Background
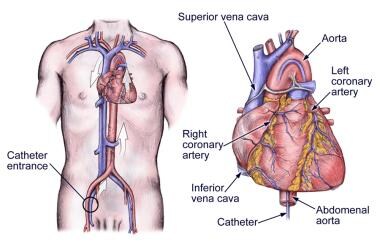
Although the technique and accuracy of noninvasive testing continue to improve, cardiac catheterization (see the image below) remains the standard for the evaluation of hemodynamics. Cardiac catheterization helps provide not only intracardiac pressure measurements but also measurements of oxygen saturation and cardiac output [1] (see the Cardiac Output calculator). Hemodynamic measurements usually are coupled with left ventriculography for the evaluation of left ventricular function and coronary angiography.
Coronary angiography remains the criterion standard for diagnosing coronary artery disease and is the primary method used to help delineate coronary anatomy. [2, 3] In addition to defining the site, severity, and morphology of lesions, coronary angiography helps provide a qualitative assessment of coronary blood flow and helps identify collateral vessels.
Correlation of the findings from coronary angiography with those from left ventriculography permits identification of potentially viable areas of the myocardium that may benefit from a revascularization procedure. Left ventricular function can be further evaluated during stress by using atrial pacing, dynamic exercise, or pharmacologic agents.
Indications
Cardiac catheterization is undertaken for the diagnosis of a variety of cardiac diseases. As with any invasive procedure that is associated with important complications, the decision to recommend cardiac catheterization must be based on a careful evaluation of the risks and benefits to the patient.
Indications for cardiac catheterization are as follows:
-
Identification of the extent and severity of coronary artery disease (CAD) and evaluation of left ventricular function
-
Assessment of the severity of valvular or myocardial disorders (eg, aortic stenosis or insufficiency, mitral stenosis or insufficiency, and various cardiomyopathies) to determine the need for surgical correction
-
Collection of data to confirm and complement noninvasive studies
-
Determination of the presence of CAD in patients with confusing clinical presentations or chest pain of uncertain origin
Many patients undergo cardiac catheterization before noncardiac surgery, even though it is not routinely indicated. In a report from the National Cardiovascular Data Registry CathPCI Registry, most of the patients undergoing diagnostic catheterization before noncardiac surgery were found to be asymptomatic. [4] Discovery of obstructive CAD was common, and revascularization was recommended in nearly half of these patients.
Contraindications
With the exception of patient refusal, there are no absolute contraindications for cardiac catheterization. Clearly, the risk-to-benefit ratio must be considered: Any procedure that is associated with some degree of risk should be contraindicated if the information derived from it will be of no benefit to the patient.
Relative contraindications are as follows:
-
Severe uncontrolled hypertension
-
Ventricular arrhythmias
-
Acute stroke
-
Severe anemia
-
Active gastrointestinal bleeding
-
Allergy to radiographic contrast
-
Acute renal failure
-
Uncompensated congestive failure (so that the patient cannot lie flat)
-
Unexplained febrile illness or untreated active infection
-
Electrolyte abnormalities (eg, hypokalemia)
-
Severe coagulopathy
Note that many of these factors can be corrected before the procedure, which lowers the risk. Preprocedural risk factor correction always should be considered unless the procedure is being performed in an emergency situation.
Absolute contraindications to radial artery access for left-heart cardiac catheterization include the following:
-
Patients who lack adequate collateral circulation
-
Patients with abnormal results from Allen test or plethysmography
-
Patients who may require an intra-aortic balloon pump
-
Patients who may require devices that are not compatible with sheaths smaller than 7 French
-
Patients with known upper-extremity vascular disease
-
Patients with Buerger disease (thromboangiitis obliterans) or severe Raynaud phenomenon
Relative contraindications to radial artery access for left-heart cardiac catheterization include the following:
-
Patients with chronic kidney disease who may need an arteriovenous fistula in the future
-
Patients with Raynaud phenomenon
-
Women with short stature and weak radial pulses
-
Patients with known severe innominate-subclavian artery disease
-
Patients with known internal mammary grafts contralateral to the site of entry
-
Cardiac Catheterization of Left Heart. The heart catheterization.
