Practice Essentials
Spinal stenosis (progressive narrowing of the spinal canal) is part of the aging process, and predicting who will be affected is not possible. No clear correlation is noted between the symptoms of stenosis and race, occupation, sex, or body type. Treatment of spinal stenosis varies along a spectrum from conservative to surgical. While the degenerative process can be managed, it cannot be prevented by diet, exercise, or lifestyle.
Acute and chronic neck and lower back pain represent major health care problems in the United States. An estimated 75% of all people will experience back pain at some time in their lives. Most patients who present with an acute episode of back pain recover without surgery, while 3-5% of patients presenting with back pain have a herniated disc, and 1-2% have compression of a nerve root. Older patients present with more chronic or recurrent symptoms of degenerative spinal disease. (See Epidemiology.)
Progressive narrowing of the spinal canal may occur alone or in combination with acute disc herniations. Congenital and acquired spinal stenoses place the patient at a greater risk for acute neurologic injury. Spinal stenosis is most common in the cervical and lumbar areas. [1, 2, 3, 4] (See the images below.)
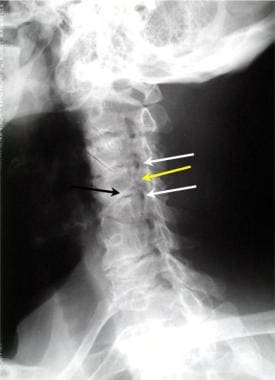 Oblique view of the cervical spine demonstrates 2 levels of foraminal stenosis (white arrows) resulting from facet hypertrophy (yellow arrow) and uncovertebral joint hypertrophy.
Oblique view of the cervical spine demonstrates 2 levels of foraminal stenosis (white arrows) resulting from facet hypertrophy (yellow arrow) and uncovertebral joint hypertrophy.
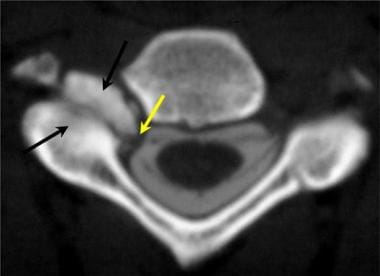 Axial cervical CT myelogram demonstrates marked hypertrophy of the right facet joints (black arrows), which results in tight restriction of the neuroforaminal recess and lateral neuroforamen.
Axial cervical CT myelogram demonstrates marked hypertrophy of the right facet joints (black arrows), which results in tight restriction of the neuroforaminal recess and lateral neuroforamen.
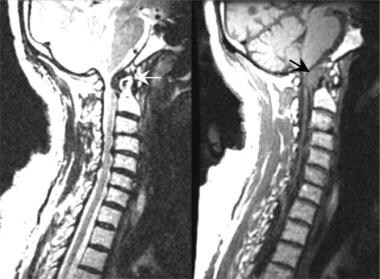 Short recovery time T1-weighted spin-echo sagittal MRI scan demonstrates marked spinal stenosis of the C1/C2 vertebral level cervical canal resulting from formation of the pannus (black arrow) surrounding the dens in a patient with rheumatoid arthritis. Long recovery time T2*-weighted fast spin-echo sagittal MRI scans better define the effect of the pannus (yellow arrow) on the anterior cerebrospinal fluid space. Note the anterior displacement of the upper cervical cord and the lower brainstem.
Short recovery time T1-weighted spin-echo sagittal MRI scan demonstrates marked spinal stenosis of the C1/C2 vertebral level cervical canal resulting from formation of the pannus (black arrow) surrounding the dens in a patient with rheumatoid arthritis. Long recovery time T2*-weighted fast spin-echo sagittal MRI scans better define the effect of the pannus (yellow arrow) on the anterior cerebrospinal fluid space. Note the anterior displacement of the upper cervical cord and the lower brainstem.
 Posterior view from a radionuclide bone scan. A focally increased uptake of nuclide (black arrow) is demonstrated within the mid-to-upper thoracic spine in a patient with Paget disease.
Posterior view from a radionuclide bone scan. A focally increased uptake of nuclide (black arrow) is demonstrated within the mid-to-upper thoracic spine in a patient with Paget disease.
Lumbar spinal stenosis (LSS) implies spinal canal narrowing with possible subsequent neural compression.
-
Oblique view of the cervical spine demonstrates 2 levels of foraminal stenosis (white arrows) resulting from facet hypertrophy (yellow arrow) and uncovertebral joint hypertrophy.
