroid-stimulating hormone (TSH). TSH stimulates the growth and metabolic activity of thyroid follicular cells. TSH stimulates each cell to increase iodine uptake and thyroid hormone synthesis and secretion. Increased TSH levels and reduction of iodine stores within the thyroid result in increased T3 production relative to T4 production. T3 is 20-100 times more biologically active than T4 and requires fewer atoms of iodine for biosynthesis. The increased production of T3 results in the maintenance of normal levels of thyroid hormone bioactivity despite the reduction in T4 because of iodine deficiency.
These processes tend to conserve iodine stores and help maintain normal thyroid function. In addition, thyroid hormones are deiodinated in the liver, and the iodine is released back into the circulation for reuptake and reuse by the thyroid gland. Even under these circumstances, iodine is passively lost in the urine, with additional small (10%) losses from biliary secretion into the gut.
Goiter development and hyperthyroidism
Enlargement of the thyroid gland begins as an adaptive process to low iodine intake. Iodine deficiency is the most common cause of goiter in the world. The goiter initially is diffuse, but it eventually becomes nodular. Some nodules may become autonomous and secrete thyroid hormone regardless of the TSH level. These autonomous nodules have been demonstrated to frequently contain TSH-activating mutations. Initially, thyroid hormone output by the normal thyroid surrounding the autonomous nodules is reduced to maintain euthyroidism. Autonomous nodules may cause hyperthyroidism.
High levels of iodine, such as those found in radiographic contrast dyes or amiodarone, may cause hyperthyroidism in the setting of nodular goiter with “hot” or autonomous nodules or hypothyroidism in the setting of autoimmune thyroid disease. If the total output of thyroid hormone by the autonomous nodules exceeds that of the normal thyroid gland, the patient becomes biochemically hyperthyroid. This condition is known as a toxic multinodular goiter. [18]
Hypothyroidism
When iodine deficiency is more severe, thyroid hormone production falls and the patient may experience a hypothyroid condition. In such cases, adults have the usual signs and symptoms of hypothyroidism. However, congenital hypothyroidism (also known as cretinism) in fetuses and young children prevents central nervous system development and maturation, resulting in permanent intellectual disability, neurologic defects, and growth abnormalities. [5, 19]
Epidemiology
Occurrence in the United States
Early in the 20th century, the Great Lakes, Appalachian, and northwestern regions of the United States were endemic for iodine deficiency disorders, but since the iodization of salt and other foods in the 1920s, dietary iodine levels generally have been adequate. National survey data suggest that average US dietary iodine intake fell dramatically from 1971-1990 and then stabilized. Urinary iodine values of less than 50 mcg/L, moderate iodine deficiency, are found in 11.1% of the total population, 7.3% of pregnant women, and 16.8% of reproductive-aged women. [11, 12]
International occurrence
Approximately 70% of all households worldwide have access to adequately iodized salt. [2] In 2016, the Iodine Global Network reported that 110 countries had sufficient iodine intake,18 were mildly deficient, and 2 were moderately deficient. No countries were found to be severely iodine-deficient, and 10 countries had excessive iodine intake. [4]
Studies in Tibet and Uzbekistan have shown low coverage with adequately iodized salt. [20, 21] The Tibetan report also noted that urinary iodine concentration was an independent risk factor for thyroid peroxidase antibody positivity. [20]
Race-, sex-, and age-related demographics
No race predilection exists for iodine deficiency disorder; prevalence is affected only by geographic area and diet. However, non-Hispanic black pregnant women from both the NHANES 2005–2010 and the National Children's Study (NCS) consistently had lower urinary iodine than non-Hispanic whites or Hispanics. [14]
Patients of any age can be affected by iodine deficiency. The most devastating complications of iodine deficiency disorder occur when iodine is deficient during fetal and neonatal growth. After age 10 years, the prevalence of goiter is higher in girls than boys in areas of iodine deficiency. No sex-based difference is observed in the incidence of cretinism.
Prognosis
The supplementation of iodine does not reverse cretinism or reduce the size of large nodular goiters. Small, diffuse goiters of short duration that occur in infants or during pregnancy appear to be managed effectively with iodine supplementation.
Iodine deficiency can recur if iodine supplementation programs lapse. [22] Recurrence of goiter and new cases of cretinism have been noted in some nations where this has occurred. These changes are manifested prominently in school-aged children, who are particularly sensitive to variations in iodine intake. Thyroid volume, prevalence of goiter, and urinary iodine levels may return to pre-iodine supplementation levels 1-2 years following the discontinuation of iodine supplementation.
Morbidity
Mild to moderate iodine deficiency disorder (IDD) can cause thyroid function abnormalities and endemic goiter. Women with severe iodine deficiency are more likely to experience infertility, and pregnancy in this group is more likely to result in miscarriage or congenital anomalies. Thyroid hormones are essential for fetal brain growth and development, and severe maternal iodine deficiency may lead to intellectual disability and growth retardation or cretinism in offspring, and even mild maternal iodine deficiency has been associated with lower IQ in children. [17] One systematic review of the impact of iodine supplementation in populations with mild-to-moderate iodine deficiency found improvement in some maternal thyroid indices and modest benefits on cognitive function in school-age children, even in marginally iodine-deficient areas. [23]
Whether iodine deficiency causes an increased risk for thyroid cancer is unclear, but a higher proportion of more aggressive thyroid cancers (ie, follicular thyroid carcinoma) and an increased thyroid cancer mortality rate are found in areas where iodine deficiency is endemic.
Excess iodine intake has been linked to higher all-cause mortality relative to those with adequate iodine intake. [24]
Patient Education
The public must understand the importance of using iodized salt, especially in the United States, where iodization of salt is not mandated by law. Several areas of the world, including the United States, Australia, and the Netherlands, where iodine deficiency was eradicated by voluntary methods, have later shown a significant decrease in iodine intake.
-
Iodine Deficiency. Distribution of iodine deficiency in developing countries.
-
Iodine Deficiency. Typical endemic goiters in 3 women from the Himalayas, an area of severe iodine deficiency. Image courtesy of F. DeLange.
-
Iodine Deficiency. A man and 3 females (age range, 17-20 y) with myxedematous cretinism from the Republic of the Congo in Africa, a region with severe iodine deficiency. Image courtesy of F. DeLange.
-
Iodine Deficiency. Histologic sections from a normal thyroid and from an endemic goiter that was removed because of compressive symptoms. The normal thyroid (A) contains thyroid cells arranged in a monolayered sheet around a storage form of thyroid hormone, colloid, while the endemic goiter (B) shows intense hyperplasia with no colloid. Image courtesy of F. DeLange.