Practice Essentials
The term gallbladder mucocele refers to an overdistended gallbladder filled with mucoid or clear and watery content. Usually noninflammatory, it results from outlet obstruction of the gallbladder and is commonly caused by an impacted stone in the neck of the gallbladder or in the cystic duct. (See the image below.)
 Stone in neck of gallbladder, with postacoustic shadowing. Minimal wall thickening and dilated gallbladder suggest mucocele.
Stone in neck of gallbladder, with postacoustic shadowing. Minimal wall thickening and dilated gallbladder suggest mucocele.
Signs and symptoms
Symptoms of a gallbladder mucocele include the following:
-
Right-upper-quadrant (RUQ) pain or epigastric pain and discomfort
-
Nausea and vomiting
The following suggest other conditions:
-
Continuance of pain or persistence of tenderness for longer than 6 hours - Acute cholecystitis
-
Fever and chills - Infected bile, with possible gallbladder empyema
-
Jaundice - Coexisting obstruction of the common bile duct (CBD)
Physical findings include the following:
-
Minimal acute inflammatory signs
-
Large, palpable, somewhat tender mass
See Presentation for more detail.
Diagnosis
Laboratory studies that may be helpful include the following:
-
White blood cell (WBC) count - Mild leukocytosis with a left shift is common; higher counts suggest acute cholecystitis or infected bile
-
Bilirubin - Usually within the reference range but may be mildly raised with Mirizzi syndrome or associated CBD obstruction or cholangitis
-
Liver enzymes - Usually within the reference range, though alkaline phosphatase may be mildly elevated; large increases suggest an obstructed CBD
-
Serum amylase levels - Usually within the reference range; large increases suggests acute pancreatitis
Imaging modalities that may be considered include the following:
-
Ultrasonography - Extremely sensitive in detecting gallbladder stones and identifying intrahepatic biliary tree dilatation
-
Plain radiography of the abdomen - Nonspecific, used only as a guideline in differential diagnosis
-
Scintigraphy (hepato-iminodiacetic acid [HIDA] scanning) - Capable of offering only indirect evidence but possible worth considering in obscure cases
-
Computed tomography (CT) - Indicated when the diagnosis is unclear or other associated conditions or complications are present that must be assessed
-
Magnetic resonance cholangiopancreatography (MRCP)
See Workup for more detail.
Management
Surgery is definitive treatment for gallbladder obstruction, and no absolute contraindication to such treatment exists. However, the following factors may be considered:
-
The presence of any associated medical conditions or illnesses that preclude surgery would constitute a contraindication to surgical treatment.
-
Laboratory research suggests that chemical ablation of the gallbladder mucosa may be an alternative in patients who are medically unfit, elderly, or critically ill
Surgical options include the following:
-
Laparoscopic cholecystectomy - The criterion standard procedure
-
Open cholecystectomy - An option for patients who have a very large gallbladder, greatly thickened gallbladder walls, or an obliterated triangle of Calot
-
Percutaneous or open cholecystostomy - A temporary measure, usually performed when the patient is very sick or the dissection is technically very difficult and followed by a completion cholecystectomy
-
Laparoscopic subtotal cholecystectomy - An option for very difficult gallbladder dissections in which the inflammation is very severe and in the region of the neck
See Treatment for more detail.
Background
Mucocele (hydrops) of the gallbladder is a term denoting an overdistended gallbladder filled with mucoid or clear and watery content. [1] The condition can result from gallstone disease, the most common affliction of the biliary system. Gallstone disease affects 15-20% of the US population, with nearly 1 million new cases reported annually. [2, 3, 4]
The gallbladder mucocele distention, which is usually noninflammatory, results from an outlet obstruction of the gallbladder and is commonly caused by an impacted stone in the neck of the gallbladder or in the cystic duct. [2, 3, 5, 6]
No single laboratory test is diagnostic of a gallbladder mucocele. However, laboratory workup should include all tests performed for acute cholecystitis. Ultrasonography (US) is extremely sensitive in detecting stones in the gallbladder; other imaging modalities may be helpful in certain circumstances (see Workup).
Cholecystectomy is the definitive treatment for an obstructed gallbladder. Medical approaches may be considered in specific circumstances (see Treatment).
Pathophysiology
Long-standing obstruction to the gallbladder’s outflow results in overdistention of the gallbladder; occasionally, the gallbladder assumes massive proportions, and its volume may reach 1.5 L. The bile or bile pigment is slowly resorbed, and continuing secretion from the mucosa of the gallbladder results in clear and watery or mucoid content (white bile).
The gallbladder wall may be of normal thickness, though in long-standing cases, the mucosa atrophies and the wall becomes thin, sometimes even transparent. Wall thickening can occur with recurrent attacks of cholecystitis (see the image below). The contents are usually sterile, and any bacterial contamination ends in empyema of the gallbladder.
 Distended gallbladder with evidence of adhesions on its wall. Irregular surface indicates recurrent attacks of cholecystitis.
Distended gallbladder with evidence of adhesions on its wall. Irregular surface indicates recurrent attacks of cholecystitis.
Gross overdistention may result in gangrene or perforation of the gallbladder, with ensuing pericholecystic collection or peritonitis. The severity of the inflammatory episode dictates the clinical presentation.
