Background
Craniosynostosis is a birth defect in which premature fusion of one or more cranial sutures occurs, often resulting in an abnormal head shape. It may result from a primary defect of ossification (primary craniosynostosis) or, more commonly, from a failure of brain growth (secondary craniosynostosis). Simple craniosynostosis is a term used when only one suture fuses prematurely. Complex or compound craniosynostosis is used to describe premature fusion of multiple sutures. When children with craniosynostosis, usually complex, also display other body deformities, this is termed syndromic craniosynostosis.
Pathophysiology
Normal skull development
Ossification of the cranial vault starts in the central region of each cranial bone and extends outward toward the cranial sutures.
The primary factor that maintains suture patency is ongoing brain growth and that the expanding dura is very osteogenic.
Normal skull growth occurs perpendicular to each suture.
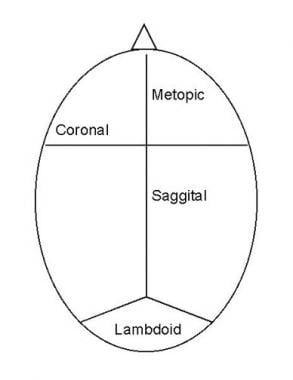
See the list below:
-
The coronal suture separates the 2 frontal bones from the parietal bones.
-
The metopic suture separates the frontal bones.
-
The sagittal suture separates the 2 parietal bones.
-
The lambdoid suture separates the occipital bone from the 2 parietal bones.
Normal Suture Closure (Open Table in a new window)
Suture |
Closure Begins (Years) |
Metopic |
0.2–2 (persists 10%) |
Sagittal |
22 |
Coronal |
24 |
Lambdoid |
26 |
Squamosal |
35-39 |
Sphenofrontal |
22 |
Sphenoparietal |
29 |
Sphenotemporal |
28–32 |
Masto-occipital |
26–30 |
Primary craniosynostosis
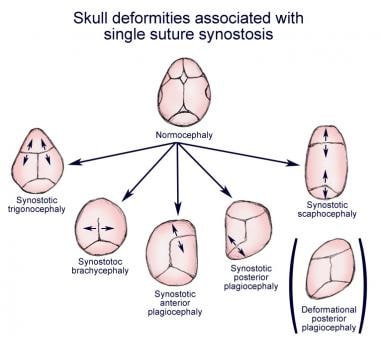
When one or more sutures fuse prematurely, skull growth can be restricted perpendicular to the suture. If multiple sutures fuse while the brain is still increasing in size, intracranial pressure can increase. [3, 1]
-
Scaphocephaly - Early fusion of the sagittal suture
-
Anterior plagiocephaly - Early fusion of one coronal suture
-
Brachycephaly - Early bilateral coronal suture fusion
-
Posterior plagiocephaly - Early closure of one lambdoid suture
-
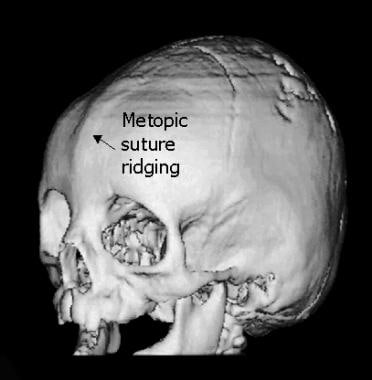
Trigonocephaly - Early fusion of the metopic suture
Secondary craniosynostosis
More frequent than the primary type, secondary craniosynostosis can result from early fusion of sutures due to primary failure of brain growth. Since brain growth drives the bony plates apart at the sutures, a primary lack of brain growth allows premature fusion of all the sutures. [3, 1]
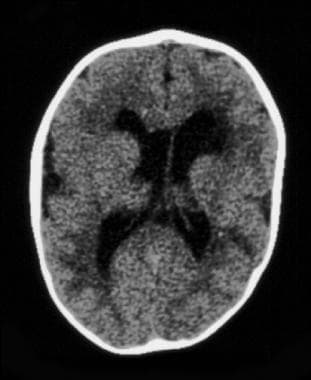 CT image demonstrating features of secondary craniosynostosis with cerebral atrophy. Cerebral atrophy is not present in primary craniosynostosis.
