Background
Carpal tunnel syndrome (CTS) is the most common focal peripheral neuropathy. CTS is caused by entrapment of the median nerve at the wrist as it traverses through the carpal tunnel.
Acute CTS is a rare compartment syndrome of the carpal tunnel that occurs after major trauma, typically distal radius fracture. Diagnosis is based on clinical history and examination and does not require electrophysiological testing to proceed with surgery as soon as possible to relieve the pressure on the median nerve. [1, 2, 3]
Chronic CTS is a much more common condition and of more gradual onset, with intermittent symptoms initially and slow progression. The condition is often bilateral and almost always more prominent in the dominant hand. The syndrome is characterized by pain, paresthesia, and weakness in the median nerve distribution of the hand that are typically provoked by sleep or activities involving repetitive hand use. Electrodiagnostic studies are helpful to confirm the diagnosis. Treatment in mild cases may be nonsurgical and includes wrist splinting, but many patients require either open or endoscopic carpal tunnel release surgery with usually excellent outcome.
Modifying occupation or ergonomic conditions (eg, tools) may be beneficial. For excellent patient education resources, see Carpal Tunnel Syndrome.
Pathophysiology
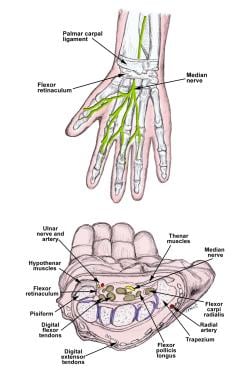
The median nerve is formed by C5-C7 fibers from the lateral cord and C8-T1 fibers from the medial cord of the brachial plexus. Muscular branches of the median nerve innervate most of the forearm flexor muscles and include the anterior interosseus nerve. The palmar cutaneous branch of the median nerve leaves the main trunk proximal to the wrist crease and provides sensation over the thenar eminence. See the image below.
Within the hand, the median nerve carries C8-T1 motor fibers to the abductor pollicis brevis, opponens pollicis, and superficial head of the flexor pollicis brevis muscles (thenar or recurrent motor branch) and the first and second lumbrical muscles. It supplies sensory innervation to the palmar surface of the thumb, and digits 2, 3, and the lateral half of digit 4 (via the common palmar digits nerves 1–3).
The median nerve crosses from the distal forearm to the hand through the carpal tunnel. The carpal tunnel is located at the base of the palm, just distal to the distal wrist crease. The floor of the carpal tunnel is formed by the carpal bones that create an arch. The fibrous flexor retinaculum, or transverse carpal ligament (TCL), is the roof of the carpal tunnel on the palmar side. The carpal tunnel is the narrowest at the level of the distal carpal row, at the level of the hook of the hamate bone. Within the carpal tunnel, the median nerve is physiologically flattened in configuration, and this flattening is maximal about 2–2.5 cm distal to the proximal edge of TCL. Along with the median nerve, 9 flexor digitorum tendons (8 tendons of the superficial and deep finger flexors and 1 of the flexor pollicis longus) pass through the carpal tunnel. The TCL is under tension, helps to maintain the carpal arch, and provides a retinacular pulley to the flexor tendons. See the image below.
CTS is caused by increased pressure in the carpal tunnel and on the median nerve. Compression of a peripheral nerve induces marked changes in intraneural microcirculation and nerve fiber structure, impairment of axonal transport, and alterations in vascular permeability, with edema formation and deterioration of nerve function. [4] Ischemia is a more significant factor of nerve fiber damage in acute median nerve compression, whereas in chronic entrapment, mechanical distortion plays a greater role. The pathology of idiopathic CTS is a noninflammatory fibrosis of the subsynovial connective tissue surrounding the flexor tendons. Biochemical studies of surgical specimens suggest that a variety of regulatory molecules may be inducing fibrous and vascular proliferation and that this may be a response to mechanical stresses. [5]
In a study of patients with CTS, when the wrist was in neutral position, the mean pressure in the carpal canal was 32 mm Hg versus 2.5 mm Hg in healthy patients. [6] The pressure increased to 94 mm Hg during wrist flexion (healthy patients 32 mm Hg) and 110 mm Hg during wrist extension (healthy patients 30 mm Hg). Carpal tunnel release brought about an immediate and sustained reduction in pressure.
