Practice Essentials
Originally classified as a glioma, medulloblastoma is referred to now as a primitive neuroectodermal tumor (PNET). This tumor accounts for approximately 7–8% of all intracranial tumors and 30% of pediatric brain tumors. Medulloblastoma is the most common malignant pediatric tumor in the central nervous system (CNS), accounting for nearly 20% of all childhood brain cancers and ~40% of all childhood tumors in the posterior fossa. This set of tumors is considered the most common brain malignancy among pediatric population. [2]
Signs and symptoms
Symptoms are often progressive over weeks to months, and it is not uncommon for patients to have an extended symptomatic period prior to initial diagnosis. Metastatic disease is commonly present at diagnosis (40%), and imaging of the entire craniospinal axis is an essential part of the initial diagnostic evaluation. [8]
Symptoms usually differ by anatomic location of the tumor, presence of disseminated disease, and by the presence of hydrocephalus.
Diagnosis
No specific biochemical test exists for the presence of medulloblastoma, although several molecular studies have revealed that histologically identical medulloblastomas are composed of distinct subgroups with different prognosis.
Management
Imaging is the primary mode of monitoring residual disease, efficacy of continuing medical treatment, and recurrence or metastasis. Because medulloblastoma is aggressive, frequent monitoring is essential. MRI should be repeated every 3 months the first year; every 4-6 months the second year; and yearly thereafter.
Surgery is still the mainstay initial therapy for medulloblastoma, as both a tool for diagnosis and as a risk-stratification factor. The recommendation is still to go for the safest resection possible, and if a second surgery is needed it is better to do it before starting the adjuvant treatment.
Radiation therapy is an outpatient procedure typically performed at least 2 weeks following operative intervention in order to allow adequate surgical incision healing.
Background
First used by Bailey and Cushing in 1925, [1] the term medulloblastoma described a series of tumors found in the cerebellum of children. Originally classified as a glioma, medulloblastoma is referred to now as a primitive neuroectodermal tumor (PNET). This tumor accounts for approximately 7–8% of all intracranial tumors and 30% of pediatric brain tumors. Medulloblastoma is the most common malignant pediatric tumor in the central nervous system (CNS), accounting for nearly 20% of all childhood brain cancers and ~40% of all childhood tumors in the posterior fossa. This set of tumors is considered the most common brain malignancy among pediatric population. [2] Medulloblastoma is a type of embryonal tumor. Embryonal tumors were described over the years as a collection of histologic entities that includes medulloblastoma and also included medulloepithelioma, CNS neuroblastoma, CNS ganglioneuroblastoma and atypical teratoid/rhabdoid tumor (ATRT) as well as primitive neuroectodermal tumors (PNET). All of that changed after the 2016 World Health Organization (WHO) reclassification. [3]
Pathophysiology
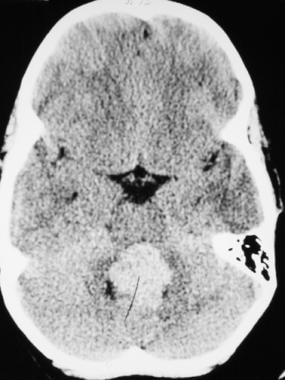
In the brain, medulloblastoma most often arises in the posterior fossa as shown in the image below. The tumor has the propensity of spreading throughout the CNS. Systemic metastases of this tumor, especially to bone, also have been recognized.
Epidemiology
Epidemiology data is changing ever since we have a better understanding of molecular and genetic behaviors of these tumors and especially after the new World Health Organization (WHO) classification from 2016. [3]
Demographics
Age and Sex
Incidence of medulloblastoma is 1.5-2 cases per 100,000 population, with 350 new cases in the United States each year.
Medulloblastoma accounts for 64.3% of all embryonal tumors in pediatric patients (0–19 years old), according to the Central Brain Tumor Registry of the United States (CBTRUS). Males displayed higher incidence rate relative to females (males: 0.16 vs. females: 0.12), except in patients < 1 year-old. [2] Overall ratio tend to be 1.5:1 for males. Males also tend to have poorer prognosis. Among all age group, the reports from CBTRUS citing the embryonal tumor group together, with total incidence rate of 0.25 per 100,000 per year with slight male predominance (0.29 vs. 0.2). Incidence of medulloblastoma decreases with age. Incidence was 0.55 per 100,000 population, 0.57 per 100,000 population, 0.32 per 100,000 population, and 0.16 per 100,000 population in children aged 0–4, 5–9, and 10–14 years, and adolescents aged 15–19 years, respectively. Incidence was highest in patients aged 1–4 years at diagnosis, but patients aged 10–14 years showed increased incidence from 2000 to 2013, and when looking at all age groups the total incidence peaks at ages 9 years and below. When looking at CBTRUS and SEER databases covering roughly the same period of time (2000/2001 to 2013) adult patients (20 years of age and older) are about 28% from all medulloblastoma patients. Interestingly enough, for the adult group there was a significant rise in incidence rate between 2001 and 2009 with subsequent significant decline in the rate between 2009 and 2013. [2, 4]
Race
In the United States, when looking at race for pediatric population (0-19 years), there is Caucasian and Asian/Pacific Islander predominance. In the collection of data from CBTRUS and SEER, white race was reported in the majority of cases (more than 80%). [2] Yet, when comparing black population to white population for the years 2001 to 2013, blacks displayed a non-significant increase in incidence and in mortality risk.
