Background
A subdural hematoma (SDH) is a collection of blood below the inner layer of the dura but external to the brain and arachnoid membrane (see the images below). Subdural hematoma is the most common type of traumatic intracranial mass lesion.
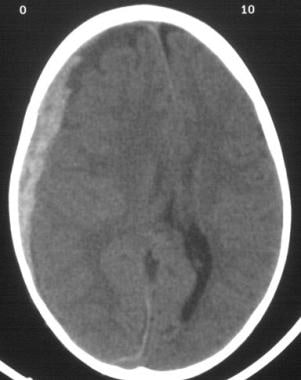 Acute subdural hematoma. Note the bright (white) image properties of the blood on this noncontrast cranial CT scan. Note also the midline shift. Image courtesy of J. Stephen Huff, MD
Acute subdural hematoma. Note the bright (white) image properties of the blood on this noncontrast cranial CT scan. Note also the midline shift. Image courtesy of J. Stephen Huff, MD
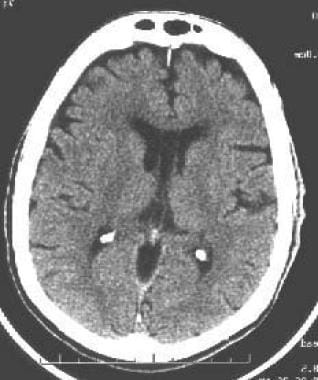
 A left-sided acute subdural hematoma (SDH). Note the high signal density of acute blood and the (mild) midline shift of the ventricles.
A left-sided acute subdural hematoma (SDH). Note the high signal density of acute blood and the (mild) midline shift of the ventricles.
SDH occurs not only in patients with severe head injury but also in patients with less severe head injuries, particularly those who are elderly or who are receiving anticoagulants. SDH may also be spontaneous or caused by a procedure, such as a lumbar puncture (see Etiology). Rates of mortality and morbidity can be high, even with the best medical and neurosurgical care (see Prognosis).
SDHs are usually characterized on the basis of their size and location and the amount of time elapsed since the inciting event age (ie, whether they are acute, subacute, or chronic). When the inciting event is unknown, the appearance of the hematoma on neuroimaging studies can help determine when the hematoma occurred. These factors, as well as the neurologic and medical condition of the patient, determine the course of treatment and may also influence the outcome. [1]
Generally, acute SDHs are less than 72 hours old and are hyperdense compared with the brain on computed tomography scans. The subacute phase begins 3–7 days after acute injury. Chronic SDHs develop over the course of weeks and are hypodense compared with the brain. However, SDHs may be mixed in nature, such as when acute bleeding has occurred into a chronic SDH.
Presentation varies widely in acute SDH. Many of these patients are comatose on admission. However, approximately 50% of patients with head injuries who require emergency neurosurgery present with head injuries that are classified as moderate or mild (Glasgow Coma Scale scores 9–13 and 14–15, respectively). Many of these patients harbor intracranial mass lesions.
In a large series of patients who developed intracranial hematomas requiring emergent decompression, more than half had lucid intervals and were able to make conversation between the time of their injury and subsequent deterioration. In a more comprehensive review of the literature on the surgical treatment of acute SDHs, lucid intervals were noted in up to 38% of cases.
These patients may be more likely to benefit from medical and surgical intervention when instituted in a timely fashion (ie, before further neurological deterioration). See Treatment, as well as the Medscape Reference article Head Injury.
Acute SDH is commonly associated with extensive primary brain injury. In one study, 82% of comatose patients with acute subdural hematomas had parenchymal contusions. [2] The severity of the diffuse parenchymal injury shows a strong inverse correlation with the outcome of the patient.
In recognition of this fact, an SDH that is not associated with an underlying brain injury is sometimes termed a simple or pure SDH. The term complicated has been applied to SDHs in which a significant injury of the underlying brain has also been identified.
Acute SDH is the most common type of traumatic intracranial hematoma, occurring in 24% of patients who present comatose. This type of head injury also is strongly associated with delayed brain damage, later demonstrated on CT scan. Such presentations portend devastating outcomes, and overall mortality rates are usually quoted at around 60%.
Significant trauma is not the only cause of SDH. Chronic SDH can occur in the elderly after apparently insignificant head trauma. Often, the antecedent event is never recognized. Chronic SDH is a common treatable cause of dementia. A minority of chronic SDH cases derived from acute SDH that have matured (ie, liquefied) because of lack of treatment.
