Practice Essentials
Community-acquired pneumonia (CAP) is one of the most common infectious diseases and an important cause of mortality and morbidity worldwide. [1] Typical bacterial pathogens that cause CAP include Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. However, with the advent of novel diagnostic technologies, viral respiratory pathogens are increasingly being identified as frequent etiologies of CAP. Prior to the COVID-19 pandemic, the most common viral pathogens recovered from hospitalized adult patients admitted with CAP include human rhinovirus and influenza.
Presentation and pathogens in typical community-acquired pneumonia
The term “typical” CAP refers to a bacterial pneumonia caused by pathogens such as S pneumoniae, H influenzae, and M catarrhalis. Patients with typical CAP classically present with fever, a productive cough with purulent sputum, dyspnea, and pleuritic chest pain. Characteristic pulmonary findings on physical examination include the following [1] :
-
Tachypnea
-
Rales heard over the involved lobe or segment
-
Increased tactile fremitus, bronchial breath sounds, and egophony may be present if consolidation has occurred.
-
Decreased tactile fremitus and dullness on chest percussion may result from parapneumonic effusion or empyema.
Epidemiologic data may provide clues to the specific pathogen causing CAP:
-
The most common bacterial pathogen overall is S pneumoniae, although, in some settings, including in the United States, its incidence is decreasing, possibly owing to vaccination. [1]
-
Underlying chronic obstructive pulmonary disease (COPD) [2] : H influenzae or M catarrhalis
-
Alcoholic patient presenting with “currant jelly” sputum: Klebsiella pneumoniae [5]
Atypical community-acquired pneumonia
The clinical presentation of so-called “atypical” CAP often is subacute and frequently indolent. [1] In addition, patients with atypical CAP may present with more subtle pulmonary findings, nonlobar infiltrates on radiography, and various extrapulmonary manifestations (eg, diarrhea, otalgia).
Bacteria that cause atypical CAP include Mycoplasma pneumoniae, Chlamydia pneumoniae, and Legionella pneumophila (Legionnaires disease). Respiratory viruses that cause atypical CAP include SARS-CoV-2 (COVID-19), influenza A and B, rhinovirus, respiratory syncytial virus, human metapneumovirus, adenovirus 4 and 7, and parainfluenza virus.
Other rare CAP pathogens
Rare viruses that cause CAP include coxsackievirus, echovirus, other coronaviruses (MERS-CoV, SARS), hantavirus, Epstein-Barr virus, cytomegalovirus, herpes simplex virus, human herpesvirus 6, varicella-zoster virus, and metapneumovirus. [6]
Rare bacteria that cause CAP include Chlamydia psittaci (Psittacosis), Coxiella burnetii (Q fever), and Francisella tularensis (Tularemia). Rare mycobacteria that cause CAP include Mycobacterium tuberculosis and nontuberculous mycobacteria. Rare endemic fungi can cause subacute or chronic pneumonia; they include Histoplasma capsulatum, Blastomyces dermatitidis, Cryptococcus neoformans and Neoformans gattii, and Coccidioides immitis.
Extrapulmonary signs and symptoms
Extrapulmonary signs and symptoms seen in some forms of atypical CAP may include the following:
-
Mental confusion
-
Prominent headaches
-
Myalgias
-
Ear pain
-
Abdominal pain
-
Diarrhea
-
Rash (Horder spots in psittacosis; erythema multiforme in Mycoplasma pneumonia)
-
Nonexudative pharyngitis
-
Hemoptysis
-
Splenomegaly
-
Relative bradycardia
Historical clues and physical examination findings may suggest a causative pathogen, but the clinical signs and symptoms of CAP are not sufficiently specific to reliably differentiate the exact etiologic agent. [1, 7] Therefore, additional testing remains necessary to identify the pathogen and to optimize therapy in CAP.
Workup
Standard diagnostic studies for CAP include the following:
-
Chest radiography
-
Complete blood cell (CBC) count with differential
-
Serum blood urea nitrogen (BUN) and creatinine levels
For patients with severe CAP, patients being empirically treated for methicillin-resistant S aureus (MRSA) or Pseudomonas, or patients in whom a specific etiology is suspected, additional workup may be warranted, including the following [8] :
-
Sputum Gram stain and/or culture
-
Blood cultures
-
Serum sodium level
-
Serum transaminase levels
-
Lactic acid level
-
C-reactive protein (CRP)
-
Lactate dehydrogenase (LDH)
-
Molecular diagnostics such as multiplex polymerase chain reaction (PCR) testing
-
Urinary antigen testing for Legionella species
In special situations:
-
During influenza season, molecular assay for influenza
-
Molecular or antigen testing for SARS-CoV-2 with ongoing community transmission
-
Serologic studies for M pneumoniae, C pneumoniae, Bordetella pertussis, C burnetii
-
Creatine phosphokinase (CPK)
-
Serum phosphorus level
Chest radiography
Obtain chest radiographs in all patients with suspected CAP to evaluate for an infiltrate and to help exclude conditions that may mimic CAP, such as lung cancer or pulmonary emboli. [9, 10] Patients who present very early with CAP may have negative findings on chest radiography. CT scanning may also be necessary in immunocompromised patients who present with symptoms that suggest CAP or ambiguous symptoms in whom chest radiography findings are negative. In patients with symptomatic improvement, repeat chest imaging is generally not recommended as radiographic improvement often lags behind clinical improvement. [8]
Hospital admission
Multiple scoring systems are available to assess the severity of CAP and to assist in deciding whether a patient should be hospitalized or admitted to the intensive care unit (ICU).
The Pneumonia Severity Index (PSI) is preferred over the CURB-65 (confusion, uremia, respiratory rate, low blood pressure, age >65 years) for determining outpatient versus inpatient treatment. [8] Patients with PSI class IV-V may need hospitalization or more intensive in-home services. Even in the setting of COVID-19, PSI still was shown to be more predictive of mortality than CURB-65. [11]
The IDSA/ATS CAP guidelines define severe pneumonia as having one major or three minor criteria.
Major criteria include [8] :
-
Septic shock requiring vasopressors
-
Respiratory failure requiring mechanical ventilation.
Minor criteria include the following [8] :
-
Respiratory rate of 30 or more breaths per minute
-
PaO2/FIO2 ratio of 250 or less
-
Multilobar infiltrates
-
Confusion
-
Uremia
-
Leukopenia (WBC < 4000 cells/µl)
-
Thrombocytopenia (platelet count < 100,000/µl)
-
Hypothermia
-
Hypotension
ICU admission is recommended for any patient who requires mechanical ventilation or vasopressors. Admission to higher-acuity care or critical care also should be considered in patients with three or more minor risk factors for severe pneumonia.
Other scoring systems also may be helpful in certain populations to predict the severity of CAP. The SMART-COP score emphasizes the ability to predict the need for ventilator or vasopressor support and includes systolic blood pressure, multilobar infiltrates, serum albumin levels, respiratory rate, tachycardia, confusion, oxygenation, and pH level. An expanded CURB-65 has been shown to improve prediction of 30-day mortality. It includes LDH, thrombocytopenia, and serum albumin, along with the traditional CURB-65, and has been shown to have better prediction accuracy. The value of adding biomarkers in addition to the above scoring systems to identify patients at risk of worse outcomes is being studied. [12, 13, 14, 15, 16]
Some research indicates that the use of biomarkers, specifically procalcitonin and CRP, may further increase the ability to identify patients at increased risk for worse outcomes, although this remains controversial. [17]
Antibiotic Therapy
Adequate empiric antimicrobial therapy for CAP includes coverage for S pneumoniae and atypical bacterial pathogens. Outpatient treatment for CAP in patients with no comorbidities and no risk factors for drug-resistant S pneumoniae frequently includes the following [8] :
-
Amoxicillin 1 g PO three times a day OR
-
A macrolide (azithromycin 500 mg once and then 250 mg daily, azithromycin 500mg daily for three days, or clarithromycin 500 mg twice daily) ORr
-
Doxycycline 100 mg twice daily
Macrolide monotherapy should be used only in areas where pneumococcal resistance is less than 25%.
