Practice Essentials
Genu valgum is the Latin-derived term used to describe knock-knee deformity. Whereas many otherwise healthy children have knock-knee deformity as a passing trait, some individuals retain or develop this deformity as a result of hereditary (see the image below) or genetic disorders or metabolic bone disease.
 This 9-year-old patient has symmetrical and progressive genu valgum caused by hereditary form of metaphyseal dysplasia. One method of treatment is to undertake bilateral femoral and tibial/fibular osteotomies, securing these with internal plates or external frames. However, hospitalization and attendant cost and risks, including peroneal nerve palsy and compartment syndrome, make this daunting for surgeon and family alike. Furthermore, mobilization and weightbearing may require physical therapy but must be delayed pending initial healing of bones.
This 9-year-old patient has symmetrical and progressive genu valgum caused by hereditary form of metaphyseal dysplasia. One method of treatment is to undertake bilateral femoral and tibial/fibular osteotomies, securing these with internal plates or external frames. However, hospitalization and attendant cost and risks, including peroneal nerve palsy and compartment syndrome, make this daunting for surgeon and family alike. Furthermore, mobilization and weightbearing may require physical therapy but must be delayed pending initial healing of bones.
The typical gait pattern is circumduction, requiring that the individual swing each leg outward while walking in order to take a step without striking the knee of the planted limb with the moving limb (hence the lay expression "knock knees"). Not only are the mechanics of gait compromised but also, with significant angular deformity, patellar tracking is compromised, resulting in anterior and medial knee pain.
For persistent genu valgum, treatment recommendations have included a wide array of options, ranging from lifestyle restriction and nonsteroidal anti-inflammatory drugs (NSAIDs) to bracing, exercise programs, and physical therapy. In recalcitrant cases, surgery may be advised. No consensus exists regarding optimal treatment. Some surgeons focus (perhaps inappropriately) on the patella itself, favoring arthroscopic or open realignment techniques. However, these efforts will fail if valgus malalignment of the extremity is significant. To correct limb alignment, corrective osteotomy or, in the skeletally immature patient, hemiepiphysiodesis (guided growth) may be indicated.
Osteotomy indications and techniques have been well described in standard textbooks and orthopedic journals and are not the focus of this article.
Hemiepiphysiodesis can be accomplished by using the classic Phemister bone block technique, the percutaneous method, hemiphyseal stapling, or the application of a single two-hole plate and screws around the physis. The senior author, having experience in each of these techniques, developed the last-mentioned one in order to solve two of the problems sometimes encountered with staples—namely, hardware fatigue and migration. [1, 2, 3, 4]
The focus of this article is on the indications, techniques, complications, and outcome of guided growth using the reversible plate technique for the correction of pathologic genu valgum.
Background
The term orthopaedia (from Greek orthos "straight" and pais "child") was coined by Nicholas Andry in 1741. Indeed, every parent hopes that his or her child will attain straight legs of equal length by maturity, with a normal gait and symptom-free activities.
Genu valgum is a frequent trigger for referral to the orthopedist, whose charge is to know whether, when, and how best to intervene. For most children, the philosophy of management has shifted from braces and physical therapy to benign neglect. Symptoms related to genu valgum include a circumduction gait, difficulty in running, knee pain, and, occasionally, patellar instability. Selected and symptomatic patients may be subjected to corrective osteotomy or, more recently, guided growth. This article makes a case for the latter treatment, exempting those patients with physiologic genu valgum (age < 6 y), who require no treatment, and those who have reached maturity.
Anatomy
The radiographic parameters relevant to defining genu valgum are best measured on a full-length anteroposterior (AP) radiograph of the legs. The patient should be standing with the knees touching and the patellae facing forward. The anatomic angle is measured between the femoral shaft and its condyles (normal angle, 84°); this is referred to as the lateral distal femoral angle (LDFA). The other relevant angle is the medial proximal tibial angle (MPTA), which is the angle between the tibial shaft and its plateaus (normal angle, 87°).
The mechanical axis (center of gravity) is a straight line drawn from the center of the femoral head to the center of the ankle; this should bisect the knee. This line is tilted 3º from vertical, reflecting the fact that the pelvis is wider than the ankles when the patient stands with the feet together. With allowances made for variations of normal, a mechanical axis that is within the two central quadrants (zones +1 or –1) of the knee is deemed acceptable.
