Practice Essentials
Leukocytosis refers to an increase in the total number of white blood cells (WBCs) due to any cause. From a practical standpoint, leukocytosis is traditionally classified according to the component of white cells that contribute to an increase in the total number of WBCs. Therefore, leukocytosis may be caused by an increase in (1) neutrophil count (ie, neutrophilia), (2) lymphocyte count (ie, lymphocytosis), (3) monocyte count (ie, monocytosis), (4) eosinophilic granulocyte count (ie, eosinophilia), (5) basophilic granulocyte count (ie, basophilia), or (6) immature cells (eg, blasts). A combination of any of the above may be involved.
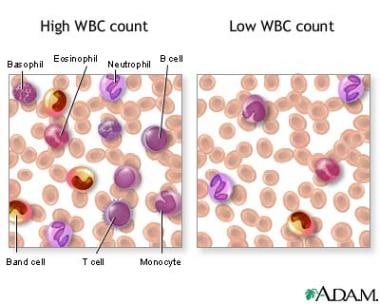
The image below is an illustration of high and low WBC counts.
Neutrophilia is divided into four categories based on the mechanism of neutrophilia: (1) increased production, (2) decreased egress from vascular space (demargination), (3) increased mobilization from the marrow storage pool, and (4) reduced margination into the tissue.
Clinically, dividing leukocytosis on the basis of its causes is more convenient. By dividing it according to causes, leukocytosis can be immediately applied for diagnostic purposes. Leukocytosis can result from infection; inflammation; allergic reaction; malignancy; hereditary disorders; drug effects, such as can occur in steroid administration; or other miscellaneous causes.
Workup in leukocytosis
In interpreting leukocytosis on the complete blood count (CBC), consider the following:
-
Clinical features
-
Duration
-
Differential
-
Remainder of the CBC
Bone marrow aspiration and biopsy may be necessary to differentiate leukemia from a benign condition (leukemoid reaction) if the patient has persistent leukocytosis.
Management of leukocytosis
In most cases, treatment for leukocytosis is not necessary. Instead, management of the underlying pathology is the goal in obtaining the leukocyte count.
In extreme instances of hyperleukocytosis syndrome (eg, acute leukemia), leukapheresis, hydration, and urine alkalinization to facilitate uric acid excretion are indicated; however, perform these treatments only in consultation with a hematologist, oncologist, or both. Direct treatment toward the underlying etiology.
Pathophysiology
Leukocytosis can be a reaction to various infectious, inflammatory, and, in certain instances, physiologic processes (eg, stress, exercise, a surgical procedure [as described below]). This reaction is mediated by several molecules, which are released or upregulated in response to stimulatory events that include growth or survival factors (eg, granulocyte colony-stimulating factor, granulocyte-macrophage colony-stimulating factor, c-kit ligand), adhesion molecules (eg, CD11b/CD18), and various cytokines (eg, interleukin-1, interleukin-3, interleukin-6, interleukin-8, tumor necrosis factor).
The peripheral leukocyte count is determined by several mechanisms, including (1) the size of precursor and storage pool of myeloid and lymphoid cells, (2) the rate of release of the cells from the storage pool in the bone marrow, (3) the rate of marginating cells out of blood vessels into the tissues, (4) the rate of consumption of the cells in the tissues (ie, cell loss), and (5) elimination by the spleen. The growth factors, adhesion molecules, and cytokines control the first four mechanisms listed above. [1]
Hyperleukocytosis (WBC count >100 X 109/L, or >100 X 103/µL) occurs in leukemia and myeloproliferative disorders. Hyperleukocytosis often causes vascular occlusion, resulting in ischemia, hemorrhage, and edema of the involved organs. The problem is most commonly observed in acute myelogenous leukemia with high WBC counts. Individuals often clinically present with mental status changes, stroke, and renal or pulmonary insufficiency. If the neutrophil count exceeds 3 x 105/μL as a reaction to extrinsic factors, such as infection, it is sometimes called a leukemoid reaction.
In a person with sickle cell disease, the baseline WBC count is elevated with a mean of 12-15 X 109/L (12-15 X 103/µL). This change mainly is due to a shift of granulocytes from the marginated pool to the circulating compartment. The segmented neutrophil count increases in both vaso-occlusive crisis and bacterial infection, in patients with sickle cell disease.
Postoperative leukocytosis is common. A clinical study in patients who had orthognathic (maxillofacial) surgery, which is clean-contaminated surgery, found that postoperative leukocytosis was associated with the preoperative white count and the duration of surgery. Though this study included adult patients, a large percentage were aged 20 years or younger. [2]
Leukocytosis and neutrophilia are very common in Sweet syndrome, or acute febrile neutrophilic dermatosis, with the syndrome being more common in adults. In a retrospective review, the age range of patients with Sweet syndrome was 7-84 years, with the disorder occurring more often in women. The etiology is unknown, but the syndrome is associated with a variety of conditions such as drug intake, autoimmune disease, malignancy, and infection, among others. [3]
A retrospective study to look for predictor variables for pulmonary embolism in children found leukocytosis (WBC>11,000) to be one of nine significant variables (odds ratio = 2.1). [4]
Epidemiology
Mortality/Morbidity
Clinically significant morbidity and mortality are frequently observed in patients with leukemic hyperleukocytosis. Hyperleukocytosis may result in tumor lysis syndrome and disseminated intravascular coagulopathy. In addition to well-known complications (eg, acute respiratory failure, pulmonary hemorrhage, central nervous system [CNS] infarction, hemorrhage), splenic infarction, myocardial ischemia, renal failure due to renal vessel leukostasis, and priapism have been reported.