-
Axial cervical CT myelogram demonstrates marked hypertrophy of the right facet joints (black arrows), which results in tight restriction of the neuroforaminal recess and lateral neuroforamen.
-
Short recovery time T1-weighted spin-echo sagittal MRI scan demonstrates marked spinal stenosis of the C1/C2 vertebral level cervical canal resulting from formation of the pannus (black arrow) surrounding the dens in a patient with rheumatoid arthritis. Long recovery time T2*-weighted fast spin-echo sagittal MRI scans better define the effect of the pannus (yellow arrow) on the anterior cerebrospinal fluid space. Note the anterior displacement of the upper cervical cord and the lower brainstem.
-
Posterior view from a radionuclide bone scan. A focally increased uptake of nuclide (black arrow) is demonstrated within the mid-to-upper thoracic spine in a patient with Paget disease.
-
T2-weighted sagittal MRI of the cervical spine demonstrating stenosis from ossification of the posterior longitudinal ligament, resulting in cord compression.
-
Severe cervical spondylosis can manifest as a combination of disk degeneration, osteophyte formation, vertebral subluxation, and attempted autofusion as depicted in this sagittal MRI. Also, note the focal kyphosis, which is typical in severe forms.
-
Lateral T2-weighted magnetic resonance imaging (MRI) scan demonstrating narrowing of the central spinal fluid signal (L4-L5), suggesting central canal stenosis.
-
Axial T2 magnetic resonance imaging (MRI) scan (L4-L5) in the same patient as in the above image, confirming central canal stenosis.
-
Trefoil appearance characteristic of central canal stenosis due to a combination of zygapophysial joint and ligamentum flavum hypertrophy.
-
Lumbar computed tomography (CT) myelogram scan demonstrates a normal central canal diameter.
-
Lateral and axial magnetic resonance imaging (MRI) scan demonstrating right L4 lateral recess stenosis secondary to combination of far lateral disk protrusion and zygapophysial joint hypertrophy.
-
Sagittal measurements taken of the anteroposterior diameter of the cervical spinal canal are highly variable in otherwise healthy persons. An adult male without spinal stenosis has a diameter of 16-17 mm in the upper and middle cervical levels. Magnetic resonance imaging (MRI) scans and reformatted computed tomography (CT) images are equally as effective in obtaining these measurements, while radiography is not accurate.
-
Oblique 3-dimensional shaded surface display CT reconstruction of right foraminal stenosis resulting from unilateral facet hypertrophy (black arrow). The volume of the reconstruction has been cut obliquely across the neuroforaminal canal.
-
Anterior view of a lumbar myelogram demonstrates stenosis related to Paget disease. Myelography is limited because of the superimposition of multiple spinal structures that contribute to the overall pattern of stenosis.
-
Lateral view of a lumbar myelogram performed in a patient who has been fused across the L4-L5 and the L5-S1 vertebral interspaces using transpedicular screws. Treatment of lumbar spinal stenosis may include decompression laminectomies, followed by the placement of transpedicular screws (yellow arrows) with a posterior stabilization bar.
-
Sagittal view of a 3-dimensional volume image of the lumbar spine in a patient with a posterior fusion using transpedicular screws in L4 and L5. Note that an interposition graft has been placed between L4 and L5 to maintain satisfactory
-
Lateral swimmer's radiographic view demonstrates compression of the anterior contrast-filled cervical thecal sac. The defect helps localize the stenosis; however, the pattern does not reflect lateral disc herniation or spondylosis directly.
-
Axial T2-weighted gradient echo MRI scan. Note the high-grade spinal stenosis resulting in severe upper cervical cord compression (arrows). This patient presented with a central spinal cord syndrome that improved following surgical decompression.
-
Sagittal T2-weighted MRI image demonstrates severe stenosis. Spinal stenosis is demonstrated at several levels (white and yellow arrows) resulting from a combination of disc annulus bulging (white arrow) and epidural soft-tissue thickening (yellow arrow).
-
Superior-to-inferior view of 3-dimensional volume reconstruction of central canal spinal stenosis resulting from chronic disc herniation. The patient presented with lower extremity weakness and loss of bladder control.
-
: Sagittal T2 weighted fast spin-echo (FSE) MRI scan of a meningioma of the lower thoracic spine obtained without contrast enhancement. The effect of the mass is better seen because of the contrast between the mass and the cerebrospinal fluid (CSF). The anterior spinal canal is occupied by a mass that displaces and compresses the conus medullaris (C) at the T12 level. The mass (white arrow) is of intermediate increased signal brightness, compared to the normal spinal cord.