With normal alignment, the leg lengths are equal, and the mechanical axis bisects the knee. This alignment places relatively balanced forces on the medial and lateral compartments of the knee and on the collateral ligaments, while the patella remains stable and centered in the femoral sulcus.
Pathophysiology
With normal alignment and gait, the physes and epiphyses are subjected to physiologic and alternating compression and tension and thus are shielded from pathologic stress. Balanced growth preserves straight legs and symmetrical limb lengths, resulting in normal gait and function. In genu valgum, as the mechanical axis shifts laterally (see the image below), pathologic stress is placed on the lateral femur, meniscus, and tibia, inhibiting growth and potentially leading to a vicious circle.
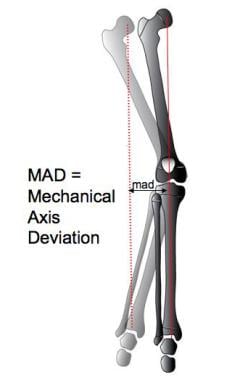 This diagram depicts genu valgum involving right leg (lighter shade), where mechanical axis falls outside knee. Goal of treatment is to realign limb and neutralize mechanical axis (dotted red line), thereby mitigating effects of gravity through guided growth of femur and/or tibia (whatever is required to maintain horizontal knee joint axis). Darker shade depicts normal alignment, with mechanical axis now bisecting knee.
This diagram depicts genu valgum involving right leg (lighter shade), where mechanical axis falls outside knee. Goal of treatment is to realign limb and neutralize mechanical axis (dotted red line), thereby mitigating effects of gravity through guided growth of femur and/or tibia (whatever is required to maintain horizontal knee joint axis). Darker shade depicts normal alignment, with mechanical axis now bisecting knee.
Not only is physeal growth inhibited, but also the Hueter-Volkmann effect is exerted upon the entire hemiepiphysis (lateral femoral condyle), preventing its normal expansion. According to the Hueter-Volkmann principle, continuous or excessive compressive forces on the epiphysis have an inhibitory effect on growth. Consequently, growth in the lateral condyle of the femur is suppressed globally, resulting in a shallow femoral sulcus and a propensity for the patella to tilt and subluxate laterally.
In children younger than 6 years, physiologic genu valgum is common but is self-limiting and innocuous. Management has shifted from orthotics and braces to parental education regarding the liklihood of spontaneous resolution. In children (of any age) with pathologic valgus, when the mechanical axis deviates laterally into zone +2 or beyond the lateral compartment of the knee (zone +3), regardless of the etiology, a number of clinical problems may ensue.
Medial ligamentous strain may be associated with recurrent knee pain. The patellofemoral joint may become shallow, incongruous, or unstable, causing activity-related anterior knee pain. In extreme cases, frank patellar dislocation with or without osteochondral fractures may ensue. During gait, medial thrust of the tibia relative to the femur may compromise the integrity of the restraining medial collateral ligaments, resulting in localized pain and progressive joint laxity.
In addition to knee pain and laxity, patients may develop a circumduction gait, swinging each leg outward to avoid knocking their knees together. A confounding factor may be the presence or exacerbation of outward tibial torsion. This gait pattern is awkward and laborious; the patient is unable to run, ride a bicycle, or participate safely and effectively in play or sports activities, and this inability may lead to social isolation and possible ridicule. If this condition is left untreated, its natural history is likely to be one of inexorable progression and deterioration.
Because patellar dislocation reflects an insidious and progressive growth disturbance, nonoperative management, with reliance on physical therapy and bracing, is of little value. During the adult years, premature and eccentric stress on the knee may result in hypoplasia of the lateral condyle, meniscal tears, articular cartilage attrition, and arthrosis of the anterior and lateral compartments.
The lifelong valgus knee presents a daunting challenge to the adult reconstructive orthopedist. Total knee arthroplasty (TKA) may be fraught with complications, including persistent malalignment, neurovascular compromise, patellar instability, and premature loosening of the prosthetic components.