For the most part, this review discusses acute and chronic SDHs; less information is available about the less common subacute SDHs. [3] Atraumatic SDH and subdural hygroma are briefly addressed.
Pathophysiology
The usual mechanism that produces an acute subdural hematoma (SDH) is a high-speed impact to the skull. This causes brain tissue to accelerate or decelerate relative to the fixed dural structures, tearing blood vessels. [4]
Often, the torn blood vessel is a vein that connects the cortical surface of the brain to a dural sinus (termed a bridging vein). In elderly persons, the bridging veins may already be stretched because of brain atrophy (shrinkage that occurs with age).
Alternatively, a cortical vessel, either a vein or small artery, can be damaged by direct injury or laceration. An acute SDH due to a ruptured cortical artery may be associated with only minor head injury, possibly without an associated cerebral contusion. In one study, the ruptured cortical arteries were found to be located around the sylvian fissure. [5]
The head trauma may also cause associated brain hematomas or contusions, subarachnoid hemorrhage, and diffuse axonal injury. Secondary brain injuries may include edema, infarction, secondary hemorrhage, and brain herniation.
Typically, low-pressure venous bleeding from bridging veins dissects the arachnoid away from the dura, and the blood layers out along the cerebral convexity. Cerebral injury results from direct pressure, increased intracranial pressure (ICP), or associated intraparenchymal insults.
In the subacute phase, the clotted blood liquefies. Occasionally, the cellular elements layer can appear on CT imaging as a hematocrit-like effect. In the chronic phase, cellular elements have disintegrated, and a collection of serous fluid remains in the subdural space. In rare cases, calcification develops.
Much less common causes of SDH involve coagulopathies and ruptured intracranial aneurysms. SDHs have even been reported to be caused by intracranial tumors.
It has been asserted that the primary brain injury associated with SDH plays a major role in mortality. However, most SDHs are thought to result from torn bridging veins, as judged by surgery or autopsy. Furthermore, not all SDHs are associated with diffuse parenchymal injury. As mentioned earlier, many patients who sustain these lesions are able to speak before their condition deteriorates—an unlikely scenario in patients who sustain diffuse damage.
Using a primate model, Gennarelli and Thibault demonstrated that the rate of acceleration-deceleration of the head was the major determinant of bridging vein failure. By using an apparatus that controlled head movement and minimized impact or contact phenomena, they were able to produce acute subdural hematomas in rhesus monkeys. In all cases, the sagittal movement of the head produced by an angular acceleration caused rupture of parasagittal bridging veins and an overlying subdural hematoma.
Gennarelli and Thibault reported that their results were consistent with the clinical causes of subdural hematoma, in that 72% are associated with falls and assaults and only 24% are associated with vehicular trauma. The acceleration (or deceleration) rates caused by falls and assaults are greater than those caused by the energy-absorbing mechanisms in cars, such as dashboard padding, deformable steering wheels, and laminated windshields. [6]
Acute subdural hematoma
Investigation of brain physiological and biochemical parameters in patients with acute traumatic SDH has suggested variables that might be associated with secondary injury to the brain.
In a study of brain biochemical patterns after acute subdural hematoma evacuation, Hlatky et al found that postsurgical patients who succumbed to their injury exhibited lower values of brain tissue oxygen tension and higher dialysate values of lactate and pyruvate in the brain underlying the hematoma. They suggested that identification of this brain biochemistry pattern after surgery might signify an evolving brain injury that warrants further evaluation or treatment. [7]
Cerebral blood flow (CBF) can become markedly reduced. Schroder et al reported that in 2 patients with acute SDH requiring emergent craniotomy, the hemisphere ipsilateral to the subdural hematoma demonstrated lower CBF than the contralateral hemisphere. Furthermore, CBF in both hemispheres was lower than normal. [8]
Impressive increases in CBF and cerebral blood volume (CBV) that could not be attributed to pCO2 or blood pressure changes were noted immediately after surgery. The authors speculated that the decreased CBV caused by the subdural hematoma was a result of a compressed microcirculation, which was caused by increased ICP. [8]
Herniation
Like other masses that expand within the skull, subdural hematomas may become lethal by increasing pressure within the brain, leading to pathologic shifts of brain tissue (brain herniations). Two common types of brain herniation are subfalcial (cingulate gyrus) herniation and transtentorial (uncal) herniation.
Subfalcial herniation may cause a cerebral infarct via compression of the anterior cerebral artery, and transtentorial herniation may cause an infarct via compression of the posterior cerebral artery. Transtentorial herniation is also associated with pressure on the third cranial nerve, causing decreased reactivity and then dilation of the ipsilateral pupil.
