Practice Essentials
Acute lymphoblastic leukemia (acute lymphocytic leukemia, ALL) is a malignant (clonal) disease of the bone marrow in which early lymphoid precursors proliferate and replace the normal hematopoietic cells of the marrow. ALL is the most common type of cancer and leukemia in children in the United States. The image below shows pre–B-cell lymphoblastic leukemia/lymphoma (B-ALL).
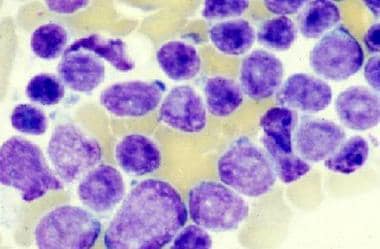 Acute lymphoblastic leukemia (ALL): Bone marrow shows proliferation of large and heterogeneous lymphoblasts consistent with pre–B-cell ALL (French-American-British L2 morphology).
Acute lymphoblastic leukemia (ALL): Bone marrow shows proliferation of large and heterogeneous lymphoblasts consistent with pre–B-cell ALL (French-American-British L2 morphology).
A proposed mechanism for some cases of childhood ALL is a two-step process of genetic mutation and exposure to infection. In contrast, most adults with ALL have no identifiable risk factors. (See Etiology).
Signs and symptoms
Signs and symptoms of ALL include the following:
-
Fever
-
Signs and symptoms of anemia, such as pallor, fatigue, dizziness, palpitations, cardiac flow murmur, and dyspnea with even mild exertion
-
Bleeding
-
Disseminated intravascular coagulation (DIC) at diagnosis (about 10% of cases)
-
Blood clots
-
Palpable lymphadenopathy
-
Symptoms related to a large mediastinal mass (eg, shortness of breath), particularly with T-cell lymphoblastic leukemia/lymphoma (T-ALL)
-
Bone pain (can be severe and often atypical)
-
Left upper quadrant fullness and early satiety due to splenomegaly (about 10% of cases)
-
Symptoms of leukostasis (eg, respiratory distress, altered mental status)
-
Kidney failure in patients with a high tumor burden
-
Infections, including pneumonia
-
Petechiae (particularly on lower extremities) and ecchymoses
-
Rashes from skin infiltration with leukemic cells
See Presentation for more detail.
Diagnosis
Laboratory tests and other studies used in the workup for ALL include the following:
-
Complete blood count with differential
-
Coagulation studies, including PT, PTT, fibrinogen and fibrin split products
-
Peripheral blood smear
-
Chemistry profile, including lactate dehydrogenase, uric acid, liver function studies, and BUN/creatinine
-
Appropriate cultures (in particular, blood cultures) in patients with fever or other signs of infection
-
Chest x-ray
-
Computed tomography, as indicated by symptoms
-
Multiple-gated acquisition scanning or echocardiogram
-
Electrocardiography
-
Lumbar puncture (especially in children)
-
Bone marrow aspiration and biopsy (definitive for confirming leukemia)
Bone marrow studies should include the following:
-
Histology
-
Immunohistochemistry/flow cytometry
-
Cytogenetics
-
Fluorescence in situ hybridization
-
Polymerase chain reaction
-
Next-generation sequencing
See Workup for more detail.
Management
Treatment of ALL is stratified on the basis of patient age (adolescent and young adult versus older) and Philadelphia chromosome status (positive versus negative)
Treatment of newly-diagnosed ALL may include the following:
-
Induction chemotherapy (eg, standard 4- or 5-drug regimen, ALL-2, or hyper-CVAD)
-
Consolidation chemotherapy
-
Maintenance chemotherapy
-
Inclusion of tyrosine kinase inhibitors for Philadelphia chromosome–positive (Ph+) disease
-
Inclusion of rituximab for CD20-positive patients (especially those < 60 years)
-
Intrathecal chemotherapy for central nervous system (CNS) prophylaxis
-
Stem cell transplantation
-
Supportive care (eg, blood products, antibiotics, growth factors)
Special considerations apply to the treatment of the following:
-
Burkitt leukemia
-
Ph+ ALL
-
ALL in older children and younger adults
-
Relapsed ALL
-
ALL in patients with hyperuricemia or at high risk for tumor lysis syndrome
See Treatment and Medication for more detail.
