Background
Elbow fractures are commonly encountered in the acute care setting. Injury patterns for children and adults are quite different. Fractures of the elbow include extra-articular and intra-articular fractures. Extra-articular fractures include intercondylar fractures, supracondylar fractures, epicondylar fractures, and condyle fractures. Intra-articular fractures include trochlea and capitellum, radial head, and proximal ulnar fractures.
The examining physician must perform a thorough neurovascular examination with all suspected elbow fractures; recognize subtle fracture patterns; provide adequate immobilization; and assess whether fractures require admission, immediate orthopedic evaluation, or less urgent referral. [1, 2] Mechanism of injury for most elbow fractures is direct elbow trauma or a fall onto an outstretched hand. Patients may experience pain, swelling, and decreased range of motion.
The elbow is a hinge joint composed of 3 bones: the ulna, the radius, and the humerus. The 3 main articulations of the elbow are (1) the humeroradial articulation, which is formed by the radial head and the capitellum of the humerus; (2) the humeroulnar articulation, which is formed by the ulnar notch and the trochlea of the humerus; and (3) the superior radioulnar articulation, which is formed by the proximal part of the ulna and the radius. All articulations are contained in one synovial-lined capsule, which typically encases a hemarthrosis following injury.
Two main movements occur at the elbow: flexion and extension, which occurs primarily at the humeroulnar articulation, and pronation and supination, which occurs primarily at the radioulnar articulation.
Fracture patterns vary widely due to the mechanism of injury as well as the age of the patient. Direct trauma or a fall onto an outstretched hand is responsible for most elbow fractures. Neurovascular injury is a common complication of elbow fractures. The brachial artery is the most commonly injured artery and is seen especially in supracondylar fractures. The median nerve is the most commonly injured nerve, which is often due to a displaced supracondylar humerus fracture.
Fracture patterns vary markedly among different age groups. Supracondylar fractures are the most common elbow fracture in children because of the relative strength of surrounding ligaments in comparison to bone. Radial head fractures are the most common elbow fracture in adults.
Extra-articular Fracture Patterns
Intercondylar fractures
Intercondylar fractures occur when the condylar fragments are separated. See the image below.
They are much more common in adults than in children. Any distal humerus fracture in adults is more likely to be intercondylar than supracondylar.
The mechanism is force directed against the posterior elbow, such as a fall onto a flexed elbow, driving the olecranon against the humeral articular surface separating the condyles.
Fractures are often a T or Y shaped fracture of the distal humerus.
Treatment is often complicated and requires anatomic reduction either open or closed. [3]
Supracondylar fractures
The supracondylar fracture is the most common pediatric elbow fracture (60%), with the average age of 6.7 years, and is rarely seen after age 15 years. [4, 5] See the image below.
Complications include injuries to nerves (the median, radial, and anterior interosseous nerves are the most commonly injured).
Most deficits are neurapraxias that resolve with conservative management
Motor function usually returns in 7-12 weeks, and sensory function usually in 6 months. [6]
Vascular injuries should always be suspected with supracondylar fractures.
Ten percent of children have temporary loss of the radial pulse because of swelling and not direct arterial injury. [1]
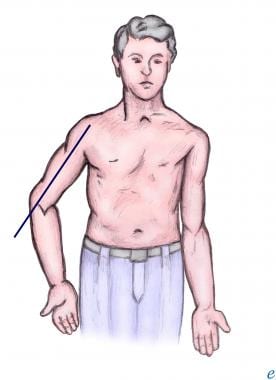
The most common complication for supracondylar fracture is cubitus varus or “gunstock deformity,” which is a loss of the carrying angle and results in more of a cosmetic disability than a functional one (see the image below).
Although rare (< 0.5%), the most serious complication is Volkmann ischemic contracture due to postfracture swelling, producing increased pressure in the forearm compartment and leading to muscle and nerve necrosis and eventual replacement by fibrotic tissue that causes contracture. [7]
In general, an orthopedic consultant best handles decisions regarding reduction of significantly angulated and displaced fractures.
If neurovascular structures are compromised, the emergency physician may need to apply forearm traction to reestablish distal pulses.
If pulse is not restored with traction, emergent operative intervention for brachial artery exploration or fasciotomy is indicated.
In children, nondisplaced, nonangulated fractures can be splinted (elbow in 90° of flexion); angulated fractures require reduction and splinting; and displaced fractures (see the image below) require reduction and percutaneous pinning on an urgent basis within 12-24 hours. In adults, supracondylar fractures generally require surgery.