With progressive transtentorial herniation, pressure on the brainstem causes its downward migration. This tears critical blood vessels that supply the brainstem, resulting in Duret hemorrhages and death. Increased ICP may also decrease cerebral flood flow, possibly causing ischemia and edema; this further increases the ICP, causing a vicious circle of pathophysiologic events.
Chronic subdural hematoma
Chronic SDH is commonly associated with cerebral atrophy. Cortical bridging veins are thought to be under greater tension as the brain gradually shrinks from the skull; even minor trauma may cause one of these veins to tear. Slow bleeding from the low-pressure venous system often enables large hematomas to form before clinical signs appear.
Small SDHs often spontaneously resorb. Larger collections of subdural blood usually organize and form vascular membranes that encapsulate the SDH. Repeated bleeding from small, friable vessels within these membranes may account for the expansion of some chronic SDHs.
Chronic SDHs may also evolve from the liquefaction of an acute SDH, particularly one that is relatively asymptomatic. Liquefaction usually occurs after 1–3 weeks, with the hematoma appearing hypodense on a CT scan.
Some chronic SDHs may also enlarge from an osmotic gradient, drawing more fluid into the subdural space, or through the separate mechanism of calcification. [9]
In 1989, Kawakami discovered that the coagulation and fibrinolysis systems were both excessively activated in chronic SDH. [10] This results in defective clot formation and recurrent hemorrhage. Katano et al reported that elevated concentrations of tissue plasminogen activator are found in some chronic SDHs, and indicate a relatively high probability of recurrence. [11]
As an SDH expands in the subdural space, it raises the ICP and deforms the brain. The rise in ICP is initially compensated by efflux of CSF toward the spinal axis and compression of the venous system, expediting venous drainage through the jugular veins. During this stage, ICP rises relatively slowly, because the intracranial compliance is relatively high; in other words, the initial changes in intracranial volume are associated with small changes in ICP.
However, as the hematoma (and edema from associated parenchymal injury) expands, a limit is reached beyond which compensatory mechanisms fail. The intracranial compliance begins to decrease; small increases in intracranial volume are associated with larger increases in ICP. The ICP rises exponentially, leading to decreased cerebral perfusion and global cerebral ischemia. In a rapidly expanding hematoma, this whole process can happen in minutes.
In patients with chronic SDH, blood flow to the thalamus and basal ganglia regions appears to be particularly affected compared to that to the rest of the brain. Tanaka et al suggested that impaired thalamic function can lead to a spreading depression that impairs various cortical regions, thereby producing various clinical deficits. They found that a 7% decrease of CBF was commonly associated with headache, whereas a 35% decrease of CBF was associated with neurological deficit such as hemiparesis. [12]
Given that the pathophysiology of chronic SDH is often directly associated with cerebral atrophy, the fact that SDHs are associated with conditions that cause cerebral atrophy (eg, alcoholism, dementia) is not surprising. In one series, alcoholics constituted over half of the patient population. Most chronic SDHs are probably caused by head injury; other causes and predisposing factors include coagulopathy, use of anticoagulants (including aspirin), seizure disorders, and CSF shunts. [13]
Herniation syndromes
In addition to increasing the ICP, the hematoma deforms and displaces the brain. Eventually, transtentorial or subfalcine herniation can develop as the brain is pushed past the dural folds of the tentorial incisura or falx, respectively.
Tonsillar herniation through the foramen magnum may develop if the whole brain stem is forced down through the tentorial incisura by elevated supratentorial pressure. Although much less common than supratentorial SDH, infratentorial subdural hematoma can develop and cause tonsillar herniation and brainstem compression.
Characteristic herniation syndromes may develop as the brain shifts. As the medial temporal lobe, or uncus, herniates past the tentorium, it can compress the ipsilateral posterior cerebral artery, oculomotor nerve, and cerebral peduncle. Clinically, the consequent oculomotor nerve palsy and cerebral peduncle compression are often manifested by an ipsilaterally dilated pupil and a contralateral hemiparesis.
The patient also may develop a stroke of the posterior cerebral artery distribution. In approximately 5% of cases, the hemiparesis may be ipsilateral to the dilated pupil. This phenomenon is called the Kernohan notch syndrome and results when uncal herniation forces the midbrain to shift so that the contralateral cerebral peduncle is forced against the contralateral tentorial incisura.
Subfalcine herniation caused by midline brain shift may result in compression of anterior cerebral artery branches against the fixed falx cerebri, leading to infarcts in an anterior cerebral artery distribution.
