Practice Essentials
Systemic inflammatory response syndrome (SIRS) is a clinical syndrome characterized by a systemic inflammatory response to an infectious or noninfectious trigger. It involves the release of proinflammatory mediators that can cause endothelial damage, microvascular thrombosis, and organ failure. The diagnostic criteria for SIRS include the presence of two or more of the following (see Presentation and Workup) [1] :
-
Body temperature >38°C (100.4°F) or < 36°C (96.8°F)
-
Heart rate >90 beats/min
-
Respiratory rate >20 breaths/min or arterial carbon dioxide tension (PaCO2) < 32 mm Hg
-
Abnormal white blood cell (WBC) count (>12,000/µL or < 4000/µL or >10% immature [band] forms)
The term Sepsis-2 refers to the definitions and criteria for sepsis and septic shock established by the Second International Consensus Definitions for Sepsis and Septic Shock in 2001. [2] Sepsis-2 defined sepsis as a suspected or confirmed infection accompanied by two or more SIRS criteria.
In 2016, the Society of Critical Care Medicine (SCCM) and the European Society of Intensive Care Medicine (ESICM) led a task force to propose a new definition for sepsis: Sepsis-3, defined as "life-threatening organ dysfunction caused by a dysregulated host response to infection." [3, 4] This created a paradigm shift in the sepsis landscape.
The Sequential Organ Failure Assessment (SOFA), a nondiagnostic intensive care unit (ICU) mortality prediction score created in 1998 [5] that was largely not designed to predict mortality like the Acute Physiology and Chronic Health Evaluation (APACHE) II and the Simplified Acute Physiology Score (SAPS), was recommended by the 2016 SCCM/ESICM Task Force, owing to its superior validity for predicting for in-hospital mortality as compared with SIRS. [3, 4] In other words, SOFA was endorsed by the task force for identification of hospitalized patients at risk for death due to sepsis. The SOFA severity score comprises the following system assessments:
-
Respiratory system - The ratio of arterial oxygen tension (PaO2) to fraction of inspired oxygen (FiO2)
-
Cardiovascular system - Mean arterial pressure (MAP) and the need for vasopressors
-
Hepatic system - Bilirubin level
-
Coagulation system - Platelet count
-
Neurologic system - Glasgow Coma Score (GCS)
-
Renal system - Serum creatinine or urine output
SOFA as a clinical tool can be accessed here: SOFA Calculator.
Although the definition of Sepsis-3 does not use SIRS criteria for diagnosis, the pathophysiologic processes present in sepsis and noninfectious SIRS are similar (see Pathophysiology and Etiology), making a discussion of SIRS in critical illness appropriate. (See the image below.)
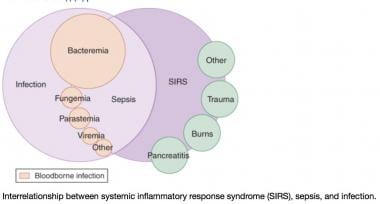 A Venn diagram of the systemic inflammatory response syndrome (SIRS). The diagram shows the overlap between infection, bacteremia, sepsis, SIRS, and multiorgan dysfunction. This perspective shows that not only infection can cause SIRS. Courtesy of emDocs.net (https://www.emdocs.net/mimics-of-sepsis/).
A Venn diagram of the systemic inflammatory response syndrome (SIRS). The diagram shows the overlap between infection, bacteremia, sepsis, SIRS, and multiorgan dysfunction. This perspective shows that not only infection can cause SIRS. Courtesy of emDocs.net (https://www.emdocs.net/mimics-of-sepsis/).
Bacteremia, sepsis, and septic shock
Infection is defined as "a microbial phenomenon characterized by an inflammatory response to the microorganisms or the invasion of normally sterile tissue by those organisms."
Bacteremia is the presence of bacteria within the bloodstream, but this condition does not always lead to SIRS or sepsis. Sepsis is the systemic response to infection and is defined as the presence of SIRS in addition to a documented or presumed infection. Severe sepsis—though the term is no longer used—meets the aforementioned criteria and is associated with organ dysfunction, hypoperfusion, or hypotension. (See Etiology, Treatment, and Medication.)
Sepsis-induced hypotension is defined as "the presence of a systolic blood pressure of less than 90 mm Hg or a reduction of more than 40 mm Hg from baseline in the absence of other causes of hypotension." Patients meet the criteria for septic shock if they have persistent hypotension and perfusion abnormalities despite adequate fluid resuscitation. Multiple organ dysfunction syndrome (MODS) is a state of physiologic derangements in which organ function is not capable of maintaining homeostasis. (See Pathophysiology.)