Extension-type
Ninety-five percent of supracondylar fractures are of the extension-type and are displaced posteriorly because of an extension force.
-
Type I fractures - Undisplaced
-
Type II fractures - Displaced with posterior cortex still intact
-
Type III fractures - Displaced with both anterior and posterior cortex disrupted
Management of type I fractures consists of immobilization with the elbow in flexion, while type II and III are generally treated by closed reduction followed by pin fixation.
Type III fractures have significant displacement and have a high incidence of neurovascular injury and therefore require urgent orthopedic consultation in the ED.
Open reduction is reserved for vascular insufficiency with a probable entrapped brachial artery in the fracture site or an irreducible fracture.
Flexion-type
Five percent of supracondylar fractures are of the flexion-type and have anterior displacement due to a flexion force.
The mechanism usually involves direct anterior force with anterior displacement of the distal fragment.
Open fractures are relatively common because of the direct force.
-
Type I fractures - Undisplaced
-
Type II fractures - Displaced with anterior cortex still intact
-
Type III fractures - Displaced with both anterior and posterior cortex disrupted and distal fragment migrants anteriorly and proximately
Treatment of type I fractures is simple immobilization in the flexed position.
Treatment of type II and III fractures should be referred to an orthopedist emergently and is often reduced to an extension position and requires surgical management. [1]
Medial epicondyle fracture
Fractures of the epicondyles are considered extra-articular.
Medial epicondyle fractures are usually in children as an avulsion type injury (see the image below).
Fracture of the medial epicondyle occurs in approximately 10% of pediatric elbow fractures. Most of these injuries involve males aged 10-14 years.
Mechanisms include posterior elbow dislocation, throwing a baseball (Little League elbow), or a direct blow.
Edema and pain over the medial elbow is common.
Nondisplaced or minimally displaced medial epicondyle fractures are treated nonoperatively.
Fragment displacement greater than 1 cm or valgus instability is often treated with internal fixation.
Rarely, entrapment of the medial epicondyle can occur between the trochlea and the coronoid process of the ulna; this can be mistaken for the ossification center of the trochlea.
ED management consists of immobilization of the forearm in flexion and pronation and the wrist in flexion.
Lateral epicondyle fracture
Lateral epicondyle fracture is very rare and is usually due to an avulsion fracture.
Fracture of the lateral humeral epicondyle can be mistaken for the radiolucency of the epiphysis. [8]
Treatment is immobilization with the elbow flexed to 90º and the forearm in supination. [8]
Medial condyle fracture
Medial condyle fracture is rare and is usually found in children.
The mechanism is a fall on outstretched hand or excessive valgus stress.
This injury is often confused with medial epicondyle fractures.
Minimally displaced fractures are usually casted, whereas fractures with greater displacement usually require open or closed reduction with pin fixation. [8]
The outcome of medial condyle fractures depends on the degree of comminution of the fracture, the accuracy of the reduction, and the stability of fixation of the fracture fragment restoring congruity of the articular surface.
Lateral condyle fracture
Lateral condyle fracture is usually found in children and is the second most common pediatric elbow fracture. [9] See the image below.
The mechanism is a blow to the lateral elbow or from varus stress.
Minimally displaced fractures are usually casted, whereas fractures with greater displacement usually require open or closed reduction with pin fixation. [9]
Intra-articular Fracture Patterns
Trochlea fracture
Isolated trochlea fractures are rare and are usually associated with other elbow injuries.
Nondisplaced fractures are usually managed with a posterior splint, whereas displaced fractures require surgical management. [8]
Capitellum fracture
Isolated capitellum fractures are rare as they often occur in posterior elbow dislocations or with radial head fractures.
They are usually due to a fall on an outstretched hand.
Surgical repair is often indicated.
Radial head fractures
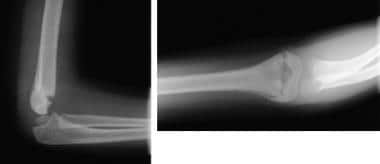
Radial head fracture is the most common of all fractures of the elbow and associated injuries are common. Radial head fractures have an annual incidence of 2.5-2.8 per 10,000 people, [10, 11, 12] which is approximately a third of all elbow fractures. See the image below.
The mechanism is usually a fall onto an outstretched hand.
Radial head fracture is characterized by point tenderness at the radial head (located along the lateral aspect of the elbow) and pain with pronation/supination.
A specific associated injury, the Essex-Lopresti lesion occurs when the radial-ulnar interosseous membrane is disrupted, causing distal radioulnar joint dissociation.