In animal experiments, acute and severe compression caused persistent impairment of intraneural microcirculation due to mechanical injury to blood vessels. [7] In rabbits undergoing a graded compression of the tibial nerve, interference with venular flow was observed at a pressure of 20–30 mm Hg, while arteriolar and intrafascicular capillary flow was impaired at about 40–50 mm Hg. At 60–80 mm Hg, no blood flow ceased completely. [7]
In early or mild CTS, the median nerve has no morphological changes, and neurologic symptoms are intermittent. Prolonged increased pressure on the nerve results in segmental demyelination. The focal demyelination causes short segment conduction delay or conduction block across the site of entrapment. In more severe cases, wallerian degeneration and denervation of the thenar muscles develops.
The peripheral nerves of patients with underlying generalized neuropathies are more susceptible to compression injury, and the condition is associated in up to one third of cases with systemic medical conditions. Most cases of CTS are considered idiopathic. Some patients have an inherited increased susceptibility of the nerve to pressure, and on rare occasions CTS may be familial.
The concept of double crush syndrome was introduced in 1973 by Upton and McComas. [8] They proposed that focal compression of the nerve proximally predisposes it to injury at a more distal site along its course through impaired axoplasmic flow. The hypothesis remains of uncertain validity; there is no clear association between the frequency and severity of CTS and level of cervical radiculopathy. [9]
Etiology
Most cases of carptal tunnel syndrome (CTS) are idiopathic. In up to 50% of cases, an underlying condition may be identified that causes a locally reduced space in the carpal tunnel or increased susceptibility to nerve damage. Many metabolic or endocrine conditions are associated with increased risk of CTS, and several risk factors may coexist. Some cases may be attributed to excessive or repetitive hand movements.
Local causes with reduced space in the carpal tunnel include:
-
Congenital - Congenital small carpal tunnel, anomalous muscles and tendons, vascular anomalies including persistent median artery
-
Thickened transverse ligament
-
Tumor - Ganglion, hemangioma, cysts, lipoma, neuroma
-
Trauma, acute or chronic manifestation due to associated degenerative changes - Distal radius fracture (Colles fracture), dislocation or fracture of one of the carpal bones
-
Exostosis, osteophytes
-
Hematoma
-
Local infection - Septic arthritis, histoplasmosis
One study indicated that in patients who suffer a distal radius fracture, CTS is more likely to develop, within a 9-month postfracture period, in those who undergo open reduction and internal fixation (ORIF). The investigators also reported that the presence of diabetes mellitus was significantly associated with the development of CTS within 9 months following distal radius fracture (adjusted hazard ratio 2.76). [10]
Regional or systemic conditions with reduced space include:
-
Osteoarthritis
-
Rheumatoid arthritis
-
Mucopolysaccharidoses and mucolipidoses
-
Amyloidosis
-
Gout
-
Spasticity with persistent wrist flexion
Systemic conditions with increased susceptibility of nerves to pressure include:
-
Hereditary neuropathy with liability to pressure palsies (HNPP)
-
Diabetes mellitus
-
Other polyneuropathies
Other associated systemic conditions include:
-
Obesity
-
Hypothyroidism, hyperthyroidism
-
Alcoholism
-
Pregnancy (third trimester, usually bilateral), lactation
-
Menopause
-
Connective tissue disorders - Systemic lupus erythematodes, scleroderma, dermatomyositis
-
Rheumatoid arthritis
-
Sarcoidosis
-
Renal failure, hemodialysis
-
Acromegaly
-
Leukemia, multiple myeloma
-
Infections - Lyme disease, histoplasmosis
Work/activity-related risk is greater for highly repetitive wrist and finger use than forceful hand use. The combination of finger flexion with repetitive wrist motion is probably the most provocative stressor. The classic concept of repetitive motion-induced chronic tenosynovitis resulting in CTS has been questioned. Keyboard data entry has not been established as a cause of CTS.
