Background
Valsalva retinopathy was first described in 1972 by Thomas Duane as "a particular form of retinopathy, pre-retinal and hemorrhagic in nature, secondary to a sudden increase in intrathoracic pressure." [1] It was used to describe retinal hemorrhages in association with heavy lifting, coughing, straining at stool, or vomiting. The Valsalva maneuver was named after the Italian anatomist Antonio Maria Valsalva, who defined the Valsalva ligaments and anatomy related to the forcible exhalation effort against a closed glottis.
Valsalva retinopathy classically manifests as preretinal hemorrhage secondary to rupturing of superficial retinal vessels caused by physical exertion. The mechanism of a Valsalva maneuver is characterized by a sudden rise in intrathoracic or intraabdominal pressure against a closed glottis, which leads to a rapid rise of intravenous pressure within the eye, causing retinal capillaries to spontaneously rupture.
Prognosis usually is good, with spontaneous resolution occurring within months after onset, but depends on location of the hemorrhage and the layer of retina involved.
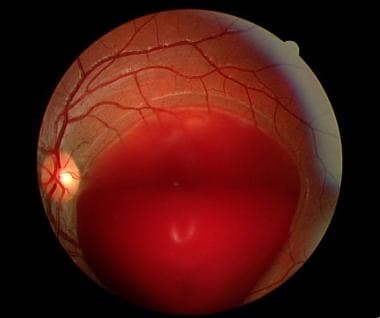 Initial presentation of a Valsalva retinopathy less than 24 hours following a Valsalva maneuver in an 18-year-old man. Note the large preretinal hemorrhage. Vision was finger counting at 5 feet.
Initial presentation of a Valsalva retinopathy less than 24 hours following a Valsalva maneuver in an 18-year-old man. Note the large preretinal hemorrhage. Vision was finger counting at 5 feet.
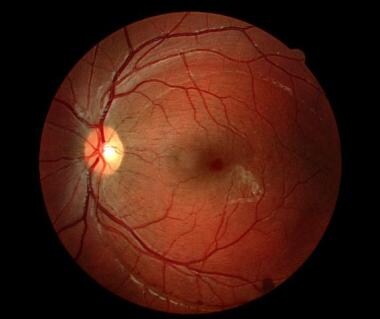 At 4-month follow-up of the same patient as in the image above, most of the large preretinal hemorrhage had cleared with observation alone. Note the wrinkled internal limiting membrane temporal to the macula and the resolving hemorrhage at the edge of the demarcation line of the stretched internal limiting membrane inferiorly. Vision had returned to 20/20.
At 4-month follow-up of the same patient as in the image above, most of the large preretinal hemorrhage had cleared with observation alone. Note the wrinkled internal limiting membrane temporal to the macula and the resolving hemorrhage at the edge of the demarcation line of the stretched internal limiting membrane inferiorly. Vision had returned to 20/20.
Pathophysiology
Increasing intrathoracic pressure against a closed glottis diminishes venous return to the heart, decreasing stroke volume and subsequently increasing the venous system pressure. [2, 3, 4, 5, 6]
The process occurs in 4 separate and distinct phases. First, a sudden increase in intrathoracic pressure decreases venous return to the right side of the heart. Second, diminished cardiac filling lowers the mean arterial pressure, slowing the pulse and leading to reflex tachycardia and peripheral vasoconstriction. Third, release of the strain causes a prompt reduction in the intrathoracic pressure, further lowering the blood pressure and simultaneously increasing the cardiac pressure. Finally, an abrupt increase in blood pressure occurs as venous blood surges back to the heart, inducing reflex bradycardia.
During a Valsalva maneuver, blood pressure in the peripheral portions of the body increases rapidly. As the sudden rise in intraocular venous pressure occurs, a spontaneous rupture of retinal capillaries ensues.
Epidemiology
Frequency
The frequency of Valsalva retinopathy is difficult to ascertain considering the rare nature of the condition.
United States
The incidence of Valsalva retinopathy in the United States has not been reported.
International
The worldwide incidence of Valsalva retinopathy has not been reported.
Mortality/Morbidity
Decreased vision occurs in the affected eye or eyes, ranging from complaints of floaters to complete loss of central vision. Vision often improves over weeks to months, depending on the severity of the retinal findings.
Race
No racial predilection exists.
Sex
No sexual predilection exists.
Age
Persons of any age can be affected. [7]
Prognosis
Prognosis generally is good, as complete recovery of vision (with observation) usually occurs within weeks to months following onset. However, visual prognosis depends on the location of the hemorrhaging and specifically the layer of retina involved.
Patient Education
There is no definitive way to prevent Valsalva retinopathy, but refraining from "holding your breath" during lifting, sneezing, and coughing may reduce the risk. Furthermore, breathing freely and openly helps decrease the chance of a Valsalva maneuver.
While lifting heavy objects, patients should be advised not to hold their breath for extended periods of time and to take multiple breaths between bearing-down phases. Exhaling while lifting or straining prevents a Valsalva maneuver because one cannot exhale against a closed glottis. Straining during bowel movements should be avoided.
For excellent patient education resources, visit eMedicineHealth's Eye and Vision Center. Also, see eMedicineHealth's patient education article Subconjunctival Hemorrhage (Bleeding in Eye).
-
Initial presentation of a Valsalva retinopathy less than 24 hours following a Valsalva maneuver in an 18-year-old man. Note the large preretinal hemorrhage. Vision was finger counting at 5 feet.
-
At 4-month follow-up of the same patient as in the image above, most of the large preretinal hemorrhage had cleared with observation alone. Note the wrinkled internal limiting membrane temporal to the macula and the resolving hemorrhage at the edge of the demarcation line of the stretched internal limiting membrane inferiorly. Vision had returned to 20/20.
-
A large preretinal hemorrhage in a 42-year-old man following a Valsalva maneuver. This image was taken 2 days after he underwent heavy straining while lifting weights.
-
This 58-year-old man with uncontrolled diabetes presented with complaints of a spot in his vision following straining during a bowel movement. He had active proliferative diabetic retinopathy, and the hemorrhage shown in this image stems from a broken neovascularized blood vessel secondary to a Valsalva maneuver.
-
Subhyaloid, sub–internal limiting membrane (ILM) hemorrhage in eye with Valsalva retinopathy. This image was originally published in the ASRS Retina Image Bank. Mitzy E. Torres Soriano, MD. Valsalva Retinopathy. Image Number 18218. © the American Society of Retina Specialists.
-
Subhyaloid, sub–internal limiting membrane (ILM) hemorrhage showing a fluid level and yellowish color as it settles over time. This image was originally published in the ASRS Retina Image Bank. Kathy Karsten, COT. Subhyaloid Hemorrhage, Right Eye. Number 23763. © the American Society of Retina Specialists.
-
Patient with history of gastroenteritis and episodes of vomiting followed by loss of central vision.
-
Patient with sudden loss of vision during labor and seen soon after giving birth.