Treatment options for CAP in patients with comorbidities such as chronic heart, lung, liver, or renal disease; diabetes mellitus; alcoholism; malignancy; asplenia; immunosuppression; prior antibiotics within 90 days; or other risk factors for drug-resistant infection include the following:
-
Beta-lactam (amoxicillin/clavulanate 2 g/125 mg twice daily, 875 mg/125 mg twice daily, 500 mg/125 mg three times daily, or cefpodoxime 200 mg twice daily, or cefuroxime 500 mg twice daily) AND a macrolide or doxycycline OR
-
Respiratory fluoroquinolones (moxifloxacin 400 mg daily, levofloxacin 750 mg daily)
For hospitalized patients, therapy consists of the following [8] :
-
Beta-lactam (ampicillin/sulbactam 1.5-3 g every 6 hours OR ceftriaxone 1-2 g daily or cefotaxime 1-2 g every 8 hours or ceftaroline 600 mg every 12 hours) AND a macrolide or
-
Respiratory fluoroquinolone or
-
If macrolides and fluoroquinolones are contraindicated: beta-lactam as above AND doxycycline
Therapy in ICU patients includes the following:
-
Beta-lactam (ampicillin/sulbactam 1.5-3 g every 6 hours OR ceftriaxone 1-2 g daily or cefotaxime 1-2 g every 8 hours OR ceftaroline 600 mg every 12 hours) AND a macrolide OR respiratory fluoroquinolone
For patients with severe beta-lactam allergy, aztreonam may be substituted for a beta-lactam. It is worth noting that many reported penicillin allergies are not true allergies. Owing to the limited spectrum of aztreonam and the relatively low likelihood of penicillin allergy cross-reacting with cephalosporins (2%), ceftriaxone or cefotaxime may be a reasonable choice after considering the balance of benefit and risk. [18]
If MRSA is suspected, therapy includes:
-
Vancomycin 15 mg/kg every 12 hours, adjusted based on levels, OR
-
Linezolid 600 mg every 12 hours.
If Pseudomonas is suspected, therapy includes:
-
Anti-pneumococcal and anti-pseudomonal beta-lactam (piperacillin/tazobactam 4.5 g every 6 hours, cefepime 2 g every 8 hours, ceftazidime 2 g every 8 hours, meropenem 1 g every 8 hours, OR imipenem 500 mg every 6 hours), OR aztreonam 2 g every 8 hours. [8]
Although the IDSA guidelines for CAP include ceftaroline as part of empiric beta-lactam therapy for inpatients, it often is reserved for patients who have risk factors for MRSA as it also is active against MRSA.
During influenza season, prompt empiric antiviral treatment is also advised for any patients presenting with flu-like symptoms and pneumonia. However, oseltamivir is preferred for inpatients due to limited data on alternative antivirals in severe cases. [19]
Rapid initiation of therapy is crucial for improving outcomes in CAP, but hastening treatment can lead to increased inappropriate antibiotic use and Clostridioides difficile colitis. In severe CAP or sepsis, antibiotics should be administered within the first hour of hypotension onset to reduce mortality. [20] Blood and ideally sputum cultures should be collected before the first antibiotic dose, but treatment should not be delayed. Studies suggest that a strict universal timing for the first antibiotic dose may lead to excessive antibiotic use. Clinical indicators of severe disease, such as advanced age, significant comorbidities, or need for supplemental oxygen, should guide the need for rapid antibiotic administration. [21]
Monitoring results from respiratory specimen cultures, blood cultures, pleural fluid analysis, PCR of respiratory samples, or antigen tests is essential to target therapy effectively. Inpatient CAP therapy typically involves intravenous antibiotics with a transition to oral therapy. [22, 23, 24, 25] Severely ill patients or those unable to tolerate or absorb oral medications may need extended parenteral therapy before switching to oral antibiotics. [26]
Mildly to moderately ill patients with CAP can be treated entirely with oral antibiotics, either as inpatients or outpatients. The standard duration for uncomplicated CAP therapy is 5 days. [20, 27] For CAP due to suspected or proven Pseudomonas or MRSA, the typical therapy duration is 7 days, with cessation after the patient has been afebrile for 48 to 72 hours and shows no signs of instability. Therapy duration may need extension if initial empiric therapy is ineffective against the identified pathogen or if the pneumonia is complicated by extrapulmonary infection. [8] Immunocompromised patients with CAP are treated similarly to otherwise healthy hosts but may require a longer therapy duration and additional investigations into pathogens. [8]
Overview
Community-acquired pneumonia (CAP) is one of the most common infectious diseases addressed by clinicians and is an important cause of mortality and morbidity worldwide.
Typical bacterial pathogens that cause CAP include S pneumoniae, H influenzae, and M catarrhalis. [1, 8] Numerous other organisms can cause CAP in the appropriate clinical setting. Furthermore, the so-called “atypical CAP” pathogens actually are common causes of CAP and originally were classified as atypical because they are not readily detectable on Gram stain or cultivatable on standard bacteriologic media.
CAP usually is acquired via inhalation or aspiration of a pathogenic organism. Aspiration pneumonia is commonly polymicrobial.
Severe community-acquired pneumonia
Severe CAP frequently develops in individuals with comorbid factors such as underlying cardiopulmonary disease, diminished splenic function, and/or heightened pathogenic virulence. Even in young and/or healthy hosts, severe CAP can develop if the causative pathogen is sufficiently virulent. For example, influenza, severe acute respiratory syndrome (SARS), Coronavirus disease 2019 (COVID-19), Hantavirus pulmonary syndrome (HPS), and Legionnaires’ disease may present as severe CAP. [28]
Patients with severe CAP should have the benefit of an infectious disease specialist to assist in identifying and optimally managing the underlying cause.
Complications associated with community-acquired pneumonia
The risk for complications in CAP depends on the infecting pathogen and the patient’s baseline health. For example, various organisms can cause empyema, including S pneumoniae, K pneumoniae (classically occurring in patients with chronic alcoholism), group A Streptococcus, and S aureus. Cavitation is not a typical feature of pneumococcal pneumonia but is relatively common in K pneumoniae infections.
Cardiovascular complications, including acute myocardial infarction or congestive heart failure (CHF), may be precipitated by CAP in up to one third of patients. [29, 30, 31] Development of an acute cardiovascular event is associated with increased mortality, longer hospital length of stay, and increased re-hospitalization rate. [32] Viral pneumonia such as COVID-19 also has been associated with increased rates of myocarditis. [33]
Patients with CAP who have impaired splenic function may develop overwhelming pneumococcal sepsis, potentially leading to death within 12 to 24 hours, regardless of the antimicrobial regimen used.
Morbidity and mortality
Morbidity and mortality associated with CAP are most common in elderly patients and immunocompromised hosts.
Other factors that may portend an increased risk for morbidity and mortality in individuals with CAP include significant comorbidities such as structural lung disease or cancer, and presenting signs of severe infection such as an increased respiratory rate, hypotension, fever, multilobar involvement, anemia, and hypoxia. [34] An elevated procalcitonin level may be associated with an increased mortality risk, although the specific threshold for increased risk remains to be determined. [14]
For more information, see the following:
Etiology of Community-Acquired Pneumonia
The definitive microbiologic etiology is determined in less than half of patients who develop community-acquired pneumonia (CAP); the exact rate depends on the patient population and diagnostic testing used. [1, 35, 36] Organisms traditionally have been classified as “typical” or “atypical” CAP pathogens, depending on their ability to be detected on Gram stain or standard bacterial cultures.
