Background
Esophagogastroduodenoscopy (EGD) is a procedure during which a small flexible endoscope is introduced through the mouth (or, with smaller-caliber endoscopes, through the nose) and advanced through the pharynx, esophagus, stomach, and duodenum. [1] An enteroscope, a longer endoscope, can be introduced beyond the ligament of Treitz into the jejunum.
EGD is used for both diagnostic procedures and therapeutic procedures. Most modern endoscopes now use a video chip (charged coupled device) for better imaging, in contrast to the older endoscopes, which used fiberoptics for image transmission. (See the images below.)
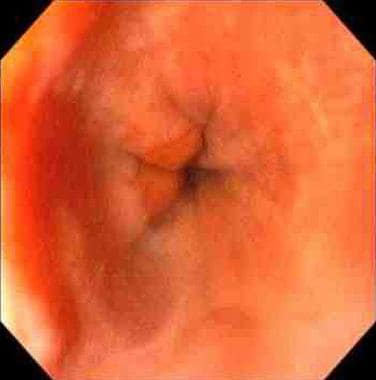
 Esophagogastroduodenoscopy (EGD). Normal vocal cords as seen prior to entering the esophagus during video EGD.
Esophagogastroduodenoscopy (EGD). Normal vocal cords as seen prior to entering the esophagus during video EGD.
In the United States, EGD is usually performed while the patient is under conscious or moderate sedation, though it can be performed with only topical anesthesia (as is common practice in Europe and Asia). General anesthesia is often used in a selected group of patients who are difficult to sedate because of chronic narcotics intake.
The procedure is usually performed in a dedicated endoscopy unit in the hospital or outpatient office setting but can also be done in the emergency department (ED), the intensive care unit (ICU), or the operating room (OR) by using portable endoscopy carts. With the aid of various types of equipment and endoscopes, endoscopic ultrasonography (EUS), endoscopic retrograde cholangiopancreatography
Indications
Indications for EGD include the following [2] :
-
Diagnostic evaluation for signs or symptoms suggestive of upper gastrointestinal (GI) disease (eg, dyspepsia, dysphagia, noncardiac chest pain, or recurrent emesis), such as gastroesophageal reflux disease (GERD) [3]
-
Biopsy for known or suggested upper GI disease (eg, malabsorption syndromes, neoplasms, or infections)
-
Therapeutic intervention (eg, retrieval of foreign bodies, [6] control of hemorrhage, dilatation or stenting of stricture, ablation of neoplasms, or gastrostomy placement)
Contraindications
Contraindications for EGD include the following:
-
Possible perforation
-
Medically unstable patients
-
Unwilling patients
-
Anticoagulation, pharyngeal diverticulum, or head and neck surgery (relative contraindications)
Diagnostic EGD is considered a low-risk procedure for bleeding in patients on anticoagulants and therefore can be performed without adjustment of anticoagulation before the procedure. [7] However, if polypectomy is contemplated or conceivable, then the patient's coagulation profile should be normalized. A risk of retropharyngeal hematoma also may be present in patients with severe coagulation abnormalities.
Certain therapeutic procedures (ie, dilations, percutaneous endoscopic gastrostomy [PEG], polypectomy, endoscopic sphincterotomy, EUS-guided fine-needle aspiration [FNA], laser ablation, and coagulation) are considered high-risk procedures for bleeding, and adjustment of anticoagulation may therefore be necessary.
Technical Considerations
Best practices
Endoscopy units are specific areas in a hospital (or physician's office) in which all endoscopic procedures are performed. For this unit to be functional and effective, according to the American Society for Gastrointestinal Endoscopy (ASGE), certain conditions must be met, [8, 9] including the following:
-
Properly trained endoscopist and nursing staff
-
Functioning and adequately maintained equipment
-
Availability of an endoscope cleaning area
-
Personnel trained to perform cardiopulmonary resuscitation
-
Quality improvement program in place
Open-access endoscopy is a system designed to offset the cost of endoscopy in stable patients without significant comorbidities who have clear indications for upper GI endoscopy. [10] The responsibilities of the referring physician are to have a complete understanding of the patient's condition and to be fully aware of the accepted indications for endoscopy. If the patient is on anticoagulation or if antibiotic prophylaxis is required, these issues must be addressed via proper communication between the referring physician and the endoscopist.