-
Sagittal T1-weighted spin-echo (SE) MRI scan of a meningioma of the lower thoracic spine obtained following IV gadolinium contrast enhancement. The mass is better seen because of the contrast enhancement within the meningioma (M). The anterior spinal canal is occupied by a mass that displaces and compresses (white arrows) the conus medullaris (C) at the T12 level. The mass (white arrow) is of intermediate increased signal brightness, compared to the normal spinal cord.
-
Normal findings in the thoracic spine as demonstrated by CT myelography. Note the detail of the spinal cord and the ventral and dorsal nerves surrounded by contrast.
-
nal-cut view of 3-dimensional reconstruction CT scan of the thoracic spine in tuberculosis spondylitis. Note the central spinal cavity (black arrow). The vertebral endplate has compressed downward (double blue arrows). The advantage of 3-dimensional reconstructions is the ability to better evaluate preoperatively the type of surgery needed to stabilize spinal compression fractures.
-
Paraspinal abscess aspiration biopsy. The stains were positive for mycobacteria (black arrows; acid-fast stain, magnification X100).
-
With the patient in a prone position and using CT localization, a bone biopsy and aspiration were performed from the area of greatest destruction within the vertebral endplate (arrow).
-
Aspergillosis organisms were recovered from a lumbar disc space abscess. The patient had received a renal transplant 12 months prior to the infection (hematoxylin and eosin, magnification X40).
-
Long recovery time T2*-weighted fat-suppressed sagittal MRI scan of the thoracic spine demonstrates subtle enlargement of a thoracic vertebral body (double white arrows) and a slightly increased degree of signal brightness within the vertebral body (yellow arrow).
-
Paget disease of the thoracic spine. Thoracic spinal CT scan demonstrates enlarged vertebral body endplates (black arrows). The axial image on the left demonstrates the characteristic thickening of the bony matrix of the vertebral body.
-
Axial lumbar CT scan demonstrates marked right-sided spinal canal stenosis (black arrow) resulting from advanced right-sided facet hypertrophy. Note the vacuum disc sign within the intervertebral disc (double yellow arrow). The vacuum disc sign is further indication of degenerative changes and spinal instability.
-
Pantopaque tracer in the epidural spaces. Pantopaque can remain in the epidural and facial spaces for years following a myelogram. Chronic inflammatory arachnoiditis has been associated with a combination of trauma (bleeding) with administration of Pantopaque.
-
Localization of thoracic lesion prior to surgical correction. A needle/wire localization technique is used to ensure the correct surgical level. Such preoperative localizations save time in the operating suite while reducing the need for intraoperative radiology.
-
Sagittal 3-dimensional CT reconstruction of the lumbar spine in a patient with multiple myeloma. The central portions of the vertebral bodies (yellow arrows) have been replaced by the nonossified tumor.
-
Biopsy (yellow arrow) of a multiple myeloma mass (black arrow) that has replaced the lumbar spinal canal (blue arrow) completely.
-
Multiple myeloma. Photomicrograph of an aspiration biopsy specimen.
-
Three-dimensional surface CT image of the lumbar spine following transpedicular screw placement across the L4-L5 interspace. Note how the tips of the screws project beyond the anterior margins of the L5 vertebral body.
-
Axial CT image taken through L5 in a patient in whom transpedicular screws have been placed. Note that the screws (black arrows) are too far lateral and anterior. The iliac veins lie just anterior to tips of the screws (white arrows). Both the angle of screw placement and the length of the screws must be tailored to the individual patient.
-
Spinal stenosis. Sagittal multiplanar reconstruction (MPR) image from a CT scan of the lumbar spine following posterior decompression and fusion of the L4-L5 interspace. The interposition graft (white arrow) is posterior to the desired position. The patient remained asymptomatic. Follow-up imaging should focus upon the stability of the posterior fusion, the position of the pedicle screws, and the position of the interposition graft.
-
Sagittal reformatted image from a CT of the cervical spine following anterior spinal decompression and fusion. Surgical treatment of spinal canal stenosis often involves anterior vertebrectomy and bone graft interposition. The goal in such cases is to restore cervical spinal alignment (white line) while securing anterior stability. In this patient, the bone graft (double black arrows) has migrated forward (double yellow arrows).