Typical community-acquired pneumonia pathogens
Typical bacterial pathogens that cause CAP include S pneumoniae, H influenza, and M catarrhalis. [28] The frequency with which CAP is attributable to one of these pathogens varies according to epidemiologic factors (eg, seasonality, patient demographics, exposure history) and the diagnostic testing used. In the past, these organisms had been reported to account for most CAP cases. [37] However, with improvement in diagnostic techniques allowing for better identification of viruses and fastidious bacteria, a smaller percentage of CAP cases are now being attributed to these typical bacterial pathogens. [38] In addition, the possibility of polymicrobial infections has received increased awareness; in recent epidemiologic studies, two pathogens, typically a virus and bacteria combination, were identified in over 30% of cases. [1, 35]
S pneumoniae remains the most common bacterial agent responsible for CAP. The incidence of S pneumoniae pneumonia varies according to the population studied. A 2015 study of 267 patients with CAP in Norway reported that S pneumoniae accounted for 30% of cases; this represented 48.5% of the cases in which an organism was identified. [35] A separate study of adults with CAP in the United States identified S pneumoniae as the etiologic agent in only 5% of total cases of CAP (13.5% of cases with an identified pathogen). [39] Declining tobacco smoking and widespread pneumococcal vaccination have been postulated as potential contributors to the decreased rates of S pneumoniae infection in the United States. [36, 38]
S aureus traditionally has not been considered a typical cause of CAP in otherwise healthy hosts, with the exception of potentially severe CAP after influenza infection. [4] Community-acquired methicillin-resistant S aureus (MRSA) has been associated with multilobar necrotizing CAP, including in previously healthy individuals. However, in a prospective multicenter US surveillance study of 2259 adults hospitalized for CAP, S aureus was identified in only 1.6% of patients, and MRSA accounted for only 0.7% of all cases. [40] Interestingly, in that study, the clinical presentation of MRSA CAP did not differ from that of all-cause non–S aureus or pneumococcal CAP with regard to concurrent influenza infection, presence of multilobar infiltrates, or hemoptysis. MRSA CAP was significantly associated with prior long-term hemodialysis use and carried a higher inpatient mortality rate (13.3%) than all-cause non–S aureus CAP (2%). [40]
Importantly, K pneumoniae and Pseudomonas aeruginosa are not typical causes of CAP in otherwise healthy hosts. K pneumoniae CAP occurs primarily in individuals with chronic alcoholism or diabetes mellitus. P aeruginosa is a cause of CAP in patients with underlying lung disease such as bronchiectasis or cystic fibrosis.
In certain patients admitted to the ICU, the microbial etiology of pneumonia may be complex. In a study by Cilloniz et al, 11% of cases were polymicrobial. The most frequently identified pathogens in polymicrobial infections were S pneumoniae, respiratory viruses, and P aeruginosa. Chronic respiratory disease and acute respiratory distress syndrome (ARDS) criteria were independent predictors of a polymicrobial infection. [41] Bacterial and viral co-infection may portend a worse prognosis. [42, 43]
Other gram-negative pathogens (eg, Enterobacter species, Serratia species, Stenotrophomonas maltophilia, Burkholderia cepacia) rarely cause CAP in patients without underlying lung disease or immunosuppression.
Atypical community-acquired pneumonia pathogens
Atypical bacterial pneumonias can be differentiated into those caused by zoonotic or nonzoonotic atypical pathogens.
Zoonotic atypical CAP pathogens include Chlamydiapsittaci (psittacosis), F tularensis (tularemia), and Coxiella burnetii (Q fever).
Nonzoonotic atypical CAP pathogens include Legionella species (Legionnaires’ disease), M pneumoniae, and C pneumoniae. [44]
Respiratory viruses are another important cause of atypical CAP. Whereas certain viruses may be zoonotically transmitted (eg, Hantavirus and avian influenza), most are transmitted from person to person.
Epidemiology of Community-Acquired Pneumonia
The incidence of CAP varies greatly from country to country. In the United States, CAP is estimated to occur in 649 of 100,000 adults annually, whereas a study from the Veterans Health Administration noted 472.2 cases per 100,000 person-years in 2017. [45, 46] Other countries report different frequencies, such as 8.1 per 10,000 in Vietnam and 31.2 per 10,000 in the United Kingdom. Rates also vary based on the population studied. In adults older than 65 years, 130.5 per 10,000 develop CAP in Malaysia, whereas 76.5 per 10,000 develop CAP in Germany. In individuals aged 85 years or older in Norway, the incidence of CAP is 172.4 per 10,000. [6]
Influenza and pneumonia combined remain in the top 10 leading causes of death in the United States, ranking 9 of 10 in 2020. The combination was responsible for 1.6% (53,495) of deaths in 2020, an absolute increase of 7.5% from 2019 but a relative decrease due to the separately accounted deaths due to COVID-19, which ranked 3 of 10 at 10.3% (345,323) of all deaths. [47] In addition, survivors of CAP have an increased incidence of cardiovascular events and mortality risk for months to years after CAP. As many as 20% of CAP survivors have been shown to have cardiovascular events, and mortality is up to 30% 2 to 5 years after CAP. [6]
The cost of CAP has been examined in numerous studies. In a 2018 retrospective analysis of claims data for adults aged 65 years or older in a Medicare insurance plan, the rate of CAP was 846.7 per 100,000 person-years, which was greater than rates for myocardial infarction (405), stroke (278.9), and osteoporotic fractures (343.9). This study noted vaccinations against influenza and Pneumococcus infection cost $40 million; however, prevention for stroke and myocardial infarction cost more than $661 million. [48]
Age
Advanced age is associated not only with a higher incidence of CAP but also with more severe disease, greater need for hospitalization, and higher mortality. [27, 49] A recent US study estimated 967,470 adults aged 65 and over are hospitalized annually from CAP with a 38% one-year mortality. [50]
CAP encountered in the ambulatory setting is more common among young adults, and is usually due to so-called atypical CAP pathogens (eg, Mycoplasma pneumoniae). [51]
Extrapulmonary Findings in Atypical Community-Acquired Pneumonia
Atypical community-acquired pneumonia (CAP) has classically been associated with more extrapulmonary manifestations than typical bacterial CAP. However, there can be considerable overlap in the clinical presentation of CAP due to various pathogens such that a definitive microbiologic diagnosis cannot be made based on signs and symptoms alone. Certain constellations of findings in the setting of appropriate historical clues may suggest an increased likelihood of a specific pathogen, thus warranting a targeted investigation for that organism. A detailed review of all potential extrapulmonary findings in CAP is beyond the scope of this article; however, some classic associations are included below:
M pneumoniae CAP is associated with the following findings [52] :
-
Headache, fever, malaise, sore throat in young adult with insidious onset of cough
-
Erythema multiforme major (Stevens-Johnson syndrome)
-
Cardiac conduction abnormalities
-
Hemolytic anemia and cold-agglutinin syndrome
-
Neurologic abnormalities, including aseptic meningitis or meningoencephalitis, Guillain-Barre syndrome, transverse myelitis
-
Epidemic outbreaks, such as schools or military barracks
Legionella pneumophila CAP (Legionnaires' disease) is associated with the following findings [53] :
-
Gastrointestinal and neurologic symptoms in the setting of pneumonia
-
Positive history of water or travel exposure
-
Relative bradycardia during febrile episode
-
Hyponatremia, hypophosphatemia, elevated creatine phosphokinase (CPK) level, elevated ferritin level, myoglobinuria
-
Leukocytosis with relative lymphopenia
-
Unresponsive to beta-lactam antibiotics
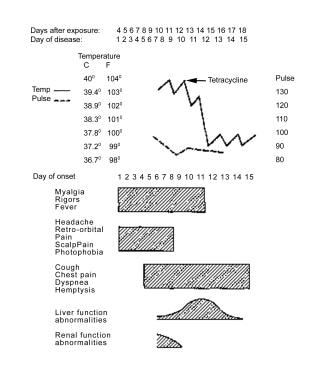 A case of Legionnaires disease from the Philadelphia outbreak, showing characteristics of relative bradycardia and extrapulmonary involvement.
A case of Legionnaires disease from the Philadelphia outbreak, showing characteristics of relative bradycardia and extrapulmonary involvement.
C burnetii CAP (Q fever) is associated with the following factors [54, 55] :
-
Acute infection
-
Severe retrobulbar headache, myalgias, fever, rigors, nonproductive cough
-
Elevated levels of transaminases and thrombocytopenia
-
Maculopapular or purpuric rash
-
Zoonotic exposure (goats, sheep, cattle most common)
Community-acquired pneumonia and shock
With the exception of CAP due to particularly virulent organisms (eg, S aureus, Hantavirus, severe acute respiratory syndrome [SARS-CoV-1 and 2], Legionella), CAP does not typically present with shock in otherwise healthy hosts. Therefore, in addition to considering the possibility of CAP due to a hypervirulent pathogen, patients who present with fever, dyspnea, leukocytosis, pulmonary infiltrates, and shock in the absence of conditions associated with hyposplenism should be evaluated for imitators of pneumonia, such as acute myocardial infarction or acute pulmonary embolism.