See also Pediatric Acute Lymphoblastic Leukemia and Acute Myeloid Leukemia (AML).
Pathophysiology
The malignant cells of ALL are lymphoid precursor cells (ie, lymphoblasts) that are arrested in an early stage of development. This arrest is caused by an abnormal expression of genes, often as a result of chromosomal translocations or abnormalities of chromosome number.
These aberrant lymphoblasts proliferate, reducing the number of the normal marrow elements that produce other blood cell lines (red blood cells, platelets, and neutrophils). Consequently, anemia, thrombocytopenia, and neutropenia occur, although typically to a lesser degree than is seen in acute myeloid leukemia. Lymphoblasts can also infiltrate outside the marrow, particularly in the liver, spleen, and lymph nodes, resulting in enlargement of the latter organs.
Etiology
A review of the genetics, cell biology, immunology, and epidemiology of childhood leukemia by Greaves concluded that B-cell precursor ALL has a multifactorial etiology, with a two-step process of genetic mutation and exposure to infection playing a prominent role. The first step occurs in utero, when fusion gene formation or hyperdiploidy generates a covert, pre-leukemic clone. The second step is the postnatal acquisition of secondary genetic changes that drive conversion to overt leukemia. Only 1% of children born with a pre-leukemic clone progress to leukemia. [1]
The second step is triggered by infection. Triggering is more likely to occur in children whose immune response is abnormally regulated because they were not exposed to infections in the first few weeks and months of life. Lack of exposure to these early infections, which prime the immune system, is more likely to occur in societies that are zealous about hygiene; this would help explain why at present, pediatric ALL is seen primarily in industrialized societies. [1]
Less is known about the etiology of ALL in adults, compared with acute myeloid leukemia (AML). Most adults with ALL have no identifiable risk factors.
Although most leukemias occurring after exposure to radiation are AML rather than ALL, an increased prevalence of ALL was noted in survivors of the Hiroshima atomic bomb but not in those who survived the Nagasaki atomic bomb.
Secondary ALL
Analysis of the Surveillance, Epidemiology and End Results (SEER) database showed that the incidence of ALL was higher than expected in patients with a prior history of Hodgkin lymphoma, small cell lung cancer, and ovarian cancer. [2]
Rare patients have an antecedent hematologic disorder (AHD) such as myelodysplastic syndrome (MDS) that evolves to ALL. However, most patients with MDS that evolves to acute leukemia develop AML rather than ALL. Some patients receiving lenalidomide as maintenance therapy for multiple myeloma have developed secondary ALL. [3] In a study of the California Cancer Registry it was noted that 3% of patients had a prior known malignancy and that any prior malignancy predisposed to the development of ALL. The prognosis for these patients with secondary ALL was unfavorable compared with that of patients with de novo ALL. [4]
Cases of ALL with abnormalities of chromosome band 11q23 following treatment with topoisomerase II inhibitors for another malignancy have been described. However, most patients who develop secondary acute leukemia after chemotherapy for another cancer develop AML rather than ALL. [5]
Genetic susceptibility
A genome-wide association study of susceptibility to ALL in adolescents and young adults identified a significant susceptibility locus in GATA3: rs3824662 (odds ratio 1.77) and rs3781093 (OR 1.73). [6] Other studies have shown increased risk of ALL in association with polymorphisms of the following [7, 8, 9] :
-
Arylamine N-acetyltransferases 1 and 2
-
MMP-8 promoter genotypes
-
HLA alleles
-
ARID5B
-
IKZF1
-
CEBPE
-
CDKN2A
-
PIP4K2A
-
LHPP
-
ELK3
Epidemiology
ALL is the most common type of cancer and leukemia in children in the United States. Median age at diagnosis is 17 years. [10] ALL accounts for 76% of pediatric leukemia cases. [11] In adults, ALL is less common than acute myeloid leukemia (AML).
