Background
Periventricular leukomalacia (PVL) is the most common ischemic brain injury in premature infants. [1] The ischemia occurs in the border zone at the end of arterial vascular distributions. The ischemia of periventricular white matter occurs in the to the lateral ventricles. The traditional diagnostic hallmarks of periventricular leukomalacia are periventricular echodensities or cysts detected by cranial ultrasonography, as shown below. Magnetic resonance imaging (MRI) studies have demonstrated a relatively common diffuse non-cystic form of periventricular leukomalacia in premature infants. Diagnosing this condition is important because a significant percentage of surviving premature infants may develop cerebral palsy (CP), intellectual impairment, or visual disturbances.
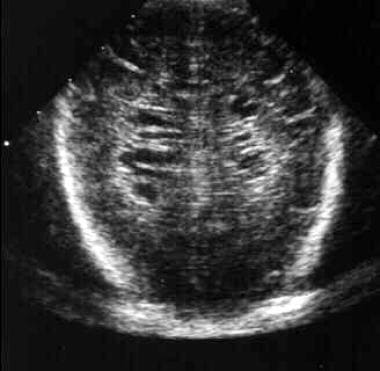 Pediatric Periventricular Leukomalacia. Cranial ultrasound, coronal view, in a 3-week-old premature infant. Multiple bilateral periventricular cysts are typical of this stage of periventricular leukomalacia (PVL). Courtesy of Matthew Omojola, MD.
Pediatric Periventricular Leukomalacia. Cranial ultrasound, coronal view, in a 3-week-old premature infant. Multiple bilateral periventricular cysts are typical of this stage of periventricular leukomalacia (PVL). Courtesy of Matthew Omojola, MD.
More recently, the term "periventricular leukomalacia (PVL)" has become fraught with controversy, as in clinical practice, it is labeled by neuroradiological findings and thus is a more neuropathological term. Unfortunately, careful correlations between neuropathological and neuroradiological assessments in preterm infants are generally unavailable and not likely to be carried out for numerous logistical reasons. Many experts suggest using the term cerebral "white matter injury" (WMI), under which PVL could be one category.
"Leukomalacia" is defined as necrosis of white matter, and not all echodensities in ultrasonography or high signal intensities on MRI are associated with necrosis on pathology. Some of these echodensities are due to excess of pre-oligodendrocytes and their maturational arrest (diffuse white matter gliosis). When necrosis is involved, the spectrum periventricular leukomalacia is described in three different levels: at the severe end, of large macroscopic focal necroses with the cystic changes; at the intermediate level, of small macroscopic focal necroses with focal gliosis but no cystic changes; and, at the least severe end, of microscopic focal necroses (with focal gliosis).
If a child is diagnosed with periventricular leukomalacia or white matter injury in the neonatal intensive care unit (NICU), it is very important that they be enrolled in early intervention programs. These children need close neurodevelopmental follow-up.
The image below represents the classification proposed by Volpe et al of cerebral white matter abnormalities in preterm infants by combining neuropathological and neuroradiological criteria and the possible spectrum of outcomes. [2]
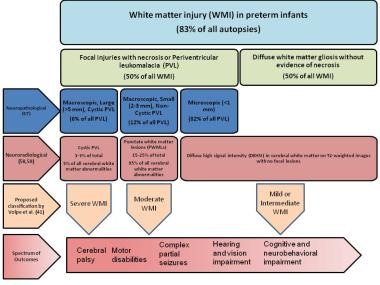 Pediatric Periventricular Leukomalacia. This image depicts cerebral white matter abnormalities in preterm infants found on neuropathological (autopsied) specimens correlating with neuroradiological findings on magnetic resonance images (MRIs) and outcomes. (Data extracted from references 2 Volpe, Pediatr Neurol, 2017], 9 [Volpe et al, Int J Dev Neurosci, 2011], 30 [Guo et al, Neurology, 2017], and 62 [Wagenaar et al, J Pediatr, 2017].)
Pediatric Periventricular Leukomalacia. This image depicts cerebral white matter abnormalities in preterm infants found on neuropathological (autopsied) specimens correlating with neuroradiological findings on magnetic resonance images (MRIs) and outcomes. (Data extracted from references 2 Volpe, Pediatr Neurol, 2017], 9 [Volpe et al, Int J Dev Neurosci, 2011], 30 [Guo et al, Neurology, 2017], and 62 [Wagenaar et al, J Pediatr, 2017].)
Pathophysiology
The pathophysiology of periventricular leukomalacia (PVL) is a complex process. This condition occurs because of ischemia-induced injury to oligodendrocytes in the periventricular area of the developing brain. Cytokine-induced damage following maternal or fetal infection may play a role.
Periventricular leukomalacia is a white matter lesion in premature infants that results from hypotension, ischemia, and coagulation necrosis at the border or watershed zones of deep penetrating arteries of the middle cerebral artery.