Conditions that predispose to severe CAP should be considered in patients presenting with CAP and shock in the absence of one of the aforementioned cardiopulmonary diseases. The following disorders and therapies have been associated with severe CAP:
-
Hyposplenism, splenectomy, or congenital asplenia
-
Corticosteroid therapy
-
HIV/AIDS
-
Chronic alcoholism
-
Amyloidosis
-
Chronic active hepatitis
-
Other causes of immunocompromise: Immunoglobulin A (IgA) deficiency, intestinal lymphangiectasia, myeloproliferative disorders, Waldenström macroglobulinemia, systemic mastocytosis
-
Illnesses requiring immunosuppression: Celiac disease, rheumatoid arthritis, systemic lupus erythematosus (SLE), vasculitis, non-Hodgkin lymphoma
Patient History
Patients with community-acquired pneumonia (CAP) due to typical bacterial CAP pathogens commonly present with fever, dyspnea, productive cough, and/or pleuritic chest pain.
The clinical presentation of atypical CAP is more subacute and associated with extrapulmonary manifestations that may provide a clue to the etiology.
Zoonotic infection
Contact with the appropriate zoonotic vector or its by-product (eg, milk, urine, feces, placenta) is needed to develop a zoonotic CAP. A history of occupational exposure to livestock (eg, farmers, veterinarians) or close contact with a parturient animal should be sought in patients with suspected Q fever. Psittacosis is preceded by recent contact with birds infected with C psittaci. Occupations and avocations associated with increased risk include poultry farming, pet shops, veterinary clinics, and ownership of pet birds (classically of the psittacine, or parrot, family). Hantavirus is transmitted via exposure to wild rodents, specifically to aerosolized rodent urine or feces; thus, queries as to whether a patient presenting with severe CAP works or recreates in a setting conducive to rodent exposure (eg, farms, ranches, forests) is warranted.
Physical Examination
Purulent sputum is characteristic of pneumonia caused by typical bacterial community-acquired pneumonia (CAP) pathogens and is not usually a feature of pneumonia caused by atypical pathogens, with the exception of Legionnaires’ disease. Blood-tinged sputum may be found in patients with pneumococcal pneumonia, Klebsiella pneumonia, or Legionella pneumonia.
Rales are heard over the involved lobe or segment. Consolidation may be accompanied by an increase in tactile fremitus, bronchial breath sounds, and egophony.
Legionella pneumonia, Q fever, and psittacosis are atypical pneumonias that may present with signs of consolidation. Consolidation is not a typical feature of pneumonia caused by M pneumoniae or C pneumoniae. [44]
Pleural effusion
Pleural effusion, if large enough, may be detectable on physical examination. Patients with a pleural effusion have decreased tactile fremitus, decreased breath sounds on auscultation, and dullness on chest percussion.
Empyema
On physical examination, empyema has the same findings as pleural effusion. Thoracentesis with analysis of pleural fluid for pH, cell counts, and Light's criteria are helpful when differentiating simple pleural effusions, parapneumonic effusions, or empyemas. PCR, in addition to traditional culture methods, may be helpful to determine the bacterial pathogen, if necessary. [56]
Differential Diagnoses of Community-Acquired Pneumonia
Aside from those mentioned above, the differential diagnoses to consider in the diagnosis of community-acquired pneumonia (CAP) include the following:
-
Acute exacerbation of chronic bronchitis
-
Tracheobronchitis
-
CHF and pulmonary edema
-
Pulmonary fibrosis
-
SLE pneumonitis
-
Drug hypersensitivity reactions (nitrofurantoin, daptomycin)
-
Drug-induced pulmonary disease (bleomycin, checkpoint inhibitors)
-
Cryptogenic organizing pneumonia
-
Bronchogenic carcinomas
-
Radiation pneumonitis
-
Granulomatosis with polyangiitis (Wegener granulomatosis)
-
Lymphoma
Sputum Studies and Blood Culture
Sputum culture is recommended in patients with severe disease and in all inpatients empirically treated for MRSA or Pseudomonas aeruginosa. [8]
Blood culture is recommended in patients with severe disease and in all inpatients empirically treated for MRSA or P aeruginosa. [8]
Studies in HIV-Positive Patients with Community-Acquired Pneumonia
The differential diagnosis of community-acquired pneumonia (CAP) in patients with human immunodeficiency virus (HIV) infection is broader than in HIV-negative patients. The patient’s immunologic status, as reflected by the CD4 count, the clinical course, and the chest radiographic appearance, provides clues to the most likely etiologic organism.
Patients with HIV infection and a normal or slightly decreased CD4 count with focal infiltrates have approximately the same pathogen distribution as otherwise healthy hosts (eg, S pneumoniae is most common) and thus warrant the same diagnostic strategies as the general population.
Pneumocystis jiroveci pneumonia (PJP) should be suspected in patients with a CD4 count of less than 200 cells/µL (or CD4% < 14%) presenting with gradually progressive dyspnea, nonfocal infiltrates on chest radiography, nonproductive cough, and hypoxemia. However, patients with a CD4 count of 100 or higher with an undetectable HIV viral load for the preceding 3-6 months are considered lower risk for PJP.
A definitive diagnosis of PJP requires visualization of the PJP cysts (ie, using special stains such as Giemsa or methenamine silver). Bronchoscopy with bronchoalveolar lavage (BAL) often is necessary to obtain an adequate specimen. The utility of other diagnostics such as serum 1,3 B-D glucan or Pneumocystis PCR of the BAL remains under study. Current limitations include the lack of reliable thresholds for 1,3 B-D glucan testing for the diagnosis of Pneumocystis as well as cost and unclear significance of lower quantitative values with PCR. [57, 58]
Patients with HIV infection who are admitted with CAP and suspicion for pulmonary tuberculosis (TB) should be placed on airborne isolation pending confirmation of the diagnosis, factoring in local incidence and exposure risk. HIV is associated with an increased likelihood of extrapulmonary disease, atypical imaging findings, and smear negative disease. Several of these differences correlate with worsening CD4 counts [59, 60]
Additional uncommon CAP pathogens, such as histoplasmosis, coccidioidomycosis, and cryptococcosis, should be considered in HIV-positive patients who present with pulmonary infiltrates, with risk stratified according to potential exposure history. Antigen testing (urine antigen for histoplasmosis; serum antigen for cryptococcosis) may be helpful in these cases.
Other Laboratory Tests for Community-Acquired Pneumonia
Several nonspecific laboratory tests often are performed during the workup of community-acquired pneumonia (CAP), particularly if atypical CAP is suspected.
Serum transaminase, serum sodium, serum ferritin, serum phosphorus, and creatine phosphokinase (CPK) levels may provide evidence supporting a particular pathogen, such as Legionella. Lactic acid, white blood cell (WBC) count, blood urea nitrogen, and creatinine may be used in categorizing the severity of illness.
Cold agglutinin titers of 1:32 or greater may support a diagnosis of M pneumoniae, although this test is neither sensitive nor specific and has largely been replaced by newer diagnostic studies, such as respiratory pathogen PCR assay.
Procalcitonin and C-reactive protein levels
C-reactive protein (CRP) and procalcitonin (PCT) are inflammatory biomarkers occasionally utilized in the diagnosis and management of pneumonia. CRP, a nonspecific acute-phase reactant, is inexpensive and widely available but has limited specificity for differentiating inflammation causes. In contrast, PCT, a calcitonin precursor peptide, is released in response to bacterial infections and is regulated by cytokines such as interleukin-1beta, tumor necrosis factor alpha, and interleukin 6, with down-regulation by interferon gamma during viral infections. [13]
PCT is of particular interest in distinguishing bacterial from non-bacterial infections, assessing the severity and prognosis of community-acquired pneumonia (CAP), and guiding the duration of antibiotic therapy, although data supporting its use has been conflicting. PCT levels, alone or combined with CRP, have been linked to mortality prediction in CAP, [15] with timing from symptom onset influencing biomarker levels at diagnosis. [61] Some studies suggest PCT-guided protocols could reduce mortality, antibiotic exposure, and adverse effects in acute respiratory infections, although no significant difference in treatment failure rates has been observed. [62] However, a recent meta-analysis identified PCT sensitivity and specificity for distinguishing bacterial pneumonia from viral pneumonia as just 0.55 and 0.76, respectively {132}. Further study will need to determine its utility in identifying bacterial CAP, timing of de-escalation of antibiotics, as well as optimal cut-off values for interpretation. The 2016 and 2019 IDSA/ATS guidelines recommend cautious use of PCT and CRP in antibiotic decision-making for HAP/VAP and CAP due to variability in test sensitivity and the lack of consistent positive thresholds. [8, 63]
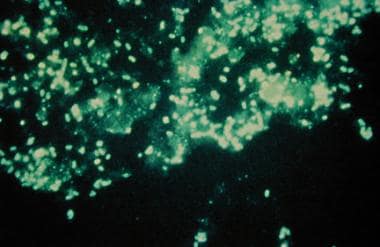
Direct fluorescent antibody testing
Direct fluorescent antibody (DFA) testing of the sputum can be performed to try to assist with the diagnosis of atypical CAP pathogens, including Legionella, P jiroveci, and Chlamydophila; however, the utility of this test is hampered by suboptimal sensitivity and is relatively difficult to perform. A DFA stain showing Legionella infection is seen in the image below.
