Practice Essentials
Primary lymphoma of bone (PLB; also referred to as reticulum cell sarcoma, malignant lymphoma of bone, or osteolymphoma) is an uncommon entity that accounts for fewer than 5% of all primary bone tumors. [1] (See the images below.) Orthopedic surgeons typically encounter PLB as a solitary lesion with a variable radiographic appearance. Alternatively, patients with stage IV systemic lymphoma and skeletal involvement may be referred to orthopedic surgeons for the treatment of impending or pathologic fractures. Osseous involvement of disseminated lymphoma is not uncommon.
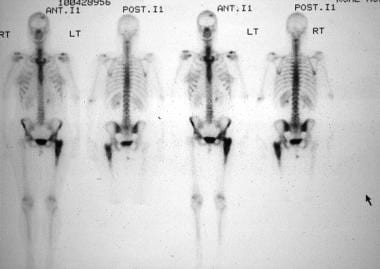 Total skeleton technetium-99m (99mTc) nuclear medicine scan reveals an isolated increased uptake in the left proximal femur at the site of this patient's bone lymphoma.
Total skeleton technetium-99m (99mTc) nuclear medicine scan reveals an isolated increased uptake in the left proximal femur at the site of this patient's bone lymphoma.
 A woman who is in the early part of her fifth decade presents with progressive left thigh pain and a limp. An anteroposterior radiograph of her left proximal femur reveals a lytic destructive process involving the subtrochanteric region, with medical cortical erosion, soft-tissue extension, and an associated lesser trochanteric avulsion fracture. The proximal femur is the most common site for primary bone lymphoma.
A woman who is in the early part of her fifth decade presents with progressive left thigh pain and a limp. An anteroposterior radiograph of her left proximal femur reveals a lytic destructive process involving the subtrochanteric region, with medical cortical erosion, soft-tissue extension, and an associated lesser trochanteric avulsion fracture. The proximal femur is the most common site for primary bone lymphoma.
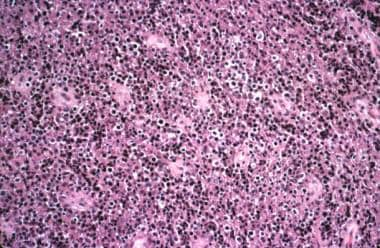 Diffuse infiltrate of large lymphoid cells is present, with cleared cytoplasm and hyperchromatic nuclei. Admixed small, reactive lymphocytes also are noted.
Diffuse infiltrate of large lymphoid cells is present, with cleared cytoplasm and hyperchromatic nuclei. Admixed small, reactive lymphocytes also are noted.
Randomized therapeutic trials for this rare disease are lacking. Most of the literature has consisted of retrospective reports on various chemotherapy and radiation therapy (RT) regimens.
RT for PLB provides adequate local control rates; however, when used alone, it results in high rates of systemic failure. The addition of chemotherapy provides superior overall survival and a decreased incidence of relapse. Multimodal chemoradiation can often even allow bone healing. Only about one third of patients with PLB ultimately require surgery for impending pathologic fractures.
Pathophysiology
The definition of PLB includes the following criteria:
-
Histologic documentation of lymphoma in the bone
-
A solitary bone lesion or multiple skeletal lesions
-
No involvement of lymph nodes (except regional lymph nodes) or other lymphoid tissue
Soft-tissue extension from the bone is a common feature of PLB.
Commonly involved bones in PLB, in order of decreasing frequency, include the following:
-
Femur
-
Humerus
-
Tibia
-
Spine
-
Pelvis
-
Sternum
-
Ribs
-
Bones of the skull and face
The metadiaphyseal portion of bone is the most common site of disease. Involvement of the small bones of the hands and feet is rare. Some studies have suggested that the mandible and maxilla are frequently affected sites, but confirmation that bone is the primary site of disease in these cases has not been well documented.
Etiology
The etiology of PLB is unknown. Viral agents and immunosuppression have been implicated in some cases. PLB has been documented as a posttransplant lymphoproliferative disorder in patients who have been immunosuppressed. Bone has also been documented as a site for primary lymphoma in patients with AIDS. Rarely, patients with Paget disease of bone may develop malignant lymphoma in the involved bone.
Cytogenetic and molecular abnormalities are associated with many different lymphomas. These also can be documented in the setting of primary bone lymphoma.
Some common recurrent abnormalities are as follows:
-
t(14;18)(q32;q21) - Overexpression of Bcl-2 protein, seen in 80-90% of follicular B-cell lymphomas and in 20% of diffuse large B-cell lymphomas
-
Rearrangements involving band 3q27 - Rearrangement of BCL6 gene, seen in 35% of diffuse large B-cell lymphomas
-
t(8:14)(q24;q32) - Overexpression of Myc protein, seen in 80% of Burkitt lymphomas; variant translocations t(2;8)(p11;q24) or t(8;22)(q24;q11), found in the remaining 20% of cases
-
t(2;5)(p23;q35) - Formation of nucleophosmin–anaplastic lymphoma kinase (NPM-ALK) fusion protein, seen in T-cell anaplastic large cell lymphoma
-
t(11;14)(q13;q32) - Overexpression of cyclin D1, seen in mantle cell lymphoma (not reported as a primary bone lymphoma)
Epidemiology
PLB accounts for fewer than 5% of primary bone tumors and fewer than 5% of extranodal lymphomas (or ~1% of all primary non-Hodgkin lymphomas). [2]
Secondary involvement of bone marrow is seen in 5-15% of patients with Hodgkin disease and 30-53% of patients with non-Hodgkin lymphoma. As many as 50% of patients with AIDS-associated Hodgkin disease have secondary bone-marrow involvement. [3, 4]
PLB may occur at any age, but it is most commonly diagnosed between the ages of 45 and 60 years; it is rare in children. [5] Males are affected more frequently than females (male-to-female ratio, 1.2-1.8:1).
