Davis DD, Kane SM. Neurilemmoma. Treasure Island, FL: StatPearls; 2023. [Full Text].
Gambacciani C, Grimod G, Sameshima T, Santonocito OS. Surgical management of skull base meningiomas and vestibular schwannomas. Curr Opin Oncol. 2022 Nov 1. 34 (6):713-722. [QxMD MEDLINE Link].
Shin DW, Ju C, Lee HS, Yoo HJ, Song SW, Cho YH, et al. Thirty-year clinical experience in gamma knife radiosurgery for trigeminal schwannomas. Sci Rep. 2022 Aug 23. 12 (1):14357. [QxMD MEDLINE Link]. [Full Text].
Park HH, Hong CK, Jung HH, Chang WS, Kim CH, Lee WS, et al. The Role of Radiosurgery in the Management of Benign Head and Neck Tumors. World Neurosurg. 2016 Mar. 87:116-23. [QxMD MEDLINE Link].
Feng S, Han S, Sun X, Li Y, Zhang Y, Li F, et al. Endoscopic retrosigmoid trans-petrosal fissure approach for vestibular schwannomas: case series. Neurosurg Rev. 2024 Sep 5. 47 (1):548. [QxMD MEDLINE Link].
Yu LG, Wang L, Zhao LJ, Zhang SN, Chen M, Cai L, et al. [Application of endoscopic resection of benign tumor in infratemporal fossa]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2020 Feb 7. 55 (2):87-93. [QxMD MEDLINE Link].
Roche PH, Bouvier C, Chinot O, Figarella-Branger D. Genesis and biology of vestibular schwannomas. Prog Neurol Surg. 2008. 21:24-31. [QxMD MEDLINE Link].
Guerrissi JO. Solitary benign schwannomas in major nerve systems of the head and neck. J Craniofac Surg. 2009 May. 20 (3):957-61. [QxMD MEDLINE Link].
Fan S, Wang H, Sun X, Gai C, Liang C, Wang G, et al. Comprehensive analysis of diagnosis and treatment in 99 cases of abdominal Schwannoma. Cancer Med. 2024 Aug. 13 (16):e70140. [QxMD MEDLINE Link]. [Full Text].
Cui H, Li P, Lu C, Huang X, Chen L, Liu N, et al. [Clinical diagnosis and treatment of primary retroperitoneal schwannoma: a report of 109 cases]. Zhonghua Yi Xue Za Zhi. 2015 Jun 9. 95 (22):1755-8. [QxMD MEDLINE Link].
Kano H, Kondziolka D, Khan A, Flickinger JC, Lunsford LD. Predictors of hearing preservation after stereotactic radiosurgery for acoustic neuroma. J Neurosurg. 2009 Oct. 111 (4):863-73. [QxMD MEDLINE Link].
Brito A, Silva JDS, Terry F, Punukollu A, Levy AS, Silva ALM, et al. Hearing preservation and quality of life in small to medium sized vestibular schwannomas after a wait and scan approach or stereotactic radiosurgery: a systematic review and meta-analysis. Acta Neurochir (Wien). 2024 Sep 9. 166 (1):361. [QxMD MEDLINE Link].
Pruijn IMJ, Parmaksiz M, Verheul JB, Mulder JJS, Kievit W, Kunst HPM. Health-Related Quality of Life in Patients With a Stable or Growing Vestibular Schwannoma Managed by Wait and Scan or Stereotactic Radiosurgery. Otolaryngol Head Neck Surg. 2024 Sep. 171 (3):823-832. [QxMD MEDLINE Link]. [Full Text].
Bakar B, Sumer MM, Cila A, Tekkok IH. An extreme lateral lumbar disc herniation mimicking L4 schwannoma. Acta Neurol Belg. 2009 Jun. 109 (2):155-8. [QxMD MEDLINE Link].
Ichinose T, Takami T, Yamamoto N, Tsuyuguchi N, Ohata K. Intratumoral hemorrhage of spinal schwannoma of the cauda equina manifesting as acute paraparesis--case report. Neurol Med Chir (Tokyo). 2009 Jun. 49 (6):255-7. [QxMD MEDLINE Link].
Strasilla C, Sychra V. [Imaging-based diagnosis of vestibular schwannoma]. HNO. 2017 May. 65 (5):373-380. [QxMD MEDLINE Link].
Fortnum H, O'Neill C, Taylor R, Lenthall R, Nikolopoulos T, Lightfoot G, et al. The role of magnetic resonance imaging in the identification of suspected acoustic neuroma: a systematic review of clinical and cost effectiveness and natural history. Health Technol Assess. 2009 Mar. 13 (18):iii-iv, ix-xi, 1-154. [QxMD MEDLINE Link].