Serology
Serology has been replaced by more rapid PCR-based assays in many settings; serology was historically useful in identifying fastidious organisms, particularly when dealing with pathogens that have potential epidemiologic implications (ie, epidemic or biohazard situations), such as B pertussis, M pneumoniae, L pneumophila, or C burnetii. Serologic diagnosis is based on a 4-fold or greater increase in titers between acute- and convalescent-phase serum specimens so is generally not useful in the acute-care setting. A significantly elevated IgM titer (typically present in the acute phase of infection) may help support a diagnosis, and some experts have suggested that combining IgM and nucleic acid amplification testing may be the optimal method for diagnosing M pneumoniae infection. [64]
Urinary antigen test
Pneumococcal urinary antigen testing (UAT) is a non–culture-based test for diagnosing pneumococcal infection that has a reported sensitivity of 50% to 80% and specificity of more than 90%. [65] Thus, a negative result does not rule out pneumococcal pneumonia. The UAT results remain positive after antibiotics have been started so may be particularly useful when cultures were not obtained prior to initiation of antibiotic therapy. Recent IDSA guidelines recommend use of pneumococcal urinary antigen testing in adults with severe CAP only. [8]
In 2018, Wunderink et al reported that serotype-specific urinary antigen detection assays may further improve detection of pneumococcal pneumonia in hospitalized adults with CAP. [66] Availability of pneumococcal UAT is the main perceived barrier to its routine use. [65]
Urinary antigen testing is considered the first-line diagnostic test for L pneumophila. The sensitivity of the test ranges from 55% to 99%, with improved sensitivity paralleling disease severity. [53] The specificity is high (95%). The urinary antigen test is applicable only for L pneumophila serogroup type I, which accounts for approximately 85% of Legionella infections in the United States and Europe. In other regions of the world, including Australasia and East Asia, a rising number of cases have been attributed to another species, Legionella longbeachae. [67] It has overtaken Legionella pneumophila to be the predominant cause of Legionellosis in New Zealand, though this may be attributable to transition to molecular diagnostics over time. [68] The UAT results remain positive for Legionella for long periods, but may be negative within the first 48 hours of infection. Using a combination of Legionella UAT and PCR of respiratory secretions, which is often able to detect all species of Legionella, may increase the ability to diagnose Legionella pneumonia. [69] The 2019 IDSA/ATS CAP guidelines recommend obtaining a urine Legionella antigen test in patients with severe CAP and when epidemiologic factors support a potential Legionella diagnosis. [8]
Polymerase chain reaction
Polymerase chain reaction (PCR) has emerged as an important diagnostic tool for determining the etiology of CAP, particularly with regard to respiratory viruses and fastidious organisms, including Legionella, Mycoplasma, and Chlamydophila. [70] PCR is a very sensitive and specific method for isolating these pathogens.
The source of specimen may affect the diagnostic yield of PCR assays; for instance, the detection rate of many pathogens, including Legionella and M pneumoniae, is higher with sputum samples than with nasopharyngeal aspirates. [69] However, nasopharyngeal samples remain useful, as many patients are unable to provide a quality sputum sample. Interpreting the significance of PCR detection of an organism known to colonize the upper airway or those that may be associated with protracted shedding, such as rhinovirus, remains a challenge. Quantitative PCR methods have shown some promise in improving interpretability of such findings. [71] Alternatively, the IDSA Diagnostics Committee cautions against the use of a negative upper respiratory tract sample to rule out infection, as some viruses shed for longer periods of time into the lower respiratory tract. [72]
The increasing commercial availability of various PCR assays (including multiplex) has allowed for increased implementation in the clinical setting. Multipathogen approaches are less time consuming than testing each organism individually, although they may be complex to perform. Rapid molecular tests for respiratory viruses are also increasingly being developed with the goal of further shortening the time to diagnosis. [73] PCT has also been used in conjunction with a lower respiratory multiplex PCR panel to distinguish bacterial infection from colonizers. [74]
A comparison of lower respiratory tract multiplex PCR and routine culture was performed in UK inpatients, which demonstrated markedly improved identification of a pathogen with multiplex PCR compared to culture (87% vs 39%). Preceding use of antibiotics did not significantly affect detection rate in the PCR group. [75]
The 2020 IDSA guidelines on molecular testing for respiratory tract infections suggest that lower respiratory tract bacterial NAAT may be most beneficial in patients with intermediate pretest probability and disease severity, as results would be more likely to influence targeting antibiotics appropriately in the case of a positive test versus avoidance of unnecessary empiric antibiotics with a negative test. However, more extensive study is needed on the topic, including benefits of quantitative results to potentially distinguish between colonization and true infection, as well as cost-effectiveness of testing. [72] Alternatively, the 2021 ATS guidelines on non-influenza viral NAAT in patients with CAP advise performing viral multiplex testing only in patients with severe CAP or who are immunocompromised. This is attributed to limited evidence that a test result, whether positive or negative, impacts subsequent antibiotic therapy outside of these high-risk populations. [76]
Chest Imaging
Chest radiography
Chest radiographs are essential for all patients with suspected community-acquired pneumonia (CAP) to confirm the presence of infiltrates consistent with CAP and to exclude conditions that mimic it. [9, 10]
 Chest radiograph in a patient with HIV infection, bilateral perihilar infiltrates, and Pneumocystis jiroveci pneumonia.
Chest radiograph in a patient with HIV infection, bilateral perihilar infiltrates, and Pneumocystis jiroveci pneumonia.
Chest radiography helps differentiate viral from nonviral pneumonias. Viral pneumonias often show few or no infiltrates, but when present, infiltrates typically are bilateral, perihilar, symmetric, and interstitial, which can be confused with pulmonary edema. In contrast, bacterial pneumonias usually exhibit a focal segmental or lobar distribution, occasionally accompanied by pleural effusions. Atypical bacterial pathogens display variable radiographic findings, from focal segmental to bilateral interstitial patterns. Pneumocystis jiroveci pneumonia (PJP) characteristically presents as bilateral patchy interstitial infiltrates. However, radiographic findings alone cannot reliably distinguish the specific etiologies of CAP.
Patients with asthma or chronic bronchitis exacerbations without CAP should have negative chest radiographic findings. In congestive heart failure (CHF), infiltrates appear as increased interstitial markings with vascular redistribution to the upper lobes, and preexisting heart failure often includes cardiomegaly. Rapid cavitation is not typical of CAP but is a hallmark of methicillin-resistant S. aureus (CA-MRSA) CAP, which presents as fulminant CAP with rapid cavitation and necrotizing pneumonia, sometimes following influenza or occurring independently in healthy individuals.
Serial chest radiography is useful for monitoring the progression of severe CAP if there is no improvement within 5 to 7 days. [8] Radiographic findings in severe typical bacterial CAP worsen rapidly and take a significant time to improve, with clinical resolution preceding radiologic resolution.
Routine follow-up chest imaging generally is not recommended; however, lung cancer screening should be considered when clinically indicated. [8]
Recognition of diverse chest radiographic patterns in CAP, such as subtle bronchopneumonia, interstitial patterns, and round pneumonia, is crucial for diagnosis, though these patterns do not specify infectious agents. [77] The presence of pleural fluid and multilobar opacities, which can influence treatment decisions, should be documented. Follow-up radiographs should be considered based on clinical presentation, especially in cases with discordant clinical and radiographic findings. Signs such as lymphadenopathy and multiple pulmonary nodules should prompt consideration of alternative diagnoses, and tuberculosis should be suspected in patients presenting with atypical, subacute symptoms, particularly when radiographic findings include cavitation or upper lobe opacities.
However, limitations of chest radiography include low sensitivity and positive predictive value and moderate inter-observer variability. [78, 79]
See Bacterial Pneumonia and Fungal Pneumonia for additional detail.