Several factors related to vascular development make the periventricular region of the preterm brain uniquely sensitive to ischemic injury. First, early in development, the deep penetrating arteries that supply the watershed zone of the periventricular white matter lack the vascular anastomoses that help maintain perfusion during periods of hypotension. As the fetus matures, the number of anastomoses between the deep penetrating arteries increases, and the periventricular white matter becomes less susceptible to small decreases in blood pressure.
The second vascular developmental factor that plays a role in periventricular leukomalacia is related to cerebral autoregulation. Premature infants have impaired cerebrovascular blood flow autoregulation, increasing their susceptibility to periventricular leukomalacia and intracranial hemorrhage (ICH). Decreased blood flow affects the white matter at the superolateral borders of the lateral ventricles. The site of injury affects the descending corticospinal tracts, visual radiations, and acoustic radiations.
Maternal infection, placental inflammation, and vasculitis are also important in the pathogenesis of periventricular leukomalacia. A link between maternal infection, preterm birth, and central nervous system (CNS) injury has been established by epidemiological studies. [3, 4] A role for infection and cytokine-induced injury in periventricular leukomalacia is strengthened by studies that demonstrate the presence of tumor necrosis factor in periventricular leukomalacia lesions [5] and in the cerebrospinal fluid (CSF) of infants with cerebral white matter injury. [6]
After the initial insult, either ischemia or inflammation, injury to the immature premyelinating oligodendrocytes occurs by either free radical attack or by excitotoxicity. The preterm infant is particularly sensitive to oxygen free radical attack because of delayed development of superoxide dismutase and catalase. [7]
Inomata et al suggested that combined elevations in serum levels of interleukin (IL) 6 and C-reactive protein (CRP) at birth are predictive of white matter injury in preterm infants with a fetal inflammatory response (FIR). [8]
Injury to the premyelinating oligodendrocytes results in astrogliosis and microgliosis. This results in a deficit of mature, myelin-producing oligodendrocytes, which leads to cerebral hypomyelination. [9]
Premature infants on mechanical ventilation may develop hypocarbia. Several studies have linked hypocarbia, particularly in the first few days of life, with the development of periventricular leukomalacia. [10, 11] Cumulative exposure during the first 7 days of life has been shown to independently increase the risk of periventricular leukomalacia in low birth weight infants. [12, 13]
Etiology
Mechanically ventilated premature infants born at less than 32 weeks' gestation are at greatest risk for periventricular leukomalacia (PVL).
Hypotension, hypoxemia, and acidosis may result in ischemic brain injury and periventricular leukomalacia.
Marked hypocarbia in ventilated premature infants has been associated with increased risk of developing periventricular leukomalacia.
Other associated risk factors include the following:
-
Placental vascular anastomoses, twin gestation, antepartum hemorrhage
-
Chorioamnionitis and funisitis
-
Sepsis
-
Maternal cocaine abuse
Risk factors for cystic periventricular leukomalacia in preterm infants younger than 35 weeks' gestation appear to be strongly associated with the following [14] :
-
Recurrent late deceleration on fetal heart rate monitoring
-
Loss of variability on fetal heart rate monitoring
-
Late-onset circulatory dysfunction
In addition, the cystic form may also occur with fetal acidosis related to recurrent late deceleration or loss of variability. [14]
Epidemiology
Although periventricular leukomalacia (PVL) is more common in preterm infants, it can occur in term infants as well. The incidence increases with decreasing gestational age and peaks at 24-32 gestational weeks. Although the incidence of the most severe cystic form of periventricular leukomalacia is falling, [15] a more subtle, diffuse form has emerged as the much more common lesion, possibly related to the increased survival of the smallest, most vulnerable infants. [16]
The worldwide overall incidence of periventricular leukomalacia ranges from 19.8% to 34.1%, and 2.5%–23% for the cystic form. Evidence of periventricular leukomalacia has been found in up to 75% of preterm infants and up to 20% in term infants in neuropathological studies during autopsy. [17, 18] Romero-Guzman and Lopez-Munoz described an incidence of white matter abnormalities in preterm infants by gestational age, estimated at 39.6% for infants born under 28 weeks' gestational age, 27.4% for those under 32 weeks' gestational age, and 7.3% for infants under 37 weeks' gestational age. [19] The lowest prevalence has been reported in Japan; in surviving preterm infants of gestational ages less than 33 weeks, the prevalence of periventricular leukomalacia was 2.7% (78/2883) on ultrasound diagnosis, and 3.3% (92/2824) on magnetic resonance imaging (MRI). [20]
Diffuse white matter abnormality on MRI is more commonly noted and increases as a function of postnatal age. Maalouf E et al described the evolution of diffuse MRI signal abnormality in premature infants in the United Kingdom (median gestational age: 27 weeks) increasing from 21% in the first postnatal week, to 53% over the next several weeks, and to 79% at term-equivalent age. [21] In a separate, later prospective study of 100 premature infants, 64 exhibited diffuse white matter signal abnormality at term. [22]
Male sex has been associated more with periventricular leukomalacia, [23] whereas race and ethnicity has no apparent impact on PVL. [24]
Prognosis
Periventricular leukomalacia (PVL) is a common neurological morbidity in preterm infants, and it is one of the most common causes of cerebral palsy in these infants.