Pathophysiology
Regardless of its etiology, SIRS has the same pathophysiologic properties, with minor differences in inciting cascades. Many consider the syndrome a self-defense mechanism. Inflammation is the body's response to nonspecific insults that arise from chemical, traumatic, or infectious stimuli. The inflammatory cascade is a complex process that involves humoral and cellular responses, complement, and cytokine cascades. Bone [1] best summarized the relationship between these complex interactions and SIRS, describing it in terms of the following three-stage process.
Stage I
Following an insult, cytokines are produced within immune effector cells de novo at the site. Local cytokine production incites a cellular inflammatory response, thereby promoting wound repair and recruitment of the reticular endothelial system. This process is essential for normal host defense homeostasis, and its absence is not compatible with life. Local inflammation (eg, in the skin and subcutaneous soft tissues) carries the classic description of rubor, tumor, dolor, calor and functio laesa:
-
Rubor (redness) - This reflects local vasodilation caused by release of local vasodilating substances such as nitric oxide (NO) and prostacyclin
-
Tumor (swelling) - This is due to vascular endothelial tight junction disruption and the local extravasation of protein-rich fluid into the interstitium, which also allows activated WBCs to pass from the vascular space into the tissue space to help clear infection and promote repair
-
Dolor (pain) - This represents the impact inflammatory mediators have on local somatosensory nerves; presumably, the pain stops the host from trying to use this part of the body as it tries to repair itself
-
Calor (heat) - The increased heat is due primarily to increased blood flow but also to increased local metabolism as WBCs become activated and localize to the injured tissue
-
Functio laesa (loss of function) - This is a hallmark of inflammation and a common clinical finding of organ dysfunction when the infection is isolated to a specific organ (eg, pneumonia—acute respiratory failure; kidney—acute kidney injury).
Importantly, on a local level, this cytokine and chemokine release by attracting activated leukocytes to the region may cause local tissue destruction or cellular injury.
Stage II
Small quantities of local cytokines are released into the circulation, improving the local response. This leads to growth factor stimulation and the recruitment of macrophages and platelets. This acute-phase response is typically well controlled by a decrease in the proinflammatory mediators and by the release of endogenous antagonists; the goal is homeostasis. At this stage, some minimal malaise and low-grade fever may become manifest.
Stage III
If homeostasis is not restored and if the inflammatory stimuli continue to seed into the systemic circulation, a significant systemic reaction occurs. The cytokine release leads to destruction rather than protection. A consequence of this is the activation of numerous humoral cascades and the activation of the reticular endothelial system and subsequent loss of circulatory integrity. This leads to end-organ dysfunction.
Multiple-hit theory
Bone also endorsed a multiple-hit theory behind the progression of SIRS to organ dysfunction and possibly to MODS. In this theory, the event that initiates the SIRS cascade primes the pump, and with each additional event, an altered or exaggerated response occurs, leading to progressive illness. The key to preventing the multiple hits is adequate identification of the cause of SIRS followed by appropriate resuscitation and therapy.
Inflammatory cascade
Trauma, inflammation, or infection leads to the activation of the inflammatory cascade. Initially, a proinflammatory activation occurs, but almost immediately thereafter, a reactive suppressing anti-inflammatory response occurs. This SIRS usually manifests itself as increased systemic expression of both proinflammatory and anti-inflammatory species. When SIRS is mediated by an infectious insult, the inflammatory cascade is often initiated by endotoxin or exotoxin. Tissue macrophages, monocytes, mast cells, platelets, and endothelial cells are able to produce a multitude of cytokines. The cytokines tissue necrosis factor (TNF)-α and interleukin (IL)-1 are released first and initiate several cascades.
The release of IL-1 and TNF-α (or the presence of endotoxin or exotoxin) leads to cleavage of the nuclear factor (NF)-κB inhibitor. Once the inhibitor is removed, NF-κB is able to initiate the production of messenger RNA (mRNA), which induces the production other proinflammatory cytokines.
IL-6, IL-8, and interferon gamma are the primary proinflammatory mediators induced by NF-κB. In-vitro research suggests that glucocorticoids may function by inhibiting NF-κB. TNF-α and IL-1 have been shown to be released in large quantities within 1 hour of an insult and to exert both local and systemic effects. In-vitro studies have shown that these two cytokines produce no significant hemodynamic response when given individually but cause severe lung injury and hypotension when given together. TNF-α and IL-1 are responsible for fever and the release of stress hormones (norepinephrine, vasopressin, activation of the renin-angiotensin-aldosterone system).