Familial carpal tunnel syndrome has X-linked dominant (females), autosomal dominant, and recessive (childhood) forms. There is a bilateral presentation and anatomical abnormalities include a narrow carpal tunnel and thick transverse carpal ligaments.
Epidemiology
United States
Carpal tunnel syndrome (CTS) is the most common focal peripheral neuropathy. The reported incidence varies by location and methodology used. Prevalence rates for CTS are reported as 1–5% in the general population and 5–15% in industrial settings. An increasing temporal trend has been reported in several studies. [11, 12] A cross-sectional survey reported in 2001 calculated the lowest possible prevalence of symptomatic CTS in the general US population as 3.72%. [13]
Among residents of Olmsted County, Minnesota, the adjusted annual rates of medically diagnosed CTS increased from 258/100,000 in 1981–1985 to 424/100,000 in 2000–2005. [11] For this last period included in the study, the incidence in women was 542/100,000 and in men was 303/100,000. Generally, the most marked increases in CTS incidence were seen in younger age groups of both sexes in the first part of the study period and among older age groups in the final decades of the study. The cause of the increase is unclear, but it corresponds to an epidemic of CTS cases resulting in lost work days that began in the mid-1980s and lasted through the mid-1990s. The elderly present with more severe disease and are more likely to have carpal tunnel surgery. [11]
International
In the general population for a Dutch community, the prevalence rate of undetected CTS was 5.8% in adult women, and an additional 3.4% already carried the diagnosis of CTS. The overall prevalence rate for men was 0.6%. [14]
A primary care study in the United Kingdom from 2000 reported an annual incidence of CTS of 88/100,000 in men, and 193/100,000 in women. New presentations were most frequent in women aged 45–54 years. [15] In this study, CTS was as common as all other entrapment neuropathies combined.
A study in Italy reported a mean standardized annual incidence of 329/100,000 in the Siena area (Tuscany) from 1991–998, with 139 for men and 506 for women. The age-specific incidence for women increased gradually with age, reaching a peak from 50–59 years. In men, there was a bimodal distribution with peaks from 50–59 years and 70–79 years. [12]
A French study of CTS from 2002–2004 in patients aged 20–59 years reported a mean incidence rate per 1000 person-years that was higher in employed than unemployed persons (1.7 vs 0.8 in women and 0.6 vs 0.3 in men). Higher values were blue-collar workers and lower-grade services, sales, and clerical white-collar workers. [16]
Mortality/Morbidity
CTS is associated with high costs to the healthcare system and society. According to 1988 data from the United States, every year an estimated 1 million adults require medical treatment for CTS. [17] About 400,000–500,000 CTS surgeries annually were reported in 1995 with an economic cost of more than 2 billion dollars. [18]
In 1999, CTS cases were associated with a median number of 27 days lost from work, the highest number of any major disabling illness or injury. [19]
Demographics
Findings of the 1988 National Health Interview Survey indicate that CTS is 1.8 times more prevalent in Whites than nonWhites.
The reported female-to-male ratio ranges from 3:1 to about 10:1. Phalen's original series in 1970 included 280 women and 96 men (female-to-male ratio 3:1). [20] According to data from the 1980s, the prevalence of electrophysiologically confirmed symptomatic CTS is about 3% among women and 2% among men. [21]
Of the patients in Phalen's series, 58% were adults aged 40–60 years. [20]
Prognosis
Carpal tunnel syndrome (CTS) is not fatal, but it can lead to complete, irreversible median nerve damage, with consequent severe loss of hand function, if left untreated. For mild cases, conservative treatment is usually adequate. Surgical decompression usually produces good results. Patients with advanced thenar muscle atrophy usually do not recover fully after surgical decompression. CTS that is caused by or aggravated by an underlying disease (eg, diabetes) has a worse prognosis.
-
Scars from carpal tunnel release surgery.
-
Anatomy of the carpal tunnel.
-
Anatomy of the median nerve and the carpal tunnel.