CT scanning
Research has consistently demonstrated the improved sensitivity and specificity of chest computed tomography (CT) over CXR. [78, 79] The feasibility of low-dose chest CT for routine CAP diagnosis is being explored, potentially improving CAP rule out and reducing unnecessary antibiotic use. [80]
A review was performed of a subset of patients within the prospective, multicenter ESCAPED study to identify CAP CT-patterns, correlation with microbiologic data, and characteristics associated with CXR false negatives. The most commonly identified pattern was lobar pneumonia, which was also more commonly associated with Streptococcus pneumoniae and Mycoplasma pneumoniae. A lobar pneumonia pattern was also the least likely to have been missed on CXR. Respiratory viruses were uniformly distributed across all patterns, though the study preceded the COVID-19 pandemic. [78]
Obtain a computed tomography (CT) scan of the chest if pneumonia is clinically suspected despite persistently negative chest radiographic findings to examine for viral, atypical, or mycobacterial pneumonia, particularly in immunocompromised hosts with a broad differential diagnosis that would benefit from further narrowing. [78] When an underlying bronchogenic carcinoma is suspected or if any abnormalities are not consistent with the diagnosis of pneumonia, CT is helpful to examine for structural lung disease or malignancy.
Lung ultrasound
Research suggests that lung ultrasound may be a useful adjunct in diagnosis of pneumonia, with improved sensitivity and specificity over routine chest radiograph when using CT as the gold standard. [81, 82] Benefits include lack of radiation exposure and improved point of care accessibility, especially in the outpatient setting. A need for specific training limits its wide usage among outpatient providers, though it may be more applicable in an emergency department setting where many providers are already trained in bedside ultrasonography.
Fine-Needle Aspiration and Bronchoscopy With Bronchoalveolar Lavage
Quantitative cultures from bronchoscopic or suctioned specimens, collected before antibiotic administration, are instrumental in distinguishing between bacterial colonization—where microorganisms are present without causing symptoms or an inflammatory response—and actual infection. [1] Bronchoscopy, often with bronchoalveolar lavage (BAL), typically is reserved for patients on mechanical ventilation or those with risk factors such as immunocompromise or failure of empirical therapy, which may suggest unusual microorganisms or complicated pneumonia. It is particularly useful in diagnosing community-acquired pneumonia (CAP) when pathogens like Pneumocystis, mycobacteria, or fungi are suspected.
Additionally, transthoracic fine-needle aspiration (FNA) can be employed to ascertain the cause of pulmonary nodules or noninfectious infiltrates that do not respond to antibiotics, providing a diagnostic alternative when bronchoscopic approaches are not indicated or feasible. [1] This method is most effective for identifying the etiology of localized lung abnormalities.
Histologic Findings
The pathology of typical bacterial lobar pneumonias is initially characterized by congestion, with alveolar edema. This progresses to red hepatization, with a hemorrhagic alveolar exudate. With breakdown of the preceding RBCs, the next stage is grey hepatization, characterized by a fibrinopurulent exudate. The term hepatization is in reference to the firmness being similar to liver tissue. Resolution eventually occurs with clearance of preceding exudates and potential formation of scar tissue.
Viral lung infections may manifest as interstitial inflammation, diffuse alveolar damage, and/or necrotizing bronchitis/bronchiolitis. [83]
Pharmacologic Therapy
Most experts feel that antimicrobial coverage should be divided against typical and atypical CAP pathogens with consideration for risk of viral infection such as influenza, based on the season. [84]
A 2017 review presented a CAP bundle that is in line with international guidelines and IDSA/ATS guidelines. The 2019 updated IDSA/ATS guidelines also support these components. The bundle includes the following [6, 8] :
-
Use of PSI and clinical criteria to the determine CAP severity and appropriate level of care
-
Appropriate empiric antibiotics started promptly
-
Rapid fluid and electrolyte resuscitation, thromboembolic prophylaxis, and management of hypoxia
-
Early ambulation
-
Assessment of cardiovascular risk with appropriate initiation of aspirin or other prophylaxis
The ATS/IDSA CAP guidelines endorse the Surviving Sepsis Campaign recommendations on using corticosteroids in patients with CAP who have refractory septic shock. [8]
Anti-influenza therapy
Anti-influenza treatment (eg, oseltamivir) should be prescribed to all adults with CAP who test positive for influenza, regardless of hospitalization status.
Antibacterial therapy in patients with influenza
Standard antibacterial treatment should be initially prescribed to adults with clinical and radiographic evidence of CAP who test positive for influenza.
Treatment duration
The duration of antibiotic therapy should be guided by a validated measure of clinical stability. Antibiotics should be continued until stability is achieved, for a total antibiotic duration of at least 5 days.
Antibiotic selection
Adequate therapy for CAP includes coverage for S pneumoniae and atypical bacterial pathogens. Treatment options for CAP in outpatients with no comorbidities and no risk factors for drug-resistant S pneumoniae include the following [8] :
-
Amoxicillin 1 gram PO three times a day OR
-
A macrolide (azithromycin 500 mg on first day then 250 mg daily or azithromycin 500mg daily for three days, or clarithromycin 500 mg twice daily or clarithromycin extended release 1,000 mg daily) only in areas with pneumococcal resistance to macrolides < 25% OR
-
Doxycycline 100 mg twice daily
During influenza season, it is also reasonable to initiate oseltamivir, zanamivir, peramivir, or baloxavir therapy in outpatients who present with a flu-like illness and pneumonia.
Treatment options for CAP in outpatients with comorbidities such as chronic heart, lung, liver, or renal disease; diabetes mellitus; alcoholism; malignancy; asplenia; immunosuppression; prior antibiotics within 90 days; or other risk factors for drug-resistant infection include the following [8] :
-
Beta-lactam (amoxicillin/clavulanate 2 g/125 mg twice daily or 500 mg/125 mg three times daily or 875 mg/125 mg twice daily, cefpodoxime 200 mg twice daily, or cefuroxime 500 mg twice daily) AND a macrolide or doxycycline OR
-
Respiratory fluoroquinolone (moxifloxacin 400 mg daily or levofloxacin 750 mg daily)
For hospitalized patients, therapy consists of the following [8] :
-
Beta-lactam (ampicillin/sulbactam 1.5-3 g every 6 hours or ceftriaxone 1-2 g daily or cefotaxime 1-2 g every 8 hours or ceftaroline 600 mg every 12 hours) AND a macrolide OR
-
Respiratory fluoroquinolone OR
-
If macrolides and fluoroquinolones are contraindicated: beta-lactam as above AND doxycycline
Therapy in ICU patients includes the following:
-
Beta-lactam (ampicillin/sulbactam 1.5-3 g every 6 hours or ceftriaxone 1-2 g daily or cefotaxime 1-2 g every 8 hours or ceftaroline 600 mg every 12 hours) AND a macrolide or respiratory fluoroquinolone
For patients with severe beta-lactam allergy, aztreonam may be substituted for a beta-lactam. It is worth noting that many reported penicillin allergies are not true allergies. Owing to the limited spectrum of aztreonam and the relatively low likelihood of penicillin allergy cross-reacting with cephalosporins (2%), ceftriaxone or cefotaxime may be a reasonable choice after considering the balance of benefit and risk. [18]
Risk factors for methicillin-resistant S aureus (MRSA) and Pseudomonas pneumonia primarily include prior MRSA isolation, recent hospitalization or use of IV antibiotics. [8] IDSA/ATS guidelines otherwise advise collecting local data to identify prevalence and local risk factors for these pathogens given absence of high quality data.
If MRSA is suspected, therapy includes:
-
Vancomycin 15 mg/kg every 12 hours, adjusted based on levels, OR
-
Linezolid 600 mg every 12 hours.
If Pseudomonas is suspected, therapy includes:
-
Anti-pneumococcal and anti-pseudomonal beta-lactam (piperacillin/tazobactam 4.5 g every 6 hours, cefepime 2 g every 8 hours, ceftazidime 2 g every 8 hours, meropenem 1 g every 8 hours, or imipenem 500 mg every 6 hours), or aztreonam 2 g every 8 hours. [8]
While the IDSA guidelines for CAP include ceftaroline as part of empiric beta-lactam therapy for inpatients, as it is also active against MRSA it is often reserved for patients who have risk factors for MRSA.