-
Cardiac Catheterization of Left Heart. Acute severe mitral regurgitation. Image courtesy of Olurotimi Badero, MD, FACP and www.tctmd.com.
-
Cardiac Catheterization of Left Heart. Cardiac catheterization sites.
-
Cardiac Catheterization of Left Heart. Femoral access. Image courtesy of Olurotimi Badero, MD, FACP and www.tctmd.com.
-
Cardiac Catheterization of Left Heart. Mitral stenosis tracings. Image courtesy of Olurotimi Badero, MD, FACP, and www.tctmd.com.
-
Cardiac Catheterization of Left Heart. Aortic stenosis tracings. Image courtesy of Olurotimi Badero, MD, FACP, and www.tctmd.com.
-
Cardiac Catheterization of Left Heart. Angiogram showing the left main bifurcating into the left anterior descending (LAD) and the left circumflex (LCX) arteries. Image courtesy of Olurotimi Badero, MD, FACP, and www.tctmd.com.
-
Cardiac Catheterization of Left Heart. Hypertrophic obstructive cardiomyopathy (HOCM) showing left ventricular outflow tract gradient at pull back. Image courtesy of Olurotimi Badero, MD, FACP, and www.tctmd.com.
-
Cardiac Catheterization of Left Heart. Aortogram obtained with a 6F pigtail catheter showing the ascending aorta, descending aorta, and great vessels. Image courtesy of Olurotimi Badero, MD, FACP.
-
Cardiac Catheterization of Left Heart. Chronic total occlusion of the right coronary artery (RCA). Image courtesy of Olurotimi Badero, MD, FACP.
-
Cardiac Catheterization of Left Heart. Recanalized chronic total occlusion (CTO) of the right coronary artery (RCA) after percutaneous coronary intervention. Image courtesy of Olurotimi Badero, MD, FACP.
-
Cardiac Catheterization of Left Heart. Judkins left 4 (JL4) catheter in place. Image courtesy of Olurotimi Badero, MD, FACP.
-
Cardiac Catheterization of Left Heart. Judkins right 4 (JR4) catheter in place. Image courtesy of Olurotimi Badero, MD, FACP.
-
Cardiac Catheterization of Left Heart. Left ventriculogram using a 6F pigtail catheter. Image courtesy of Olurotimi Badero, MD, FACP.
-
Cardiac Catheterization of Left Heart. Stents in the left anterior descending (LAD) and left circumflex (LCX) arteries. Image courtesy of Olurotimi Badero, MD, FACP.
-
Cardiac Catheterization of Left Heart. Left ventriculogram showing mid cavity obliteration in hypertrophic cardiomyopathy (HOCM). Image courtesy of Olurotimi Badero, MD, FACP.
-
Cardiac Catheterization of Left Heart. Angiogram showing totally occluded left main coronary artery distally. Image courtesy of Olurotimi Badero, MD, FACP.
-
Cardiac Catheterization of Left Heart. Angiogram showing recanalized left main coronary artery with critical trifurcation lesion involving the distal left main coronary artery. Image courtesy of Olurotimi Badero, MD, FACP.
-
Cardiac Catheterization of Left Heart. Image showing catheter advancing into the ascending aorta via the right radial artery in the transradial approach. Note the tortuous aorta. Image courtesy of Tak W. Kwan, MD
-
Cardiac Catheterization of Left Heart. Transradial cardiac angiogram showing pigtail catheter in the ascending aorta via a retro-esophageal subclavian artery (arteria lusoria). Image courtesy of Olurotimi Badero, MD, FACP.
-
Cardiac Catheterization of Left Heart. Tortuous brachiocephalic artery. Image courtesy of Olurotimi Badero, MD, FACP.