According to ASGE recommendations, training in upper GI endoscopy should include an understanding of indications, limitations, contraindications, alternatives, principles of conscious sedation, and correct interpretation of endoscopic findings. [11] A minimum of 100 upper GI endoscopic procedures has been recommended for trainees to become competent in diagnostic upper GI endoscopy.
Therapeutic upper GI endoscopy requires further training and experience to gain competency. The recommendations of the ASGE for the number of procedures required to gain competency in various therapeutic upper GI endoscopic procedures are available through the society Web site (see American Society for Gastrointestinal Endoscopy).
EGD, like other endoscopic procedures, has a substantial environmental impact (eg, through greenhouse gas emission and the creation of waste, as in single-use instruments). Accordingly, the ASGE has established a Task Force on Sustainable Endoscopy to propose ways of minimizing this impact. [12]
Procedural planning
Transnasal EGD (TN-EGD) has certain limitations in bending, which can make approaching certain gastric regions difficult. Rhee et al evaluated whether the quality and quantity of two-directional TN-EGD biopsied gastric specimens were affected by this limitation. [13] Specimen quantity was assessed on the basis of diameter and depth (μm), as well as presence of tissue layers (superficial mucosa, deep mucosa, muscularis mucosa, and submucosa). Specimen quality was assessed on the basis of anatomic orientation (good, intermediate, or poor), presence of crush artifact (none to minimal, mild, or moderate), and overall diagnostic adequacy (adequate, suboptimal, or inadequate).
Of 289 TN-EGD gastric biopsy specimens, 33 (11.4%) were of poor orientation, 26 (9.0%) revealed the presence of crush, and 37 (12.8%) demonstrated overall diagnostic inadequacy. [13] In 211 (73.0%), deep mucosa was present, but only 75 specimens (26.0%) had muscularis mucosa. The posterior aspect of the cardia had the greatest limitations in specimen quantity and quality, with the shallowest depth, poorest orientation, and poorest diagnostic adequacy. The investigators recommended paying special attention to gastric lesions located on the posterior aspect of the cardia when using two-directional TN-EGD.
In a two-part study, investigators attempted to find a good washing solution to counter the known limitations of the small-caliber water-jet nozzles of TN-EGDs for cleaning lenses. [14] Komazawa et al compared oolong tea, barley tea, and distilled water as washing solutions for the endoscopic lenses. In the first part of the study, the TN-EGD lenses were soiled by lard and then washed with one of the three washing solutions. When the image quality of photographs were judged, lenses washed with oolong tea resulted in a significantly higher image quality than did lenses washed with barley tea or distilled water solutions.
In the second part of the study, 982 patients scheduled to undergo TN-EGD were randomly assigned to groups in which the endoscope lens was washed with one of the three washing solutions. [14] The investigators found that the level of lens cleansing was significantly greater and the overall time required for endoscopy was significantly shorter in the oolong tea group than in the other two groups. When the volume of washing solution used for lens cleansing was compared, significantly less was used in the oolong group compared with the distilled water group. On the basis of their findings, Komazawa et al recommended oolong tea rather than water for cleaning TN small-caliber EGD lenses.
Complication prevention
Despite the large number of endoscopic procedures performed each day, the incidence of infection transmission via endoscopes remains very low. [15, 16] Methods of reprocessing endoscopes include mechanical cleaning, high-level disinfection, rinsing, and drying. Proper and diligent care during reprocessing of endoscopes, with attention to quality control, cannot be overstated for minimizing the risk of spreading infection via endoscopic procedures. [17]
-
Esophagogastroduodenoscopy (EGD). Normal vocal cords as seen prior to entering the esophagus during video EGD.