The American Cancer Society estimates that 6550 cases of ALL (adult and pediatric) will occur in the United States in 2024, resulting in 1330 deaths. [11] The estimated 5-year survival is 72.0%. The favorable survival rate is due to the high cure rate of ALL in children. Prognosis declines with increasing age, and the median age at death is 60 years. [10]
Worldwide, the highest incidence of ALL occurs in Italy, the United States, Switzerland, and Costa Rica. In Europe overall, B-cell precursor ALL has been increasing by around 1% each year. [12]
Prognosis
Only 20-40% of adults with ALL are cured with current treatment regimens.
Historically, patients with ALL were divided into three prognostic groups: good risk, intermediate risk, and poor risk.
Good-risk criteria included the following:
-
No adverse cytogenetics
-
Age younger than 30 years
-
White blood cell (WBC) count of less than 30,000/μL
-
Complete remission within 4 weeks
Intermediate risk included those whose condition did not meet the criteria for either good risk or poor risk.
Poor-risk criteria included the following:
-
Adverse cytogenetics – Translocations t(9;22), t(4;11)
-
Age older than 60 years
-
Precursor B-cell WBCs with WBC count greater than 100,000/μL
-
Failure to achieve complete remission within 4 weeks
The addition of tyrosine kinase inhibitors to chemotherapy has resulted in improved prognosis of patients with Philadelphia chromosome–positive ALL such that many experts no longer consider these patients poor risk. [13]
Immunophenotype effects on prognosis
Czuczman et al studied 259 patients treated with several Cancer and Leukemia Group B (CALGB) protocols for newly diagnosed ALL and found no significant difference in response rates, remission duration, or survival for patients expressing myeloid antigens versus those not expressing myeloid antigens. [14] B-lineage phenotype was expressed in 79% of patients; one third of these coexpressed myeloid antigens. Seventeen percent of patients demonstrated T-lineage ALL; one quarter of these coexpressed myeloid antigens. [14]
T-lineage ALL was associated with younger age, male sex, presence of a mediastinal mass, higher WBC count and hemoglobin level, longer survival, and longer disease-free survival. The number of T markers expressed also had prognostic significance. Patients expressing six or more markers had longer disease-free and overall survival compared with patients expressing three or fewer markers.
In a report by Preti et al, 64 of 162 patients with newly diagnosed ALL coexpressed myeloid markers. [15] Patients coexpressing myeloid markers were significantly older, had a higher prevalence of CD34 expression, and had a lower prevalence of common ALL antigen expression than patients without myeloid expression. A trend toward a decreased remission rate was observed for patients coexpressing myeloid markers (64%) relative to those who did not coexpress such markers (78%). [15] However, no significant effect on remission duration or overall survival was observed.
Chromosome number and prognosis
The effect of chromosome number on prognosis is displayed in Table 1, below.