During influenza season, it is also reasonable to start oseltamivir, zanamivir, peramivir, or baloxavir therapy to treat influenza in patients with MRSA CAP, as well as in patients who present with a flulike illness and pneumonia, as influenza may have preceded the MRSA infection. However, oseltamivir remains the preferred agent in inpatients with suspected or confirmed influenza, as there is limited data to support the alternative antivirals in severe or complicated disease. [19]
Other antibiotics approved by the FDA for CAP
Omadacycline is a tetracycline designed to overcome tetracycline resistance, and it was shown to be noninferior to moxifloxacin. [85, 86]
Lefamulin, a pleuromutilin antibiotic, was found to be noninferior to moxifloxacin in a 2019 phase 3 trial. [87] Lefamulin is indicated for the treatment of bacterial CAP due to S pneumoniae, S aureus (methicillin-susceptible isolates), H influenzae, Legionella pneumophila, M pneumoniae, or C pneumoniae in adults. It is administered twice daily as either an intravenous infusion or an oral tablet.
Solithromycin, a new macrolide, was compared with moxifloxacin as an IV-to-PO option and was found to be noninferior. [88]
Delafloxacin, a novel fluoroquinolone, has the advantage of activity against both MRSA and Pseudomonas, and gained approval in October 2019 for the treatment of bacterial CAP in adults. Approval was based on a phase 3 randomized, double-blind study (n = 859) that compared delafloxacin with moxifloxacin. Results showed that IV-to-oral delafloxacin was noninferior at 96 hours compared with moxifloxacin. [89, 90]
Ceftobiprole medocaril sodium is an extended-spectrum cephalosporin with activity against clinically important gram-positive bacteria, including methicillin-resistant Staphylococcus aureus (MRSA). It is indicated for S aureus bacteremia (SAB) in adults, including right-sided infective endocarditis, caused by methicillin-susceptible and methicillin-resistant isolates.
Treatment Duration and other Pharmacologic Considerations
Mild to moderately ill patients with CAP may be treated entirely via the oral route, on either an inpatient or outpatient basis. Patients who are severely ill or unable to tolerate or absorb oral medications require some duration of intravenous therapy before switching to an oral antibiotic. [26]
If the patient is switched to an oral regimen and is doing well, earlier discharge with completion of antibiotics at home is possible. Optimal intravenous-to-oral switch therapy consists of a single agent that has an appropriate spectrum, has excellent bioavailability, is well tolerated, has a low resistance potential, and is relatively inexpensive.
The duration of therapy for uncomplicated CAP is usually 5 days. [20, 27] The duration of therapy for CAP due to suspected or proven Pseudomonas or MRSA is typically 7 days. Patients should be afebrile for 48 to 72 hours and have no signs of instability before antibiotic therapy is stopped. The duration of therapy may need to be increased if the initial empiric therapy has no activity against the specific pathogen or if the pneumonia is complicated by extrapulmonary infection. [27]
Due to limited data, the use of systemic corticosteroids in patients with CAP is not recommended routinely for any severity of CAP but is advised for managing certain comorbidities or as part of the sepsis bundle. [8] The Surviving Sepsis Campaign Guidelines Studies recommend hydrocortisone for those patients with septic shock being managed with vasopressors. [91] Studies have demonstrated that corticosteroids in CAP may decrease mortality and progression to mechanical ventilation of initiation of vasopressors. [92] However, the data remains conflicting and these potential benefits should be weighed against the risk of worsening influenza pneumonia, hyperglycemia, and secondary infections. [93] Furthermore, there is insufficient data or agreement on the dose or duration of the steroid therapy.
Appropriate spectrum
In otherwise healthy hosts with CAP, therapy does not need to cover methicillin-resistant S aureus, Klebsiella species, or P aeruginosa. Coverage should include typical (S pneumoniae, H influenzae, M catarrhalis) and atypical (Legionella and Mycoplasma species, C pneumoniae) pathogens.
A regimen including methicillin-susceptible S aureus (MSSA) coverage should be included in patients with influenza and signs of CAP, with need for MRSA coverage determined by risk. Risk factors for MRSA pneumonia include prior hospital admission of 2 or more days in the preceding 90 days, antibiotics in the preceding 90 days, residence in a long-term care facility, septic shock at the time of CAP, immunosuppression, enteral tube feedings, nonambulatory status, gastric acid suppression, chronic hemodialysis, congestive heart failure, and history of MRSA colonization. [63]
Most antibiotics used to treat community-acquired pneumonia are highly effective against oral anaerobes that are involved in aspiration pneumonia. The routine addition of anaerobic coverage (ie clindamycin or beta-lactam/beta-lactamase inhibitor) for suspected aspiration pneumonia is not recommended, except for lung abscess or empyema. For aerobic lung abscesses, clindamycin or a beta lactam/beta-lactamase inhibitor are preferable.
Penicillin resistance
The CDC routinely monitors rates of invasive antibiotic-resistant S pneumoniae. Predominant drugs with resistance as of latest 2023 data include erythromycin (24.4%), trimethoprim/sulfamethoxazole (19.9%), and tetracycline (10.2%). Penicillin resistance based on 2009 CLSI breakpoints is 2.7%. Most penicillin-resistant S pneumoniae infections may be treated with beta-lactams. [94] Alternately, doxycycline or respiratory quinolones may be used if susceptibility is demonstrated. High-level penicillin-resistant S pneumoniae (MIC 6 µg/mL) strains are a rare cause of CAP; fortunately, they remain susceptible to ceftriaxone.
Severity
The severity of CAP may be estimated with scoring systems. The Pneumonia Severity Index (PSI) is preferred over the CURB-65 (confusion, uremia, respiratory rate, low blood pressure, age >65 years) for determining outpatient verses inpatient treatment. Patients with PSI class IV-V may need hospitalization or more intensive in-home services. Severe pneumonia is defined as having 1 major criteria or 3 minor criteria as follows:
Major criteria:
-
Septic shock requiring vasopressors
-
Respiratory failure requiring mechanical ventilation
Minor criteria:
-
Respiratory rate of 30 or more breaths per minute
-
PaO2/FIO2 ratio of 250 or less
-
Multilobar infiltrates
-
Confusion
-
Uremia
-
Leukopenia (WBC < 4000 cells/µl)
-
Thrombocytopenia (platelet count < 100,000/µl)
-
Hypothermia
-
Hypotension
These are the primary criteria to use to determine if a patient requires ICU admission. CURB-65 was designed to predict mortality risk; CRB-65 is similar but is used when certain laboratory tests are unavailable. Some scoring systems (eg, CURXO and SMART-COP) focus on the severity of CAP and likelihood of requiring ventilatory or circulatory support, whereas the PSI helps determine whether CAP requires hospitalization.
Comorbid conditions
Comorbid conditions affect a patient’s risk of contracting CAP caused by MRSA, Pseudomonas, or other antibiotic-resistant pathogens. Risks for antibiotic-resistant pathogens include hospital admission within the preceding 90 days, antibiotics in the preceding 90 days, septic shock at the time of CAP, immunosuppression, enteral tube feedings, non-ambulatory status, or gastric acid suppression. MRSA risk factors include all of the prior plus hemodialysis, CHF, and a history of MRSA colonization. [6, 63]
There is conflicting evidence as to the safety of using PPIs and H2 blockers. [95, 96, 97, 98] Some studies have concluded that PPI use increases the risk for pneumonia or even the risk of multidrug-resistant pathogens causing pneumonia. Other, more recent, studies find such links may have resulted from confounding factors. [97, 99]
Negative prognostic factors in community-acquired pneumonia (CAP) include preexisting lung disease, underlying cardiac disease, poor splenic function, advanced age, multilobar involvement, past infection with tuberculosis, and delayed initiation of appropriate antimicrobial therapy. [100, 101]
Overall, comorbidities represent important prognostic factors and contribute to the severity index. [101]
Outpatient Care in Community-Acquired Pneumonia
Patients with mild community-acquired pneumonia (CAP) who are being treated on an outpatient basis should be monitored to ensure compliance with their medications and to ensure clinical improvement. After 1 week, a repeat visit is advisable. If the patient is improving and parapneumonic complications are not evident, posttherapy chest radiography is unnecessary. [102, 103, 104]
The diet in patients with CAP is as tolerated. Guide activity with common sense.