-
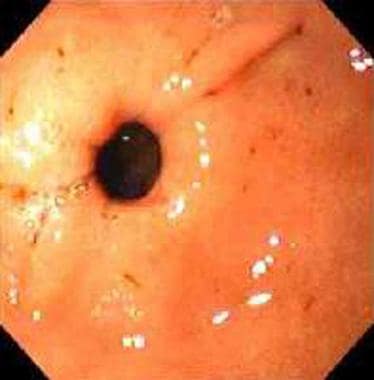
Esophagogastroduodenoscopy (EGD). Normal lower esophageal sphincter seen during EGD.
-
Esophagogastroduodenoscopy (EGD). Normal pylorus seen during EGD.
-
Esophagogastroduodenoscopy (EGD). Normal duodenum in the area of the ampulla, as seen during EGD.
-
Esophagastroduodenoscopy. Video courtesy of George Y Wu, MD, PhD.
-
This video, captured via esophagogastroduodenoscopy, shows biopsy samples being obtained from the duodenum. The duodenal folds show some "scalloping," and biopsies are obtained to rule out celiac sprue. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy, shows classic "scalloping" of the duodenal folds, a finding seen in celiac sprue. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy, shows dilation of a duodenal stricture. In this case, the patient developed an NSAIDS-related stricture. He underwent balloon dilation to relieve symptoms of nausea, vomiting, weight loss, and early satiety. The stricture had been biopsied previously to rule out malignancy. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy, depicts erosive gastritis. The antrum of the stomach is erythematous, and some erosions are noted, but no obvious ulcers. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy, depicts treatment of an arteriovenous malformation (AVM) in the small intestine using argon plasma coagulation (APC). AVMs are a common cause of gastrointestinal bleeding. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy (EGD), depicts the obtaining of biopsies of the duodenum. This is often performed during EGD to rule out certain diseases. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy, shows the treatment of a bleeding duodenal ulcer by deployment of an Endoclip. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy, shows the treatment of a duodenal ulcer with injection of epinephrine into the ulcer. The mucosa is friable and bleeds easily when manipulated. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy, shows erosive duodenitis, shallow mucosal erosions within the bulb of the duodenum. This can be caused by NSAIDS or Helicobacter pylori infection, in addition to other etiologies. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy, shows an abnormal polyp within the stomach. It is then biopsied in order to obtain a pathologic diagnosis and to rule out malignancy. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy, shows the use of the HALO 90 device in order to perform radiofrequency ablation in a patient with Barrett esophagus. Barrett esophagus increases the risk of developing esophageal cancer. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video shows the insertion of the endoscope over the mouth, into the oropharynx. The vocal cords, epiglottis, and piriformis sinuses are seen, and the scope is advanced into the right piriformis sinus and behind the epiglottis and into the esophagus. This is a normal esophageal intubation when performing esophagogastroduodenoscopy. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy, shows erythema of antrum of the stomach consistent with gastritis. Biopsies are obtained to rule out Helicobacter pylori infection. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy, shows portal hypertensive gastropathy (PHG). These are changes to the stomach mucosa caused by advanced liver disease. The mucosa has a "snake skin" appearance. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured via esophagogastroduodenoscopy, shows a moderate to severe case of portal hypertensive gastropathy (PHG). These are changes to the stomach mucosa caused by advanced liver disease. The mucosa has a "snake skin" appearance. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video shows "trachealization" of the esophagus, the finding of rings similar to those in the trachea. This is commonly seen in eosinophilic esophagitis. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video shows inflammation and erosion at the distal esophagus, erosive esophagitis. The bleeding is likely secondary to a biopsy that had been performed. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video shows severe distal reflux esophagitis via esophagogastroduodenoscopy. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video shows, in retroflexion (the scope looking back on itself), esophagogastroduodenoscopy in a patient who had a previous lap band surgery for weight loss. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video shows a normal esophagus via esophagogastroduodenoscopy. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured with esophagogastroduodenoscopy, shows an esophageal varix with a nipple, which is a sign of recent bleeding. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.
-
This video, captured with esophagogastroduodenoscopy, shows a normal Z line, which is another name for the esophageal gastric (EG) junction. Video courtesy of Dawn Sears, MD, and Dan C. Cohen, MD, Division of Gastroenterology, Scott & White Healthcare.