Table 1. Effect of Chromosome Number on Prognosis (Open Table in a new window)
Chromosome Number |
3-Year Event-Free Survival |
Near tetraploidy |
46-56% |
Normal karyotype |
34-44% |
Hyperdiploidy >50 |
32-59% |
Hyperdiploidy 47-50 |
21-53% |
Pseudodiploidy |
12-25% |
Hypodiploidy |
11% |
In a study of 428 patients with Philadelphia chromosome negative ALL treated at MD Anderson Cancer Center, 43% had a diploid karyotype. Other patients had 3 or 4 chromosomal abnormalities (6%), 5 or more chromosome abnormalities (7%), low hypodiploidy/near-triploidy (6%), or tetraploidy (1%). Six percent of patients had an mixed-lineage leukemia rearrangement and 11% had other recurrent chromosomal abnormalities. The 5-year overall survival rate was 47%. The overall survival of patients with 3 or 4 chromosomal abnormalities was similar to that of patients with diploid ALL (51%), whereas the overall survival for patients with 5 or more abnormalities was 28%. Complex karyotype and hypodiploidy/near triploidy retained their prognostic importance independent of minimal residual disease (MRD) status after treatment. [16]
Minimal residual disease
Case-specific molecular probes or multiparametric flow cytometry can be used to detect 1 leukemic cell in 10,000 mononuclear cells (ie, sensitivity of > 104). The presence of such MRD after treatment is a strong predictor for relapse.
A meta-analysis of 39 trials of ALL treatment of children and adults demonstrated that the event-free survival (EFS) hazard ratio for achieving MRD negative status after therapy was 0.23 for pediatric patients and 0.28 for adults. [17] The hazard ratio for overall survival was 0.28 for both patient populations. The effect was seen across therapies, disease subtypes and methods of detection.
Genomics
Routine use of next-generation sequencing and other molecular methods is identifying recurrent genetic abnormalities with prognostic implications. Patel et al performed genome-wide analysis (GWAS) with single-nucleotide polymorphism (SNP) arrays on 70 patients with B-ALL. The most prevalent deletions occurred in CDKN2A, IKZF1 and PAX5. [18] Other genes were affected at a lower frequency.
Liu et al performed GWAS on 264 cases of pediatric and young adult T-ALL72. NRAS/FLT3 mutations were associated with immature T-ALL, JAK3/STAT5B mutations were seen in HOXA1 deregulated ALL, PTPN2 mutations were seen in TLX1 deregulated T-ALL, and PIK3R1/PTEN mutations were seen in TAL1 deregulated ALL. Philadelphia chromosome–like ALL (a subtype of ALL with a poor prognosis that is amenable to treatment with tyrosine kinase inhibitors) was identifed by genomic studies. [19]
Further studies correlating genomic and clinical findings are ongoing. These studies will determine the prognostic implication of specific molecular findings and could allow for the development of targeted agents in these diseases.
Patient Education
Patients with ALL should be instructed to immediately seek medical attention if they are febrile or have signs of bleeding. Furthermore, while receiving chemotherapy, patients with leukemia should avoid exposure to crowds and people with contagious illnesses, especially children with viral infections.
Although activity may occur as tolerated, patients with ALL may not participate in strenuous activities such as lifting or exercise. In addition, a neutropenic diet is recommended in these individuals, as follows:
-
No fresh fruits or vegetables may be eaten
-
All foods must be cooked
-
Meats are to be cooked until well done
For patient education information, see Acute Lymphoblastic Leukemia.
-
Acute lymphoblastic leukemia (ALL): Bone marrow shows proliferation of large and heterogeneous lymphoblasts consistent with pre–B-cell ALL (French-American-British L2 morphology).
-
Pre–B-cell acute lymphoblastic leukemia: Flow cytometry of bone marrow shows that the cells are positive for CD10, CD19, CD22, CD34, and terminal deoxynucleotidyl transferase.
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Treatment
- Approach Considerations
- Induction Chemotherapy
- Consolidation Therapy
- Maintenance Therapy
- CNS Prophylaxis
- Treatment of Mature B-Cell ALL
- Treatment of Ph Chromosome–Positive ALL
- Treatment of the Younger Adult
- Transplantation
- Treatment of Relapsed ALL
- CAR T-Cell Therapy
- Supportive Care - Blood Products
- Supportive Care: Therapy and Prophylaxis for Infection
- Supportive Care: Growth Factors
- Hyperuricemia and Tumor Lysis Syndrome
- Long-Term Monitoring
- Show All
- Guidelines
- Medication
- Media Gallery
- Tables
- References