Despite the current availability of gender-specific total knee components, or patellofemoral arthroplasty, these anatomic problems continue to pose a challenge. Therefore, it is in the best interest of the patient for the clinician to try to prevent such an outcome. Correction of genu valgum and neutralization of the forces across the knee are the goals of early and, if necessary, repeated intervention, which forestalls the need for more invasive adult reconstructive procedures.
Etiology
It is well recognized that toddlers aged 2-6 years may have physiologic genu valgum. This condition typically is symmetrical and gives rise to little or no discomfort and few functional limitations. Despite the sometimes impressive deformities, no treatment is warranted for this self-limiting condition. Bracing is meddlesome and expensive, and shoe modifications are unwarranted. The natural history of this condition is benign; therefore, parents simply need to be educated regarding what to expect and when to expect it. Annual follow-up until resolution may help assuage their fears.
In contrast, adolescent idiopathic genu valgum is neither benign nor self-limiting. Teenagers may present with a circumduction gait, anterior knee pain, and, occasionally, patellofemoral instability. The natural history of this condition may culminate in premature degenerative changes in the patellofemoral joint and in the anterior and lateral compartments of the knee.
Various other conditions, including postaxial limb deficiencies, genetic disorders such as Down syndrome, skeletal dysplasias, hereditary multiple exostoses, neurofibromatosis, and vitamin D–resistant rickets may cause persistent and symptomatic genu valgum. Some of these conditions require team management in conjunction with other healthcare providers; however, surgical intervention is still likely to be necessary to correct the malalignment of the knees.
Epidemiology
Adolescent idiopathic genu valgum may be familial or may occur sporadically. The true incidence is unknown. Certainly, it is one of the most common causes of anterior knee pain in teenagers and is a frequent reason for orthopedic consultation. Predisposing syndromes, such as those previously mentioned, are more apt to manifest in patients aged 3-10 years, and valgus may become severe if untreated. Whereas the tibiofemoral angle may not change, as the height increases and the stance becomes more widely based, the mechanical axis progressively shifts more laterally, a shift manifested by increasing knee pain, patellar instability, or both.
Regardless of the etiology, surgical correction of significant and symptomatic malalignment is warranted; when required in younger children, the process may have to be repeated as they continue to grow. [5] In light of the pathophysiology discussed previously, it is preferable to consider early and repeated intervention rather than try to calculate the precise timing for "definitive" intervention.
In countries where malnutrition is common and access to medical care is limited, the overall incidence of genu valgum is undoubtedly higher. Although polio has been largely eradicated, other infectious diseases may result in growth disturbances. Mistreated (or untreated) traumatic injuries cause physeal damage or overgrowth (for example), resulting in progressive and disabling clinical deformity. Likewise, untreated congenital anomalies, skeletal dysplasias, genetic disorders, nutritional deficiency, metabolic conditions, and rheumatologic diseases may cause genu valgum.
Prognosis
Provided that the appropriate criteria (ie, sufficient growth remaining, careful analysis and preoperative planning, proper plate insertion, and periodic follow-up) are met, the results of guided growth are uniformly gratifying. The parents and the surgeon must be patient, however, because growth is a slow process. The immediate satisfaction (carpentry) of osteotomies is supplanted by the delayed gratification of guided growth (gardening). The success of this technique is predicated on skillful harnessing of the inherent power of the growth plate. Even a sick physis can respond, given enough time; this is why the procedure works even in patients with skeletal dysplasias and vitamin D–resistant rickets. [6]
That patient satisfaction and family satisfaction are excellent is not surprising, given that guided growth, compared with osteotomy, is less invasive, relatively painless, more cost-effective, and less risky. Recovery time is minimal, and educational and recreational activities are only briefly interrupted. Consequently, previous arbitrary guidelines pertaining to minimum age and diagnoses have been abandoned. In the author's opinion, guided growth with a tension band has become the treatment of choice for most angular deformities of the knee. Osteotomy can still be performed if guided growth is unsuccessful (or vice versa).