A study by Tien et al indicated that hyperleukocytosis is an independent risk factor for poor prognosis in acute myelogenous leukemia, its impact being unassociated with a patient’s cytogenetic or mutational status. However, the detrimental effects of hyperleukocytosis were apparently reduced in study patients who underwent allogeneic hematopoietic stem cell transplantation in first complete remission, with overall and disease-free survival being significantly extended in these individuals. [5]
A study by Klein et al of patients with myelodysplastic and myeloproliferative neoplasms with neutrophilia (MDS/MPN-N; formerly called atypical chronic myelogenous leukemia) also found a positive survival impact from allogeneic hematopoietic stem cell transplantation. The overall survival rate was highest among the transplant patients, being 59% at 2 years. [6]
Spurious hyperkalemia may result from hyperleukocytosis. Claver-Belver et al described a case of T-cell acute lymphoblastic leukemia with a WBC count of 468.11 X 109/L. A biochemistry analyzer determined the patient's serum potassium level to be 7.3 mmol/L, but a blood gas analyzer determined the whole blood potassium value to be only 4.0 mmol/L. According to the investigators, the spuriously high serum potassium value was attributable to a centrifugation process for serum separation. Thus, it is important to recognize that such false findings may occur in the presence of a very high WBC count. [7]
In certain situations, leukocytosis may have a prognostic value. In a study performed mostly with adult patients, cardiac preoperative leukocytosis (defined by WBC >11,000) was found to be a strong predictor of postoperative medical complications. [8]
A study by Izhakian et al indicated that following lung transplantation, delayed leukocytosis is significantly linked to a higher mortality rate (hazard ratio = 1.52). The highest associated mortality was found when the delay was attributed to acute graft rejection. [9]
Age
Always remember that there are age-specific reference ranges for total WBC, neutrophil, and lymphocyte counts. The total WBC and neutrophil count in neonates younger than 1 week are physiologically higher than those of older children and adults. The proportion of lymphocytes and absolute lymphocyte count in children younger than 6 years are higher than those in adults. Failure to recognize age-specific lymphocytosis may lead to unnecessary investigations (see the table below for reference ranges of age-related leukocyte counts).
Infants (usually aged < 3 mo) have small storage pools of neutrophils. In severe infections, their neutrophilic demands often exceed their supplies. Therefore, young infants may have neutropenia in response to serious infection.
Table. Normal Leukocyte Counts (Open Table in a new window)
|
|
Total Leukocytes* |
|
Lymphocytes |
|
Neutrophils† |
|
Monocytes |
|
Eosinophils |
|||||||
Age |
|
Mean |
Range |
|
Mean |
Range |
% |
|
Mean |
Range |
% |
|
Mean |
% |
|
Mean |
% |
Birth |
|
... |
... |
|
4.2 |
2-7.3 |
... |
|
4 |
2-6 |
... |
|
0.6 |
... |
|
0.1 |
... |
12 h |
|
... |
... |
|
4.2 |
2-7.3 |
... |
|
11 |
7.8-14.5 |
... |
|
0.6 |
... |
|
0.1 |
... |
24 h |
|
... |
... |
|
4.2 |
2-7.3 |
... |
|
9 |
7-12 |
... |
|
0.6 |
... |
|
0.1 |
... |
1-4 wk |
|
... |
... |
|
5.6 |
2.9-9.1 |
... |
|
3.6 |
1.8-5.4 |
... |
|
0.7 |
... |
|
0.2 |
... |
6 mo |
|
11.9 |
6-17.5 |
|
7.3 |
4-13.5 |
61 |
|
3.8 |
1-8.5 |
32 |
|
0.6 |
5 |
|
0.3 |
3 |
1 y |
|
11.4 |
6-17.5 |
|
7.0 |
4-10.5 |
61 |
|
3.5 |
1.5-8.5 |
31 |
|
0.6 |
5 |
|
0.3 |
3 |
2 y |
|
10.6 |
6-17 |
|
6.3 |
3-9.5 |
59 |
|
3.5 |
1.5-8.5 |
33 |
|
0.5 |
5 |
|
0.3 |
3 |
4 y |
|
9.1 |
5.5-15.5 |
|
4.5 |
2-8 |
50 |
|
3.8 |
1.5-8.5 |
42 |
|
0.5 |
5 |
|
0.3 |
3 |
6 y |
|
8.5 |
5-14.5 |
|
3.5 |
1.5-7 |
42 |
|
4.3 |
1.5-8 |
51 |
|
0.4 |
5 |
|
0.2 |
3 |
8 y |
|
8.3 |
4.5-13.5 |
|
3.3 |
1.5-6.8 |
39 |
|
4.4 |
1.5-8 |
53 |
|
0.4 |
4 |
|
0.2 |
2 |
10 y |
|
8.1 |
4.5-13.5 |
|
3.1 |
1.5-6.5 |
38 |
|
4.4 |
1.8-8 |
54 |
|
0.4 |
4 |
|
0.2 |
2 |
16 y |
|
7.8 |
4.5-13 |
|
2.8 |
1.2-5.2 |
35 |
|
4.4 |
1.8-8 |
57 |
|
0.4 |
5 |
|
0.2 |
3 |
21 y |
|
7.4 |
4.5-11 |
|
2.5 |
1-4.8 |
34 |
|
4.4 |
1.8-7.7 |
59 |
|
0.3 |
4 |
|
0.2 |
3 |
* Numbers of leukocytes are in X 109/L or thousands per μL, ranges are estimates of 95% confidence limits, and percentages refer to differential counts. † Neutrophils include band cells at all ages and a small number of metamyelocytes and myelocytes in the first few days of life. |
|||||||||||||||||
-
WBC counts.