Other cytokines, especially IL-6, stimulate the release of acute-phase reactants such as C-reactive protein (CRP) and procalcitonin. It is noteworthy that infection has been shown to induce a greater release of TNF-α—and consequently a greater release of IL-6 and IL-8—than trauma does. This is suggested to be the reason why a higher fever is associated with infection as compared with trauma.
The proinflammatory interleukins either function directly on tissue or work via secondary mediators to activate the coagulation cascade and the complement cascade and the release of NO, platelet-activating factor, prostaglandins, and leukotrienes.
High mobility group box 1 (HMGB1) is a protein present in the cytoplasm and nuclei in a majority of cell types. In response to infection or injury, as is seen with SIRS, HMGB1 is secreted by innate immune cells, released passively by damaged cells, or both. Thus, elevated serum and tissue levels of HMGB1 would result from many of the causes of SIRS.
HMGB1 acts as a potent proinflammatory cytokine and is involved in delayed endotoxin lethality and sepsis. [6] In an observational study of patients with traumatic brain injury, multivariate analysis selected plasma HMGB1 level as an independent predictor for 1-year mortality and unfavorable outcome. [7] Therapeutic studies are under way to evaluate various mechanisms for blocking HMGB1, with hopes of improving outcomes in SIRS and sepsis syndromes. [6]
Numerous proinflammatory polypeptides are found within the complement cascade. The protein complements C3a and C5a have been the most studied and are believed to contribute directly to the release of additional cytokines and to cause vasodilatation and increasing vascular permeability. Prostaglandins and leukotrienes incite endothelial damage, leading to multiorgan failure.
Studies have shown that polymorphonuclear cells (PMNs) from critically ill patients with SIRS are more resistant to activation than PMNs from healthy donors but, when stimulated, demonstrate an exaggerated microbicidal response. This may represent an autoprotective mechanism in which the PMNs in the already inflamed host may avoid excessive inflammation, thereby reducing the risk of further host cell injury and death. [8]
Coagulation
The correlation between inflammation and coagulation is critical for understanding the potential progression of SIRS. IL-1 and TNF-α directly affect endothelial surfaces, leading to the expression of tissue factor (TF). TF initiates the production of thrombin, thereby promoting coagulation, and is a proinflammatory mediator itself. Fibrinolysis is impaired by IL-1 and TNF-α via production of plasminogen activator inhibitor (PAI)-1. Proinflammatory cytokines also disrupt the naturally occurring anti-inflammatory mediators antithrombin and activated protein C (APC).
If unchecked, this coagulation cascade leads to complications of microvascular thrombosis, including organ dysfunction. The complement system also plays a role in the coagulation cascade. Procoagulant activity related to infection is generally more severe than that produced by trauma.
SIRS vs CARS
The cumulative effect of this inflammatory cascade is an unbalanced state with inflammation and coagulation dominating. To counteract the acute inflammatory response, the body is equipped to reverse this process via the counterinflammatory response syndrome (CARS). IL-4 and IL-10 are cytokines responsible for decreasing the production of TNF-α, IL-1, IL-6, and IL-8. In fact, this proinflammatory and anti-inflammatory activation mirrors other homeostatic processes, such as coagulation, anticoagulation, complement activation, and complement suppression.
The normal homeostatic processes attempt to keep these highly toxic inflammatory processes in check. Inflammation is an essential component of host defense and serves a strongly positive survival function in suppressing and then eliminating local infection and tissue injury. It is only when this localized aggressive process gains access to the whole body through the bloodstream and lymphatic vessels that SIRS develops.
The acute-phase response also produces antagonists to TNF-α and IL-1 receptors. These antagonists either bind the cytokine, thereby inactivating it, or block the receptors. Comorbidities and other factors can influence a patient's ability to respond appropriately.
The balance between SIRS and CARS helps determine a patient's outcome after an insult. It is possible that because of CARS, medications meant to inhibit the proinflammatory mediators may lead to deleterious immunosuppression.