Wiemann et al compared the use of the eight-Plate (Orthofix Medical, Lewisville, TX) for hemiepiphysiodesis (n = 24) with physeal stapling (n = 39) in 63 cases of angular deformity in lower extremities. The eight-Plate was as effective as staple hemiepiphysiodesis in terms of correction rate (~10º/y) and complication rate (12.8% vs 12.5%). However, patients with abnormal physes (eg, from Blount disease or skeletal dysplasias) did have a higher rate of complications than those with normal physes (27.8% vs 6.7%), though there was no difference between the eight-Plate group and the staple group. [7] We have not shared this experience; we have found the complication rate to be exceedingly low in both groups. [8]
After analyzing 35 patients, Jelinek et al reported that a shorter operating time for implantation and explantation was noted for the eight-Plate technique than for Blount stapling. [9]
Vaishya et al retrospectively studied 24 pediatric patients with bilateral (n = 11) or unilateral (n = 13) genu valgum deformity (35 knees) that required surgical correction in an attempt to evaluate the efficacy, correction rate, and complication rate associated with the use of the eight-Plate in this setting. [10] Excellent results were achieved in 91.6% of patients. There was one case (4.16%) of partial correction and one case (4.16%) of superficial infection, which was taken care of. There were two cases (8.33%) of overcorrection, which was gradually self-corrected during follow-up.
Ulusaloglu et al reported on risk factors for rebound deformity after correction of genu valgum in patients with skeletal dysplasia (N = 33; 59 limbs; 52 femurs, 29 tibias). [5] Although guided growth successfully corrected the alignment, there was a high incidence of recurrent deformity (43/59 limbs) as a "complication" of guided growth. A simple and economical approach to anticipating and managing this problem is to percutaneously remove just the metaphyseal screw when the mechanical axis has been restored to neutral (medial zone 1), observe for recurrence, and percutaneously reinsert the screw as necessary ("traveler plate"). Alternatively, the entire plate/screw can be removed and reinserted.
In view of the pathophysiology of unrelenting and progressive genu valgum, it is more prudent to perform repeated or intermittent guided growth, if necessary, rather than await adolescence for "perfectly timed" (not possible) physeal tethering or resort to corrective osteotomies. Dysplastic genu valgum is typically bilateral, involving both the femora and the tibiae; thus, six osteotomies (including the fibulas) would be required. Parents typically are more accepting of repeated minor interventions than of this scenario.
Patient Education
Parental education is paramount for successful treatment. With the child standing and in the prone position, parents can readily be instructed as to how to measure the intermalleolar distance (IMD) while the knees are touching. A simple and convenient monitoring method is for the parents to photograph the child standing, with the patellae facing forward and the knees touching. This should be done every month after plate insertion or removal; it provides invaluable and timely documentation of improvement following guided growth. Once the deformity has been corrected, parents should seek follow-up. This method is also a foolproof way of monitoring for overcorrection or for rebound deformity after implant removal.
-
This diagram depicts genu valgum involving right leg (lighter shade), where mechanical axis falls outside knee. Goal of treatment is to realign limb and neutralize mechanical axis (dotted red line), thereby mitigating effects of gravity through guided growth of femur and/or tibia (whatever is required to maintain horizontal knee joint axis). Darker shade depicts normal alignment, with mechanical axis now bisecting knee.
-
This 9-year-old patient has symmetrical and progressive genu valgum caused by hereditary form of metaphyseal dysplasia. One method of treatment is to undertake bilateral femoral and tibial/fibular osteotomies, securing these with internal plates or external frames. However, hospitalization and attendant cost and risks, including peroneal nerve palsy and compartment syndrome, make this daunting for surgeon and family alike. Furthermore, mobilization and weightbearing may require physical therapy but must be delayed pending initial healing of bones.
-
Heretofore, stapling was viable option. This outpatient procedure permitted simultaneous and multiple deformity correction, without casts or delayed weightbearing. However, concept of compressing and overpowering the physes has drawbacks of slower correction because fulcrum is within physis. Provided that rigid staples did not dislodge or fatigue, satisfactory correction could be realized. If hardware failed prematurely, either correction was abandoned or hardware was exchanged. Compared with osteotomies, this was risk worth taking--that is, until advent of better option.