Microscopic examination reveals a flattened mucosa lined by low columnar or cuboidal cells; the increased intraluminal pressure results in plentiful Rokitansky-Aschoff sinuses. Inflammatory cells may be present, either in small numbers or in abundance. [2, 3, 5]
Etiology
Causes of gallbladder mucoceles include the following:
-
Impacted stone in the gallbladder neck or cystic duct
-
Spontaneously resolved acute cholecystitis
-
Tumors - Polyps or malignancy of the gallbladder
-
Extrinsic compression of the neck or the cystic duct by lymph nodes or inflammatory fibrosis or by adjacent malignancies in the liver, duodenum, or colon
-
Prolonged total parenteral nutrition or ceftriaxone therapy
-
Congenital narrowing of the cystic duct
-
Parasites (eg, Ascaris)
In infants and children, acute, acalculous, noninflammatory hydrops of the gallbladder may be associated with the following:
-
Kawasaki syndrome (mucocutaneous lymph node syndrome) [7]
-
Streptococcal pharyngitis
-
Mesenteric adenitis
-
Typhoid
-
Leptospirosis
-
Hepatitis
-
Familial Mediterranean fever
-
Nephrotic syndrome
-
Fibrocystic disease
Epidemiology
About 3% of all pathologic gallbladders in adults are mucoceles. Because different authors use varying criteria to define the condition, the true prevalence of gallbladder mucocele may be higher. [2, 3, 8] Some reports indicate that an association could exist between mucoceles and solitary stones of the gallbladder. [9]
Prognosis
The prognosis is excellent if the diagnosis is correct and no complications have ensued.
Complications may develop when progressive inflammation leads to acute cholecystitis and all its attendant manifestations.
In addition, bacterial contamination of the bile can lead to empyema of the gallbladder, in which case the patient will usually have a toxic and ill appearance. Gas-producing organisms may lead to an emphysematous gallbladder; air bubbles in the wall of the gallbladder can be visualized by means of plain radiography, US, or computed tomography (CT).
Another potential complication is perforation of the gallbladder (see the first image below) with ensuing pericholecystic abscess or fluid collection and peritonitis (see the second image below); the diagnosis is usually strongly suspected on clinical grounds. Pseudomyxoma peritonei may result from the rupture of a true mucocele of the gallbladder.
 Subserosal perforation of acute, emphysematous, acalculous cholecystitis in a 58-year-old diabetic man. Patient presented with features suggestive of ileus. He had high intrathoracic liver (and gallbladder), and clinical signs were atypical. Green color is unusual.
Subserosal perforation of acute, emphysematous, acalculous cholecystitis in a 58-year-old diabetic man. Patient presented with features suggestive of ileus. He had high intrathoracic liver (and gallbladder), and clinical signs were atypical. Green color is unusual.
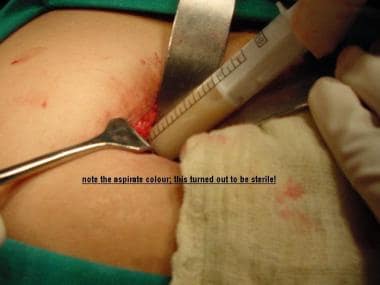 Yellowish aspirate from gallbladder of a 28-year-old woman who presented with features of right upper quadrant peritonitis. Slightly yellowish fluid was sterile and was rich in cholesterol.
Yellowish aspirate from gallbladder of a 28-year-old woman who presented with features of right upper quadrant peritonitis. Slightly yellowish fluid was sterile and was rich in cholesterol.
Perforation of the gallbladder into the intestinal tract results in a cholecystenteric fistula. This occurs when the stone erodes into adjacent bowel, usually the duodenum. Gas in the biliary tree may be evident on plain radiographs of the abdomen or on ultrasonograms. If the stone is large, this may result in obstruction of the distal small bowel, leading to gallstone ileus.
Large gallbladders may compress the pylorus or duodenum, causing gastric outlet obstruction. [2, 10]
-
Image is from a 35-year-old woman who presented with recurrent episodes of right upper quadrant colic; most recent attack was 3 days before. Gross wall thickening is apparent; this is usually measured on anterior wall of gallbladder. Also apparent are clear content, stone in neck of gallbladder, and absence of pericholecystic fluid. All favor diagnosis of acute cholecystitis.
-
Stone in neck of gallbladder, with postacoustic shadowing. Minimal wall thickening and dilated gallbladder suggest mucocele.
-
Transverse scan shows stone in neck of gallbladder, with postacoustic shadowing. Minimal wall thickening and dilated gallbladder are also visible.
-
Transverse scans show layering of gallbladder wall; this suggests edema and indicates acute cholecystitis.
-
Longitudinal scan shows layering, with fluid in wall of gallbladder and impacted stone in neck of gallbladder. Intraluminal shadowing indicates sediments in fluid; image indicates acute cholecystitis with possible pyocele of gallbladder.
-
Cluster of impacted calculi in neck of gallbladder, minimal wall thickening, and clear content; this indicates mucocele of gallbladder.
-
Cluster of calculi with postacoustic shadowing in neck of gallbladder, normal wall, and clear content; this indicates mucocele of gallbladder.
-
Distended gallbladder with evidence of adhesions on its wall. Irregular surface indicates recurrent attacks of cholecystitis.
-
Yellowish aspirate from gallbladder of a 28-year-old woman who presented with features of right upper quadrant peritonitis. Slightly yellowish fluid was sterile and was rich in cholesterol.
-
Subserosal perforation of acute, emphysematous, acalculous cholecystitis in a 58-year-old diabetic man. Patient presented with features suggestive of ileus. He had high intrathoracic liver (and gallbladder), and clinical signs were atypical. Green color is unusual.
-
Laparoscopic view of distended gallbladder in woman aged 70 years with sudden onset of severe right upper abdominal pain.
-
Stone being extracted from cystic duct through small ductotomy.








