Background
Band keratopathy is characterized by the appearance of an opaque white band of variable density across the central cornea, caused by the precipitation of calcium salts, primarily hydroxyapatite, on the underside of the corneal epithelium. [1] This corneal degeneration can result from a variety of causes, either systemic or local, with visual acuity decreasing in proportion to the density of the deposition. (See Etiology.)
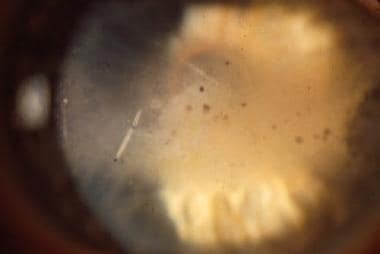 Band keratopathy. Note the bandlike whitish-grey lesion across the central corneal surface, most prominent on the exposure surfaces, sparing the superior and inferior cornea, and gaps representing corneal nerves passing through the Bowman membrane.
Band keratopathy. Note the bandlike whitish-grey lesion across the central corneal surface, most prominent on the exposure surfaces, sparing the superior and inferior cornea, and gaps representing corneal nerves passing through the Bowman membrane.
Superficial debridement often restores vision and comfort for most patients with band keratopathy; however, inadequate treatment of the inciting condition can lead to recurrence. (See Prognosis, Treatment, and Medication.)
Etiology
Corneal deposition of calcium salt
The concentration of cations (including calcium and phosphate) in tears approaches their solubility products. Evaporation of tears can concentrate these solutes to a degree that they precipitate, particularly in the interpalpebral zone of exposure in the eye. Additionally, chronically inflamed eyes (ie, uveitis) raise the tear pH, further favoring participation of solutes. [2, 3, 4, 5]
The use of silicone oil, often employed after treatment of an open globe injury, has been implicated in the incidence of band keratopathy. Interestingly, the retention time of the silicone oil (>6 months) is directly proportional to the risk for band keratopathy. The exact etiology of this interaction remains to be fully elucidated; however, hypotheses point to changes in pH and localized toxic reactions caused by the silicone oil. [6]
Systemic risk factors
The following conditions are associated with hypercalcemia, a risk factor for band keratopathy:
-
Hyperparathyroidism
-
Excessive vitamin D intake
-
Renal failure [7]
-
Hypophosphatasia
-
Paget disease
-
Sarcoidosis
Local ocular risk factors
Local ocular conditions associated with band keratopathy include the following [8, 9] :
-
Chronic uveitis
-
Keratitis sicca
-
Exposure keratopathy
-
Phthisis bulbi
-
End-stage glaucoma
-
Anterior mosaic dystrophy
-
Neurotrophic keratitis
-
Chronic herpes simplex stromal keratitis
-
Herpes zoster keratitis
Chemically associated risk factors
Drug-associated calcium deposition can result from the following:
-
Steroid phosphate preparations (see the images below) [10]
-
Long-term use of glaucoma medications
-
Pilocarpine-containing, mercury-based preservatives
-
Viscoelastic agents - Rare, early formulations; may be related to phosphate buffers
-
Topical medications containing phosphate buffers - Especially in the setting of chemical eye burns [13]
-
Intraocular use of tissue plasminogen activator [14]
-
Certain noxious vapors (Mercury and calcium bichromate)
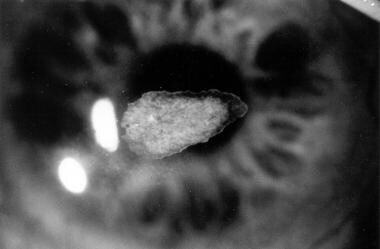 The image shown is of a patient who developed a calcium plaque following a corneal transplant and the use of a topical steroid phosphate preparation.
The image shown is of a patient who developed a calcium plaque following a corneal transplant and the use of a topical steroid phosphate preparation.
It is important to note, however, that a large percentage of cases of band keratopathy are idiopathic. Recent studies have demonstrated that upwards of 35% of cases have no identifiable systemic or local cause.
Prognosis
Patients with band keratopathy experience a decrease in vision as the deposition progresses across the visual axis. Commonly, the irregular surface epithelium causes a foreign body sensation. The ocular discomfort may worsen to the point of disability, especially as smaller segments of the plaque loosen and partially mobilize. The plaque itself often is visible and of cosmetic concern to the patient and family.
Superficial debridement or lamellar keratectomy can restore vision and comfort in most patients with band keratopathy, with a very low incidence of adverse outcomes following this procedure. Unless underlying conditions have been addressed, removing the calcium deposits in band keratopathy is associated with a higher rate of recurrence.
-
Band keratopathy. Note the bandlike whitish-grey lesion across the central corneal surface, most prominent on the exposure surfaces, sparing the superior and inferior cornea, and gaps representing corneal nerves passing through the Bowman membrane.
-
Calcium deposition associated with the use of dexamethasone phosphate. The calcium plaques appear as elevated white lesions at the edge of a persistent epithelial defect.
-
Total calcification of the cornea. Deep and superficial layers of the cornea are involved with this process.
-
The image shown is of a patient who developed a calcium plaque following a corneal transplant and the use of a topical steroid phosphate preparation.