CT image demonstrating features of secondary craniosynostosis with cerebral atrophy. Cerebral atrophy is not present in primary craniosynostosis.
Intracranial pressure is usually normal, and surgery is seldom needed. Typically, failure of brain growth results in microcephaly. Premature suture closure does not compromise brain growth and does not require surgery to open sutures.
Intrauterine space constraints may play a role in the premature fusion of sutures in the fetal skull. [4] This has been demonstrated in coronal craniosynostosis. Other secondary causes of craniosynostosis include systemic disorders that affect bone metabolism such as rickets and hypercalcemia.
Epidemiology
Frequency
Incidence of craniosynostosis is 0.04–0.1% or 1 in every 2500 babies. [5] Of affected individuals, 2–8% have primary craniosynostosis. The remaining cases are secondary craniosynostosis, which frequently is accompanied by microcephaly. The frequencies of the various types of craniosynostosis are as follows: sagittal 50–58%, coronal 20–29%, metopic 4–10%, and lambdoid 2–4%. [6]
Mortality/morbidity
Raised intracranial pressure is rare with fusion of a single suture. It can occur in primary craniosynostosis when multiple sutures fuse.
-
Primary craniosynostosis: Although the major morbidity is due to the abnormal shape of the skull, intracranial pressure can be elevated. This occurs with a high frequency in multiple suture synostosis and rarely with single suture synostosis.
-
Craniosynostosis of 1–2 sutures: Cosmetic defect is the primary morbidity.
Demographics
Craniosynostosis is equally distributed in both boys and girls.
Craniosynostosis is evident at birth (neonatal period) when associated with other craniofacial abnormalities.
Secondary or primary craniosynostosis becomes evident as the child grows (0–18 mo).
Prognosis
Patients with primary craniosynostosis must be monitored after surgery. The vast majority of patients with primary, single suture synostosis have little or no morbidity following surgery. One systematic review of neurodevelopmental studies found some evidence that children with single suture synostosis are at increased risk for difficulties in cognitive, language, and motor domains during infancy (both pre- and post-surgery) and childhood. [9]
In secondary craniosynostosis, prognosis is dependent upon underlying etiology.
Patients with syndromic craniosynostosis can have a much more complicated clinical course due to the increased severity of the craniosynostosis and associated problems (eg, hydrocephalus and airway obstruction). They are also at increased risk of intellectual disability, and social and attention problems. [10, 11] A multidisciplinary approach is important in the management of the complex problems of these patients.
-
Diagram of a neonate's skull demonstrating the location of the sutures.
-
Frontal view showing a fused and ridged metopic suture on 3-dimensional CT.
-
CT image demonstrating features of secondary craniosynostosis with cerebral atrophy. Cerebral atrophy is not present in primary craniosynostosis.
-
Positional molding. Note the anterior displacement of the right occiput and of the right frontal region on the same side, which differentiate positional molding from posterior plagiocephaly craniosynostosis.
-
Posterior view of 3-dimensional cranial CT demonstrating early fusion of the lambdoid suture.
-
Isolated fusion of the metopic suture. Note that the remaining sutures are open.
-
Trigonocephaly. Note the triangular shape of the head.
-
Infant with primary craniosynostosis. The specific deformity of the skull is Kleeblattschadel or cloverleaf skull.
-
Skull deformities associated with single suture synostosis.
-
Positional plagiocephaly. Note anterior position of the ear on the side with occipital flattening.
-
Sagittal synostosis and the associated scaphocephaly seen on skull radiograph and 3-dimensional craniofacial CT scan.
-
Sagittal synostosis before and after cranial vault surgery and the associate improvement of scaphocephaly.
-
Unilateral coronal deformity with retrusion of the orbit and harlequin eye deformity. Note the ipsilateral deviation of the nasal radix and the contralateral deviation of the nasal tip.
-
Fusion of coronal sutures bilaterally. Note the increase transverse dimension and retrusion of the orbital rim.
-
Intraoperative view of bilateral coronal synostosis. Note the decreased anterior-posterior dimension, increased transverse width and retruded orbital rim.
-
Pre- and postoperative photos of metopic synostosis. Note the prominent forehead keel corrected after surgical repair.