Careful examination of radiographs is important because fractures may be subtle.
For nondisplaced fractures, a sling with the elbow in flexion is usually adequate.
With displaced radial head fractures, patients can be placed in a posterior long-arm splint with the elbow in 90° of flexion and the forearm in full supination and placed in a sling for comfort.
Bipolar radial fractures have been reported involving simultaneous fracture of the distal radius and the radial head. This fracture pattern can lead to radial shortening and treating the wrist before the elbow may be advisable. [13]
Olecranon fractures
The mechanism is usually a direct blow or a fall onto an outstretched hand. See the image below.
The fracture line is usually transverse, passing into the trochlear notch. [8]
Patients demonstrate an inability to extend the elbow actively, along with point tenderness at the olecranon.
Ulnar nerve injury is common.
Patients can be placed in a well-padded, long-arm posterior splint with the elbow in 70° of flexion and the forearm neutral with respect to pronation/supination.
Nondisplaced fractures are usually managed conservatively, whereas all others often require surgical repair.
Prognosis
Supracondylar fracture
Children: Undisplaced fractures and properly managed displaced/angulated fractures result in no long-term functional deficits.
Adults: Usually, range of motion decreases somewhat but without functional deficit.
Radial head fracture
Usually, no functional loss occurs with nonoperative treatment.
Olecranon fracture
This fracture may result in loss of full extension but usually restores strength.
Olecranon fracture can be associated with post-traumatic arthritis of the elbow.
Most operative and nonoperative cases of olecranon fracture have a good outcome with no long-term deficits.
Complications
Cubitus varus
Cubitus varus, or "gunstock deformity," is the most common complication of supracondylar fractures. This loss of the carrying angle results in more of a cosmetic disability than a functional disability.
Volkmann ischemia
This is a form of compartment syndrome that can lead to muscle ischemia and permanent muscle contracture, particularly in children. [14] Symptoms suggestive of this complication include pain with passive extension of the fingers, refusal to open the hand, and forearm tenderness.
Median nerve injury
Displaced supracondylar humerus fractures may lead to median nerve dysfunction. Rarely does this result in complete nerve transection, and full return of function is common.
Malunion
Angulated or displaced fractures that remain unreduced lead to functional and cosmetic deformities.
Radial head fracture
Nondisplaced fractures that are immobilized for prolonged periods of time may have permanently decreased range of motion.
Comminuted radial head fractures associated with undiagnosed distal radial-ulnar joint injuries can lead to permanent wrist injuries and loss of pronation/supination motion.
Olecranon fracture
An ulnar nerve injury, although rare, may be associated with a displaced olecranon fracture.
Medial condyle fracture
Limited flexion and extension can occur with medial condyle fractures.
Nonunion/pseudoarthrosis of the fracture fragment can be a complication of medial condyle fractures in children. This may be related to the precarious blood supply of the distal fragment and because fractures that traverse the physeal plate are inherently less stable.
Posttraumatic arthritis due to chondral injury or residual joint incongruity may occur; it usually manifests several years later.
-
Intercondylar fracture.
-
Supracondylar fracture.
-
Displaced supracondylar fracture.
-
Medial epicondyle fracture.
-
Lateral condyle fracture.
-
Radial head fracture.
-
Olecranon fracture.
-
Anterior and posterior fat pads with radial head fracture.
-
Cubitus varus.
-
Typical supracondylar fracture. Fracture is obvious on both the anteroposterior (A) and lateral (B) views. Lateral view demonstrates an abnormal relation of the capitellum to the anterior humeral line, which passes along the anterior margin of the capitellum. Compare these images with the lateral view of the contralateral elbow (C), which shows the anterior humeral line passing normally through the middle third of the capitellum.
-
Typical supracondylar fracture. Anteroposterior (A) and lateral (B) views. Note the abnormal relation of anterior humeral line on the lateral view.
-
Normal lines. Lateral view shows the 2 lines used for radiographic analysis in patients with elbow trauma. The solid anterior humeral line is drawn along the anterior cortex of the distal humeral metaphysis and should pass through the middle third of the capitellum. Passage of the anterior humeral line either anterior to the capitellum or through the anterior third of the capitellum demonstrates that the capitellum is positioned too far posteriorly; this finding indicates a distal humeral fracture. The dashed radiocapitellar line is drawn through the radial neck and should pass through the capitellum. This relation should be examined on a frontal view as well. Failure of the radiocapitellar line to pass through the capitellum indicates radiocapitellar dislocation.
-
Minimally displaced radial head/neck fractures can be treated with early motion.