Etiology
The etiology of SIRS is broad and includes the following:
-
Infectious and noninfectious conditions
-
Surgical procedures
-
Trauma
-
Medications
-
Other therapies
The inciting molecular stimuli inducing this generalized inflammatory reaction fall into two broad categories: pathogen-associated molecular patterns (PAMPs) and damage-associated molecular patterns (DAMPs). PAMPs become present when infection of foreign cell lysis releases these foreign molecules intrinsic to their structure into the circulation, whereas DAMPs arise when cellular injury occurs at rates that overwhelm local clearance mechanisms. Thus, it can be seen that generalized bacteremia, severe pneumonia (viral or bacterial), severe trauma with tissue injury, and pancreatitis all share common inflammatory activation pathways.
The following is a partial list of infectious causes of SIRS:
-
Bacterial sepsis
-
Burn wound infections
-
Candidiasis
-
Cellulitis
-
Cholecystitis
-
Community-acquired pneumonia [9]
-
Diabetic foot infection
-
Erysipelas
-
Infective endocarditis
-
Influenza
-
Intra-abdominal infections (eg, diverticulitis, appendicitis)
-
Gas gangrene
-
Meningitis
-
Nosocomial pneumonia
-
Pseudomembranous colitis
-
Pyelonephritis
-
Septic arthritis
-
Urinary tract infections (male and female)
-
Total joint arthroplasty infection [10]
The following is a partial list of noninfectious causes of SIRS:
-
Acute mesenteric ischemia
-
Adrenal insufficiency
-
Autoimmune disorders
-
Burns
-
Chemical aspiration
-
Cirrhosis
-
Cutaneous vasculitis
-
Dehydration
-
Drug reaction
-
Electrical injuries
-
Erythema multiforme
-
Hemorrhagic shock
-
Hematologic malignancy
-
Intestinal perforation
-
Medication side effect (eg, from theophylline)
-
Myocardial infarction
-
Pancreatitis [11]
-
Seizure
-
Substance abuse - Stimulants such as cocaine and amphetamines
-
Surgical procedures
-
Toxic epidermal necrolysis
-
Transfusion reactions
-
Upper gastrointestinal (GI) bleeding
-
Vasculitis
Epidemiology
US and international statistics
The true incidence of SIRS is not known. Not all patients with SIRS require hospitalization or have diseases that progress to serious illness. Indeed, patients with a seasonal head cold due to rhinovirus usually fulfill the criteria for SIRS. Because SIRS criteria are nonspecific and occur in patients who present with conditions ranging from influenza to cardiovascular collapse associated with severe pancreatitis, [11] any incidence figures would need to be stratified according to SIRS severity.
In a prospective survey of patients admitted to a tertiary care center, Rangel-Fausto et al determined that 68% of hospital admissions to surveyed units met SIRS criteria. [12] The incidence of SIRS increased as the level of unit acuity increased. The following progression of patients with SIRS was noted: 26% developed sepsis, 18% developed severe sepsis, and 4% developed septic shock within 28 days of admission.
A hospital survey of SIRS performed by Pittel et al revealed an overall in-hospital incidence of 542 episodes per 1000 hospital days. [13] In comparison, the incidence in the ICU was 840 episodes per 1000 hospital days. It is not clear what percentage of patients with SIRS have a primary infectious etiology that allows them to be classified as having sepsis. It is most likely, however, that the proportion of SIRS patients varies across patient and hospital groups—for example, being highest in acute care settings and in those with immune deficiency.
The etiology in patients admitted with severe sepsis from a community emergency department (ED) was evaluated by Heffner et al, who determined that 55% of patients had negative cultures and 18% were diagnosed with noninfectious causes that mimicked sepsis (SIRS). [14] Many of the noninfectious etiologies (eg, pulmonary embolism, myocardial infarction, and pancreatitis) required urgent alternative disease-specific therapy. In the SIRS patients without infection, the clinical characteristics were similar to those in the patients with positive cultures.
Another study demonstrated that 62% of patients who presented to the ED with SIRS had a confirmed infection, whereas 38% did not. [15] Within the same cohort of patients, 38% of infected patients did not present with SIRS.
Angus et al found the incidence of severe SIRS associated with infection to be 3 cases per 1,000 population, or 2.26 cases per 100 hospital discharges. [16] The real incidence of SIRS, therefore, must be much higher and likely depends to some degree on the rigor with which the definition is applied.
Internationally, no geography-based differences in the frequency of SIRS have been defined.
Age- and sex-related demographics
Extremes of age (young and old) and concomitant comorbidities probably affect SIRS outcomes negatively. Young people may be able to mount a more exuberant inflammatory response to a challenge than older people can, and they may also be able to better modify the inflammatory state (via CARS). Young people have better outcomes for equivalent diagnoses.