Vaccination
Pneumococcal vaccines have been shown to have some efficacy in preventing vaccine-strain pneumococcal pneumonia and invasive disease. They have not been shown to prevent community-acquired pneumonia (CAP) of all kinds. [105, 106] Annual influenza vaccination has been shown to decrease pneumonia diagnoses, hospitalizations, and cardiac events in certain populations. [107, 108, 109, 110]
Annual influenza vaccination is recommended in all persons older than 6 months. There are several options for vaccination, including standard-dose trivalent inactivated vaccine, high-dose inactivated trivalent vaccine, three different formulations of quadrivalent inactivated vaccine (egg-based, cell culture–based, and recombinant-derived), and a live attenuated influenza vaccine. Per current CDC recommendations, people with a history of egg allergy of any severity may receive any licensed, recommended, and age-appropriate influenza vaccine. [111] Individuals with a history of severe egg allergy should receive the vaccine under the supervision of a physician experienced in the management of allergic conditions. People with a personal history of severe allergy to the flu vaccine should not receive it, and persons with history of Guillain-Barré syndrome should consult with their physician prior to being vaccinated. [112]
Four pneumococcal vaccines are approved in the United States [113] :
-
15-valent conjugate vaccine (PCV15; Vaxneuvance) is approved for adults 18 years and older.
-
20-valent conjugate vaccine (PCV20; Prevnar 20) is approved for adults 18 years and older.
-
21-valent conjugate vaccine (PCV21; Capvaxive)
-
23-valent pneumococcal polysaccharide vaccine (PPSV23; Pneumovax 23) is approved for adults aged 65 years or older and persons aged 2 years or older who are at an increased risk for pneumococcal disease.
In October 2024, the Advisory Committee on Immunization Practices (ACIP) approved the Recommended Immunization Schedule for Adults Ages 19 Years or Older, United States, 2025. [113, 114] PCV21 now is listed as a vaccination option across all relevant sections of the notes. PCV21 includes 8 pneumococcal serotypes that are not present in PCV15, PCV20, or PPSV23. However, it lacks some serotypes, such as serotype 4, that are found in other pneumococcal vaccines.
For routine vaccination, universal vaccination now is recommended for adults aged ≥50 years. For “special situations,” a risk-based vaccination recommendation is provided for adults aged 19–49 years. New details have been added about the use of pneumococcal vaccines during pregnancy and guidance for situations where PPSV23 is not available. [113, 114]
The administration of pneumococcal vaccines is tailored based on an individual's age, vaccination history, and specific health conditions.
The Advisory Committee on Immunization Practices (ACIP) recommends the following [113, 114] :
Routine vaccination
-
Adults aged 50 years and older should receive a pneumococcal conjugate vaccine—either PCV15, PCV20, or PCV21. This recommendation applies to individuals who have not previously received any pneumococcal conjugate vaccine or whose vaccination history is unknown.
- For those administered PCV15, an additional dose of PPSV23 is required 1 year later to complete the pneumococcal vaccination series. This subsequent dose may be considered at a minimum interval of 8 weeks in specific clinical scenarios, such as patients with an immunocompromising condition, those with a cochlear implant, or individuals with a cerebrospinal fluid leak.
- If PCV20 or PCV21 is administered, no further vaccination with PPSV23 is indicated.
-
For adults aged 65 years or older, shared clinical decision-making is recommended regarding pneumococcal vaccination. These patients may choose to receive PCV20 or PCV21, or opt out of additional pneumococcal vaccines if they have previously received PCV13 (but not PCV15, PCV20, or PCV21) at any age and PPSV23 at or after the age of 65.
Adults under age 50 with a risk condition
-
The CDC defines a risk condition as presence of cerebrospinal fluid (CSF) leak, chronic liver disease, cochlear implant, an immunocompromising condition (congenital or acquired asplenia/splenic dysfunction, immunodeficiency, conditions associated with immunosuppressive drugs or radiation therapy, HIV infection, hemoglobinopathy), or diabetes mellitus.
-
Individuals who have never received a pneumococcal vaccine are administered 1 dose of either PCV15, PCV20, or PCV21. If PCV15 is selected, it should be followed by a dose of PPSV23 at least 1 year later, although this interval can be shortened to 8 weeks for adults with an immunocompromising condition, a cochlear implant, or a cerebrospinal fluid leak. Once this regimen is completed, the pneumococcal vaccination series is considered complete.
-
For those who receive PCV20 or PCV21, no subsequent dose of PPSV23 is required, and the vaccination series is complete upon administration of either vaccine.
-
Individuals who have previously received only PPSV23 should be given a dose of PCV15, PCV20, or PCV21 at least 1 year after their most recent PPSV23 vaccination. Following this, no additional dose of PPSV23 is recommended regardless of the vaccine used, completing their pneumococcal vaccination series.
-
Those who have only received PCV13 should receive a dose of PCV20 or PCV21 at least 1 year after their most recent PCV13 vaccination, which completes their pneumococcal vaccination series.
-
For patients who have received both PCV13 and 1 dose of PPSV23, the subsequent recommendations are contingent upon the individual's risk condition.
- Patients with high-risk conditions such as an immunocompromising condition, a cerebrospinal fluid leak, or a cochlear implant should receive a dose of PCV20 or PCV21 at least 5 years after their most recent pneumococcal vaccination. This completes their pneumococcal vaccination series.
- For those with other risk conditions, no additional pneumococcal vaccines are recommended until the individual reaches at least age 50 years, at which time it is advisable to reassess the pneumococcal vaccine recommendations to ensure continued protection against pneumococcal disease.
Guidelines
The following organizations have released guidelines for the management of community-acquired pneumonia. Key diagnostic and treatment recommendations have been reviewed and integrated throughout the article.
-
Infectious Diseases Society of America and the American Thoracic Society (2019): Updated guidelines for community-acquired pneumonia (2019). [8]
Patient Instructions
Remind patients with community-acquired pneumonia (CAP) to comply with prescribed antimicrobials even after they experience clinical improvement. Avoid dampening the cough reflex, and, except in patients with heart failure, encourage hydration to help facilitate clearance of secretions.
Acknowledgments
This article is the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the U.S. Government. The contents of this article do not represent the views of the Department of Veterans Affairs or the United States Government.
-
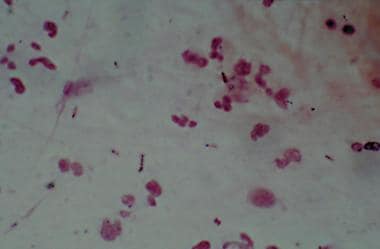
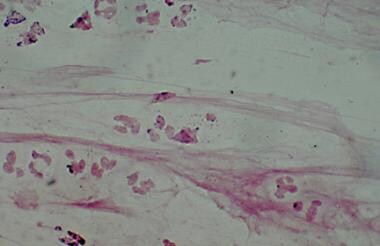
Gram stain showing Streptococcus pneumoniae.
-
Gram stain showing Haemophilus influenzae.
-
Gram stain showing Moraxella catarrhalis.
-
Clinical diagnostic approach in community-acquired pneumonias.
-
Sputum direct fluorescent antibody stain showing Legionella infection.
-
A case of Legionnaires disease from the Philadelphia outbreak, showing characteristics of relative bradycardia and extrapulmonary involvement.
-
Chest radiograph in a patient with HIV infection, bilateral perihilar infiltrates, and Pneumocystis jiroveci pneumonia.
-
Chest radiograph in a patient with HIV infection and focal infiltrates due to tuberculosis.
Tables
What would you like to print?
- Practice Essentials
- Overview
- Etiology of Community-Acquired Pneumonia
- Epidemiology of Community-Acquired Pneumonia
- Extrapulmonary Findings in Atypical Community-Acquired Pneumonia
- Patient History
- Physical Examination
- Differential Diagnoses of Community-Acquired Pneumonia
- Sputum Studies and Blood Culture
- Studies in HIV-Positive Patients with Community-Acquired Pneumonia
- Other Laboratory Tests for Community-Acquired Pneumonia
- Chest Imaging
- Fine-Needle Aspiration and Bronchoscopy With Bronchoalveolar Lavage
- Histologic Findings
- Pharmacologic Therapy
- Severity
- Outpatient Care in Community-Acquired Pneumonia
- Vaccination
- Guidelines
- Patient Instructions
- Acknowledgments
- Show All
- Media Gallery
- References