Prognosis
In general, PLB has a better prognosis than most primary bone sarcomas or metastatic lesions do. The Surveillance, Epidemiology, and End Results (SEER) database reported 5- and 10-year survival rates of 58% and 45%, respectively, including patients from 1973-2005. [6] These rates were lower than those reported in most other literature.
A study from Memorial Sloan-Kettering Cancer Center reported a 5-year overall survival rate of 95% with chemoradiation and 78% with single-modality treatment. [7] The patients treated with only chemotherapy, however, tended to have more advanced-stage disease. The University of Miami reported a progression-free survival rate of 83% at 4 years. [8] Demircay et al reported a disease-free 5-year survival rate for patients younger than 60 years and older than 60 years of 90% and 62%, respectively. [9]
Positive prognostic factors for outcome include younger age at diagnosis, multimodal treatment, and localized disease; inclusion of rituximab in the treatment regimen may improve the prognosis. [10] Other factors (eg, type of lymphoma, sex, and lesion size) have not been shown to be significant on multivariate analysis.
-
Total skeleton technetium-99m (99mTc) nuclear medicine scan reveals an isolated increased uptake in the left proximal femur at the site of this patient's bone lymphoma.
-
Total skeleton technetium-99m (99mTc) nuclear medicine scan shows increased uptake in the left acromion, the site of bony involvement by lymphoma in this patient. The initial differential diagnosis suggested metastatic disease to bone in addition to multiple myeloma and lymphoma, in that order.
-
Coronal, T1-weighted magnetic resonance imaging (MRI) scan of the left shoulder reveals the replacement of the left acromion by a low-signal process extending into the surrounding soft tissue.
-
Coronal, T2-weighted magnetic resonance imaging (MRI) scan of the left shoulder reveals a high-signal process involving the left acromion and extending to the surrounding soft tissue. The MRI scan's features are suggestive only of a very high cellularity fluid-containing process, but they are nonspecific. Biopsy is required for a specific diagnosis.
-
Sections of the biopsy show a diffuse infiltrate of atypical large lymphoid cells with vesicular nuclei, small nucleoli, and moderate cytoplasm. Small reactive lymphocytes are in the background.
-
An immunohistochemical stain using an antibody directed against CD20 (B-cell marker) shows strong positivity in the large lymphoid cells. This is an example of a diffuse large B-cell lymphoma.
-
A woman who is in the early part of her fifth decade presents with progressive left thigh pain and a limp. An anteroposterior radiograph of her left proximal femur reveals a lytic destructive process involving the subtrochanteric region, with medical cortical erosion, soft-tissue extension, and an associated lesser trochanteric avulsion fracture. The proximal femur is the most common site for primary bone lymphoma.
-
An elderly woman presents with complaints of left shoulder pain of several months duration. A plain radiograph of the left shoulder (glenoid view) reveals a destructive lytic process eroding the cortical margins of the acromial process.
-
Diffuse infiltrate of large lymphoid cells is present, with cleared cytoplasm and hyperchromatic nuclei. Admixed small, reactive lymphocytes also are noted.
-
Immunohistochemical stain using an antibody against CD20 is positive in the large cells; this is a diffuse large B-cell lymphoma.
-
Clinical photo of a left shoulder shows a prominence in the midportion of the left clavicle. This 45-year-old man was suffering from local pain and tenderness but had no history of prior trauma.
-
Technetium-99m (99mTc) total skeleton nuclear medicine scan shows increased uptake in the midportion of the left clavicle, an area corresponding to the clinical site of bone enlargement.
-
Anteroposterior radiograph of the left clavicle reveals a mixed lytic and sclerotic destructive process within the midportion of the bone, with indistinct, permeative borders.
-
Another example of a diffuse large cell lymphoma. In addition to the large lymphoid cells with moderate cytoplasm, a few cells with lobate nuclei also are seen. Such cells are often observed in large cell lymphoma of the bone.
-
Plain radiographs in this 12-year-old patient with severely progressive right shoulder pain were interpreted as being normal. At most, they showed the existence of localized osteopenia in the right proximal humerus, but they did not demonstrate the presence of a discrete lesion within the bone. Based on the initial evaluation and plain radiographs, the patient was thought to have referred pain from the cervical region or brachial plexus.
-
Coronal, T1-weighted magnetic resonance imaging (MRI) scan of the upper thorax and bilateral shoulders reveals a marrow replacement low-signal process involving the entire right proximal humerus. The corresponding T2-weighted MRI scan showed a high-signal process in this area. This MRI scan was produced after plain radiographs were interpreted as normal and an MRI scan of the cervical spine and brachial plexus revealed the unsuspected findings in the humerus.
-
Histologic sections reveal a highly cellular neoplasm composed of cells with a high nucleus-to-cytoplasm ratio, scant cytoplasm, and fine nuclear chromatin. The cells showed immunohistochemical evidence of B-cell lineage and expressed terminal deoxynucleotidyl transferase (TdT), consistent with a precursor B-lymphoblastic lymphoma.