Mortality/Morbidity
The 5-year and 10-year survival rates among all patients are 73% and 64.7%, respectively. Patients aged 1–4 years have lower survival rates for each year post diagnosis relative to patients aged 5–9, 10–14, and 20+ years up to 5 years post diagnosis. Survival rates for males and females are similar up to 10 years post diagnosis. Black patients displayed slightly lower survival rates for each year post diagnosis compared to white patients. [2] Yet the reader needs to take into consideration that these survival numbers are from before the adjustment by molecular subtypes. When looking at the new classification (even before changing from 4 subtypes to 5), certain unsettled issues in epidemiology can become clearer. The group of infants < 1 year of age has a much poorer prognosis. In previous works it was described that the age group of children less than 4 years old are divided mainly to SHH (more than 50%) and group 3 (~40%). Whereas SHH pathway-driven tumors usually lead to a fair survival rate of 75% in 5 years for children below 3 years of age, group 3 for the same age group is having significantly worse survival rates. This accounts for the discrepancy between the old survival rates in CBTRUS of about 48% for children < 1 year old and 62% for children between 1 and 4 years of age, and the more positive picture that sometime can be seen in daily life. [5, 6]
In terms of morbidity, there are a lot of potential causes and complications for the patient diagnosed with medulloblastoma:
-
Hydrocephalus: The most common complication is hydrocephalus due to compression of the normal cerebrospinal fluid (CSF) pathways. Although this is a common complication, only 10-50% of patients with preoperative hydrocephalus will need a long-term ventricular shunt. Some children can be treated with an endoscopic third ventriculostomy.
-
Cerebellar dysfunction: Tumor infiltration of the cerebellum usually is in the midline, leading to difficulties with ambulation and truncal ataxia. This is more common than signs attributable to the cerebellar hemisphere (eg, extremity dysmetria). Cerebellar mutism syndrome occurs in approximately one quarter of patients who underwent resection of medulloblastoma in the immediate postoperative period. Brainstem invasion of the tumor was the only risk factor identified as having a positive correlation with the development of cerebellar mutism. [7]
-
Leptomeningeal dissemination: One of the most feared complications of medulloblastoma is dissemination within the CSF. Medical and, less commonly, surgical therapy must be directed at controlling dissemination to cranial nerves and spinal cord and related structures. This dissemination of disease portends to a high-risk stratification.
Prognosis
Medulloblastoma is a very aggressive tumor. Even after a good response to surgery and radiation, recurrence is common; most recurrences occur within 2 years after treatment.
The most common location of recurrence is at the primary tumor site in the posterior fossa.
With the use of adjuvant chemotherapy, incidence of recurrence in the spinal canal and the supratentorial region seems to decrease.
Systemic metastases, in the absence of a CSF shunting system, are also a recognized problem in 10-20% of patients. Bone is the most common site of systemic metastasis; regional lymph node sites follow.
The Collin law was first hypothesized for Wilms tumor and has been expanded since to cover many pediatric tumors thought to be congenital in origin.
The Collin law states that if a tumor has not recurred in a period of time equal to age of the patient plus 9 months, that patient can be considered to be cured.
The Collin law generally holds for medulloblastoma, however, several late recurrences (longer than 10 years after diagnosis) have been reported. The 5-year progression-free survival rate in that group is 70–80% for patients at low risk and 60–70% for patients at high risk.
Greater age at diagnosis has been associated with a better prognosis, most likely because adults more often harbor the less aggressive desmoplastic variant of medulloblastoma.
Why females have a longer recurrence-free interval is not understood.
For discussion of prognosis by subtypes, see Approach Considerations.
-
CT scan demonstrates a hyperdense lesion within the posterior fossa of an 8-year-old boy who presented with nausea and vomiting.
-
T1-weighted sagittal MRI of an 8-year-old boy who presented with nausea and vomiting reveals an enhancing tumor within the fourth ventricle. The child underwent a suboccipital craniotomy and resection of his medulloblastoma.
-
T1-weighted sagittal MRI of 4-year-old boy who presented with gait ataxia and precocious puberty. MRI shows a heterogenous enhancing tumor located within the fourth ventricle with marked hydrocephalus.
-
T1-weighted axial MRI shows heterogeneous enhancement of the medulloblastoma in a 4-year-old boy who presented with gait ataxia and precocious puberty.
-
Coronal MRI confirms the presence of the tumor within the fourth ventricle of a 4-year-old boy who presented with gait ataxia and precocious puberty.
-
High-power magnification hematoxylin and eosin (H&E) section of a typical medulloblastoma