The sex-based mortality risk of severe SIRS is unknown. Because of the mitigating aspects of estrogen, females tend to have less inflammation from the same degree of proinflammatory stimuli. The reasons are not completely known, but estrogen sustains adrenergic receptor activity in inflammation, when, in its absence, adrenergic receptor downregulation occurs. Thus, premenopausal females tend to have less vasoplegia and to respond more vigorously to resuscitation. This equates to women having a 10-year age benefit over men. Mortality in women with severe sepsis is similar to that in men 10 years younger; however, whether this protective effect applies to women with noninfectious SIRS is unknown.
Prognosis
Comstedt et al, in a study focusing on SIRS in acutely hospitalized medical patients, found 28-day mortality to be 6.9 times higher in SIRS patients than in non-SIRS patients. [15] Most deaths occurred in SIRS patients with an associated malignancy.
Prognosis depends on the etiologic source of SIRS, as well as on associated comorbidities. The mortality figures in the previously mentioned study by Rangel-Fausto et al were 7% for SIRS, 16% for sepsis, 20% for severe sepsis, and 46% for septic shock. [12] The median time interval from SIRS to sepsis was inversely related to the number of SIRS criteria met. Morbidity is related to the causes of SIRS, complications of organ failure, and the potential for prolonged hospitalization.
However, a large retrospective study of Australia and New Zealand ICU care over the period 2000-2012 found a clear progressive decline in severe sepsis and septic shock mortality, from 35% to 18%, with equal trends across all age groups and treatment settings. [17] These data suggest that attention to detail, using best practices and overall quality care, has nearly halved mortality from severe sepsis, independently of any specific treatment. Thus, attention to overall patient status and use of proven risk reduction approaches (eg, stress ulcer prophylaxis, deep vein thrombosis [DVT] prophylaxis, daily awakening, and weaning trials in ventilator-dependent patients) are central to improving outcomes.
Pittet et al showed that control patients had the shortest hospital stay, whereas patients with SIRS, sepsis, and severe sepsis required progressively longer hospital stays. [13]
A study by Shapiro et al evaluated mortality in patients with suspected infection in the ED and found the following in-hospital death rates [18] :
-
Suspected infection without SIRS - 2.1%
-
Sepsis - 1.3%
-
Severe sepsis - 9.2%
-
Septic shock - 28%
In this study, the presence of SIRS criteria alone had no prognostic value for either in-hospital mortality or 1-year mortality. Each additional organ dysfunction increased the risk of mortality at 1 year. The authors concluded that organ dysfunction was a better predictor of mortality than SIRS criteria were.
Sinning et al evaluated the SIRS criteria in patients who underwent transcatheter aortic valve implantation (TAVI) and found that SIRS appeared to be a strong predictor of mortality. [19] The occurrence of SIRS was characterized by a significantly elevated release of IL-6 and IL-8, with subsequent increases in the leukocyte count, CRP, and procalcitonin. The occurrence of SIRS was related to 30-day and 1-year mortality (18% vs 1.1% and 52.5% vs 9.9%, respectively) and independently predicted 1-year mortality risk.
In the aforementioned Heffner et al study, in-hospital mortality was lower in SIRS patients without an identified infection than in patients with an infectious etiology for their SIRS (9% vs 15%). [14]
McConnell et al found that nearly 10% of patients with infections of a total knee or hip arthroplasty developed SIRS that led to increases in duration of hospitalization, ICU admissions, and 2-year reoperation and death rates. [10]
The reformulated definitions by the 2016 SCCM/EISCM task force specified that (1) sepsis requires organ dysfunction and (2) the concepts of SIRS and severe sepsis are eliminated. Furthermore, the task force recommended SOFA as the tool to assess severity of organ dysfunction in potentially septic patients, on the grounds that SOFA has superior predictive validity for in-hospital mortality as compared with SIRS. [4]
Patient Education
Education should ideally target the patient's family. Family members need to understand the fluid nature of immune responsiveness and to realize that SIRS is a potential harbinger of other more dire syndromes.
-
A Venn diagram of the systemic inflammatory response syndrome (SIRS). The diagram shows the overlap between infection, bacteremia, sepsis, SIRS, and multiorgan dysfunction. This perspective shows that not only infection can cause SIRS. Courtesy of emDocs.net (https://www.emdocs.net/mimics-of-sepsis/).