Spontaneous subdural hematoma
Spontaneous SDH is rare. The literature is limited to sporadic case reports. These cases often have an arterial source; they are usually associated with the same pathology as that involved in subarachnoid or intracerebral hemorrhage. The blood from a ruptured aneurysm may dissect through the brain parenchyma or subarachnoid space into the subdural space.
Likewise, the blood released from a "hypertensive" intracerebral hemorrhage can dissect into the subdural space. In fact, a case has been reported of an acute spontaneous SDH precipitated by cocaine abuse.
Coagulopathy, occasionally associated with malignancy, also has been associated with spontaneous SDH. SDH also can be caused by bleeding from intracranial tumors. The treatment of spontaneous SDH is similar to that of SDH caused by trauma, but the underlying cause must be sought and treated.
Subdural hygroma
Some chronic SDHs may be derived from subdural hygromas. Brain atrophy or loss of brain tissue due to any cause, such as alcoholism, or stroke, may provide either an increased space between the dura and the brain surface where a subdural hygroma can form (see the image below) or traction on bridging veins that span the gap between the cortical surface and dura or venous sinuses.
 Atrophy of the brain, resulting in a space between the brain surface and the skull, increases the risk of subdural hematoma (SDH).
Atrophy of the brain, resulting in a space between the brain surface and the skull, increases the risk of subdural hematoma (SDH).
Hygromas probably form after a tear in the arachnoid allows CSF to collect in the subdural space. A subdural hygroma may therefore also occur after head trauma; they are frequently asymptomatic.
Etiology
Acute subdural hematoma
Causes of acute SDH include the following:
-
Head trauma [4]
-
Coagulopathy or medical anticoagulation (eg, warfarin [Coumadin], heparin, hemophilia, liver disease, thrombocytopenia)
-
Nontraumatic intracranial hemorrhage due to cerebral aneurysm, arteriovenous malformation, or tumor (meningioma or dural metastases)
-
Postsurgical (craniotomy, CSF shunting)
-
Intracranial hypotension (eg, after lumbar puncture, lumbar CSF leak, lumboperitoneal shunt, spinal epidural anesthesia [14]
-
Child abuse or shaken baby syndrome (in the pediatric age group)
-
Spontaneous or unknown (rare)
Chronic subdural hematoma
Causes of chronic SDH include the following:
-
Head trauma (may be relatively mild, eg, in older individuals with cerebral atrophy) [4]
-
Acute subdural hematoma, with or without surgical intervention
-
Spontaneous or idiopathic
Risk factors for chronic SDH include the following:
-
Chronic alcoholism
-
Epilepsy
-
Coagulopathy
-
Anticoagulant therapy (including aspirin)
-
Cardiovascular disease (eg, hypertension, arteriosclerosis)
-
Thrombocytopenia
-
Diabetes mellitus
In younger patients, alcoholism, thrombocytopenia, coagulation disorders, and oral anticoagulant therapy have been found to be more prevalent. Arachnoid cysts are more commonly associated with chronic SDH in patients younger than 40 years.
In older patients, cardiovascular disease and arterial hypertension are found to be more prevalent. In one study, 16% of patients with chronic SDH were on aspirin therapy. Major dehydration is a less commonly associated condition and is found concurrently in only 2% of patients.
Epidemiology
Acute SDHs have been reported to occur in 5–25% of patients with severe head injuries, depending on the study. The annual incidence of chronic SDH has been reported to be 1.7–20.6 cases per 100,000 population. [15] Subsequent studies have shown a higher incidence, probably because of better imaging techniques, aging population, and use of anticoagulation. [16]
Sex- and age-related differences in incidence
Overall, SDHs are more common in men than in women, with a male-to-female ratio of approximately 3:1. Men also have a higher incidence of chronic SDH. The male-to-female ratio has been reported to be 2:1.
The incidence of chronic SDH appears to be highest in the fifth through seventh decades of life. [17]
Adhesions existing in the subdural space are absent at birth and develop with aging; therefore, bilateral subdural hematomas are more common in infants. Interhemispheric SDHs are often associated with child abuse. [18]
Prognosis
Acute subdural hematoma
Acute SDH is associated with high mortality rates, ranging from 50% to 90% in patients presenting with Glasgow Coma Scale (GCS) scores of 8 or less. The overall prognosis for patients with acute SDH remains challenging, with fewer than 25% of all cases achieving full recovery without major neurological deficits. [19, 20, 21, 22, 1]
Several series have shown an increase in favorable outcome in younger patients. [19] Age younger than 40 years was associated with a mortality rate of 20%, whereas age 40–80 years was associated with a mortality rate of 65%. Age older than 80 years carried a mortality rate of 88%.