Wu S, Liu G, Tu R. Value of ultrasonography in neurilemmoma diagnosis: the role of round shape morphology. Med Ultrason. 2012 Sep. 14 (3):192-6. [QxMD MEDLINE Link].
Yuan Y, Gao J, Xiong G, Guo L. Diagnostic accuracy of multiparametric ultrasound for peripheral nerve schwannoma. Acta Radiol. 2023 Apr. 64 (4):1608-1614. [QxMD MEDLINE Link].
Yousem SA, Colby TV, Urich H. Malignant epithelioid schwannoma arising in a benign schwannoma. A case report. Cancer. 1985 Jun 15. 55 (12):2799-803. [QxMD MEDLINE Link].
Tan M, Myrie OA, Lin FR, Niparko JK, Minor LB, Tamargo RJ, et al. Trends in the management of vestibular schwannomas at Johns Hopkins 1997-2007. Laryngoscope. 2010 Jan. 120 (1):144-9. [QxMD MEDLINE Link].
Rutten I, Baumert BG, Seidel L, Kotolenko S, Collignon J, Kaschten B, et al. Long-term follow-up reveals low toxicity of radiosurgery for vestibular schwannoma. Radiother Oncol. 2007 Jan. 82 (1):83-9. [QxMD MEDLINE Link].
Sade B, Mohr G, Dufour JJ. Vascular complications of vestibular schwannoma surgery: a comparison of the suboccipital retrosigmoid and translabyrinthine approaches. J Neurosurg. 2006 Aug. 105 (2):200-4. [QxMD MEDLINE Link].
Strauss C, Prell J, Rampp S, Romstöck J. Split facial nerve course in vestibular schwannomas. J Neurosurg. 2006 Nov. 105 (5):698-705. [QxMD MEDLINE Link].
Kondziolka D, Lunsford LD. Future perspectives in acoustic neuroma management. Prog Neurol Surg. 2008. 21:247-54. [QxMD MEDLINE Link].
Pillai P, Sammet S, Ammirati M. Image-guided, endoscopic-assisted drilling and exposure of the whole length of the internal auditory canal and its fundus with preservation of the integrity of the labyrinth using a retrosigmoid approach: a laboratory investigation. Neurosurgery. 2009 Dec. 65 (6 Suppl):53-9; discussion 59. [QxMD MEDLINE Link].
Shin DW, Sohn MJ, Kim HS, Lee DJ, Jeon SR, Hwang YJ, et al. Clinical analysis of spinal stereotactic radiosurgery in the treatment of neurogenic tumors. J Neurosurg Spine. 2015 Oct. 23 (4):429-37. [QxMD MEDLINE Link].
Kida Y, Yoshimoto M, Hasegawa T. Radiosurgery for facial schwannoma. J Neurosurg. 2007 Jan. 106 (1):24-9. [QxMD MEDLINE Link].
Langlois AM, Iorio-Morin C, Masson-Côté L, Mathieu D. Gamma Knife Stereotactic Radiosurgery for Nonvestibular Cranial Nerve Schwannomas. World Neurosurg. 2018 Feb. 110:e1031-e1039. [QxMD MEDLINE Link].
Dzierzęcki S, Turek G, Czapski B, Dyttus-Cebulok K, Tomasiuk R, Kaczor S, et al. Gamma knife surgery in the treatment of intracanalicular vestibular schwannomas. Acta Neurol Scand. 2020 May. 141 (5):415-422. [QxMD MEDLINE Link].
Smith DR, Saadatmand HJ, Wu CC, Black PJ, Wuu YR, Lesser J, et al. Treatment Outcomes and Dose Rate Effects Following Gamma Knife Stereotactic Radiosurgery for Vestibular Schwannomas. Neurosurgery. 2019 Dec 1. 85 (6):E1084-E1094. [QxMD MEDLINE Link]. [Full Text].
Yang L, Hu L, Zhao W, Zhang H, Liu Q, Wang D. Endoscopic endonasal approach for trigeminal schwannomas: our experience of 39 patients in 10 years. Eur Arch Otorhinolaryngol. 2018 Mar. 275 (3):735-741. [QxMD MEDLINE Link].
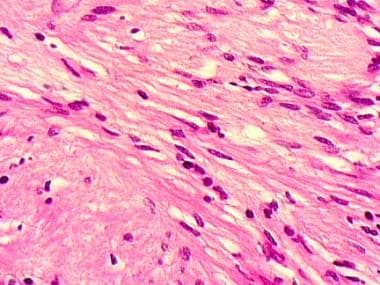 The cell of origin for a neurilemmoma is the Schwann cell, which is derived from the neural crest. These cells line the peripheral nerve processes.
The cell of origin for a neurilemmoma is the Schwann cell, which is derived from the neural crest. These cells line the peripheral nerve processes.