-
Application of single eight-Plate per physis permits same correction as stapling, without potential drawbacks of implant migration or fatigue failure. Based on principle of facilitating rather than compressing physes, correction occurs more rapidly, and rebound growth, though possible, may be less frequent. When mechanical axis has been restored to neutral, plates (or metaphyseal screws) are removed (and replaced as necessary if recurrent deformity ensues).
-
This 14-year-old boy, weighing 132 kg, presented with activity-related anterior knee pain, circumduction gait, and difficulty with running and sports. Symptoms had been progressive over 18 months despite nonoperative measures that included physical therapy, activity restrictions, and nonsteroidal anti-inflammatory drug (NSAID) therapy.
-
At 9 months after insertion of eight-Plates in distal femora (1 per knee), patient's mechanical axis is approaching neutral, and his symptoms have abated. Plates were removed 2 months later, allowing full correction of his valgus deformities. Patient has not had recurrence.
-
This 14-year-old boy broke his distal femur 1 year previously. He was treated with internal fixation using condylar plate, and fracture healed uneventfully. However, he developed medial overgrowth of femur, which caused progressive and painful genu valgum. Note lateral displacement of mechanical axis into zone 2. One alternative is to perform supracondylar osteotomy with exchange of plate; this was declined.
-
Two options for instrumented and reversible hemiepiphysiodesis are (1) multiple staples and (2) tension-band plate. The latter, being flexible yet secure, avoids potential risks of hardware breakage or migration. Furthermore, growth is facilitated rather than restricted, and alignment is restored more rapidly.
-
At 1 year after guided growth of femur with eight-Plate, patient's mechanical axis is neutral, limb lengths are equal, and symptoms have abated; plate was then removed. Neither procedure required hospitalization or immobilization. Each time, patient was able to rapidly resume sports participation.
-
17-year-old male underwent arthroscopic reconstruction of left anterior cruciate ligament utilizing braided semitendinosis 1 year prior to this film. With ensuing growth, he developed progressive genu valgum with medial and anterior knee pain and difficulty running.
-
Fluoroscopic close-up view of patient's left knee demonstrates that despite chronologic age of 17 years, he has significant growth remaining. (Note arrows pointing to physis = growth plate). It was felt that most expedient and safe treatment would be guided growth. In consideration of his relative skeletal maturity, decision was made to apply tension-band plates to femur and tibia simultaneously, for sake of time.
-
Patient's legs are straight 11 months after pan-genu guided growth of medial femur and tibia. Pain has resolved, and he has resumed a fully active lifestyle. Limb lengths are equal, and knee remains stable.
-
Standing anteroposterior radiograph of legs confirms clinical findings; plates were therefore removed.
-
This 6-year-old girl, born with tibial dysplasia, underwent foot ablation at age 2 years, combined with surgical synostosis of distal fibula to tibial stump. She developed progressive genu valgum necessitating that prosthetist move post medially. However, she then experienced medial knee pain and stump irritation. Full-length weightbearing radiograph demonstrates lateral displacement of mechanical axis (red dotted line) to joint margin.
-
Treatment options are limited to osteotomy and guided growth. Osteotomy would require "down time"--out of her prosthesis and nonweightbearing while cut bone is healing.
-
Family chose option of guided growth, and plates were applied to distal medial femur and proximal medial tibia. Patient resumed full activities in her prosthesis, and this full-length radiograph, taken 1 year later, demonstrates normalization of mechanical axis. At this point, prosthetist moved post laterally. Knee pain and stump irritation have abated.
-
Close-up view demonstrates neutral mechanical axis and open growth plates. Note divergence of screws. At this point, plate was removed. Further growth will be monitored, and guided growth will be repeated if needed.
-
Clinical photograph shows her alignment just prior to hardware removal.
-
After guided growth for idiopathic genu valgum, this girl's parents sent periodic photos of her legs, documenting full correction over 8 months, whereupon they returned for implant removal. No "routine" office visits and x-rays were required in interim.
-
Shown is gross overcorrection of genu valgum. Because there is substantial growth remaining, even this deformity may be corrected by removing medial implant and placing a lateral tension band. The overcorrection was potentially preventable with smartphone monitoring. It is important to educate parents as to what to expect from guided growth and to encourage them to use their smartphones to document improvement with monthly pictures.