Ultimate prognosis is related to the amount of associated direct brain damage and the damage resulting from the mass effect of the hematoma. Simple acute SDH (ie, without parenchymal injury) accounts for about half of all cases and is associated with a mortality rate of about 20%. Complicated SDH (eg, with accompanying contusion or laceration of a cerebral hemisphere) is associated with a mortality rate of about 60%.
Findings on CT scan or MRI may help indicate prognosis. Such findings may include the following: [23]
-
Thickness or volume of the hematoma
-
Degree of midline shift
-
Presence of associated traumatic intraparenchymal lesions
-
Compression of the brainstem or basal cisterns
The first CT scan may underestimate the size of parenchymal contusions.
In general, a poor preoperative neurologic status may be a harbinger of a poor outcome. In addition to factors discussed above, poor prognostic indicators for acute SDH have been reported to include the following: [20, 24, 23]
-
Low initial (< 8) and postresuscitation (< 8) GCS [21]
-
Low GCS motor score on admission (< 5)
-
Pupillary abnormalities
-
Alcohol use
-
Injury by motorcycle accident
-
Ischemic damage [25]
-
Hypoxia or hypotension
-
Difficulty in controlling ICP
Elevated ICP postoperatively indicates a poor prognosis and may indicate the severity of the underlying brain injury (eg, trauma, secondary infarction).
Acute SDHs that would otherwise be considered operative by imaging criteria may resolve on their own, although this is rare. One series reported four such patients. [26]
Chronic subdural hematoma
Suggested prognostic factors associated with chronic SDH include:
-
Admission GCS score
-
Radiographic features (eg, midline shift and neomembranes)
-
Type of surgical intervention [27]
The mortality within 30 days of surgery is 3.2–6.5%. Eighty percent of patients resume their prehematoma level of function. Sixty-one percent of patients aged 60 years or younger and in 76% of patients older than 60 years have favorable outcomes. In one series, 89.4% of patients with chronic SDH who were treated with a closed drainage system had a good recovery and 2.2% worsened. [28]
Mori et al found that old age, pre-existing cerebral infarction, and subdural air after surgery correlated with poor brain expansion. [29] Stanisic et al reported a 14.9% postoperative recurrence rate; various factors were associated with this. [29]
The morbidity and mortality rates associated with surgical treatment of chronic SDH have been estimated at 11% and 5%, respectively. Between 86% and 90% of patients with chronic SDH are adequately treated after one surgical procedure.
-
Acute right-sided subdural hematoma associated with significant midline shift (ie, subfalcine herniation) shown on CT scan.
-
Bilateral chronic subdural hematomas shown on CT scan. Midline shift is absent because of bilateral mass effect. Subdural hematoma is bilateral in 20% of patients with chronic subdural hematoma.
-
An acute subdural hematoma is shown in this intraoperative photograph. Note the frontotemporoparietal flap used. The hematoma is currant jelly–like in appearance.
-
A left-sided acute subdural hematoma (SDH). Note the high signal density of acute blood and the (mild) midline shift of the ventricles.
-
A left-sided chronic subdural hematoma (SDH). Note the effacement of the left lateral ventricle.
-
Chronic subdural hematomas (SDHs) are commonly bilateral and have areas of acute bleeding, which result in heterogeneous densities. Note the lack of midline shift due to the presence of bilateral hematomas.
-
An isodense subdural hematoma (SDH). Note that no sulcal markings are below the inner table of the skull on the right side. This hematoma has scattered areas of hyperdense, or acute, blood within it.
-
Isodense subdural hematoma (SDH) as pictured with MRI. MRI can more readily reveal smaller SDHs, and, on MRI, the imaging of the blood products change characteristically over time.
-
Atrophy of the brain, resulting in a space between the brain surface and the skull, increases the risk of subdural hematoma (SDH).
-
An acute subdural hematoma (SDH) as a complication of a craniotomy. Note the significant mass effect with midline shift.
-
Acute subdural hematoma. Note the bright (white) image properties of the blood on this noncontrast cranial CT scan. Note also the midline shift. Image courtesy of J. Stephen Huff, MD
-
Subacute subdural hematoma. The crescent-shaped clot is less white than on CT scan of acute subdural hematoma. In spite of the large clot volume, this patient was awake and ambulatory. Image courtesy of J. Stephen Huff, MD.