Significant variation exists in clinical practice, and different protocols are used to diagnose periventricular leukomalacia; hence, associated outcomes are difficult to delineate (eg, periventricular leukomalacia diagnosed by ultrasonography vs magnetic resonance imaging [MRI]; diagnosis at early corrected gestational age vs at term corrected gestational age).
A very interesting study by Sarkar et al from the Neonatal Research Network showed that among 433 infants with recorded cystic periventricular leukomalacia in early ultrasonography (< 28 days of life), at closest to 36 weeks' gestation, 18% of cases “disappeared,” 20% persisted, and 62% had late cystic periventricular malacia (not detected early, but detected around 36 weeks). [25] Death or neurodevelopmental impairment (NDI) was more common in infants with disappeared cystic periventricular leukomalacia compared to those with no cystic periventricular leukomalacia (38 of 72 [53%] vs 1776 of 6376 [28%]). Disappeared, persistent, and late cystic periventricular leukomalacia were all also independently associated with poor neurodevelopmental outcomes. [25]
Moreover, the outcomes of periventricular leukomalacia depend on the quantitative involvement of white matter and its location/extent. The most common outcomes occurring as a consequence of this condition include the following:
Motor disabilities/cerebral palsy
Motor disability is the most common outcome for severe forms of periventricular leukomalacia (cystic/focal lesions) as compared to subtle forms of neurodevelopmental impairment or neuropsychiatric disorders associated with diffuse periventricular leukomalacia. Cystic periventricular leukomalacia changes affect deep and medial fiber tracts that control lower extremity functions, leading to spastic diplegia. If more lateral fibers are affected, upper extremity function can also be impaired. Extensive white matter involvement may result in quadriplegia. [18]
A meta-analysis by Gotargo et al showed that periventricular leukomalacia was associated with cerebral palsy, both in its cystic and non-cystic form. [26] The presentation of clinical features as a consequence of periventricular leukomalacia evolves with time. In the early phase of changes of the disease, infants may have low tone and poor head control, apnea, bradycardia, irritability, and poor feeding. After several weeks, characteristic features of spastic diplegia (ie, increased tone, brisk deep tendon reflex, scissoring of lower extremities, contractures, and abnormal gross and fine motor incoordination) may be seen. [27]
Cognitive or neurobehavioral impairment
If repeated ultrasonography shows only increased periventricular echogenicity without cysts, less than 5% of these infants will subsequently develop overt cerebral palsy, although substantially more of them will show evidence of cognitive dysfunction. [28] Injury to white matter association fibers may result in intellectual impairment and learning difficulties, such as visuomotor and perceptual disabilities, constructional dyspraxia, or attention-deficit disorders. One study also reported a reduction in performance intelligence quotients but not verbal intelligence quotients in children who had periventricular leukomalacia. [29] Punctate white matter lesions in the territory of the frontal lobes are associated with clinically significant adverse motor and cognitive outcomes at 18 months in very preterm neonates. [30]
In a retrospective study (2006-2015) that assessed the influence of severe peri-intraventricular hemorrhage, with or without cystic periventricular leukomalacia, on mortality and neurodevelopment of 99 Portugese newborns at age 24 months, Amaral et al found severe peri-intraventricular hemorrhage was associated with higher mortality and neurodevelopment impairment in preterm infants, particularly in those with cystic periventricular leukomalacia. [31]
Complex partial seizures
The incidence of complex partial seizures is much higher in infants with ultrasonically demonstrable cystic lesions relative to those with non-cystic lesions.
Cerebral visual/hearing impairment
Cerebral visual/hearing impairment is an important sequela of periventricular leukomalacia and can be predicted with abnormalities within the optic radiation as seen on MRI. [32] When comparing children with cystic periventricular leukomalacia and those without periventricular leukomalacia, Gotargo et al found that there is an increased risk of hearing impairment and visual impairment. [26]
-
Pediatric Periventricular Leukomalacia. Cranial ultrasound, coronal view, in a 1-week-old premature infant. The periventricular echotexture is abnormally increased (greater than or equal to that of the choroid plexus), which is consistent with the early changes of periventricular leukomalacia (PVL). Courtesy of Matthew Omojola, MD.
-
Pediatric Periventricular Leukomalacia. Cranial ultrasound, coronal view, in a 1-week-old premature infant without periventricular leukomalacia (PVL). The periventricular echotexture is normal. Compare this image with the previous image. Courtesy of Matthew Omojola, MD.
-
Pediatric Periventricular Leukomalacia. Cranial ultrasound, coronal view, in a 3-week-old premature infant. Multiple bilateral periventricular cysts are typical of this stage of periventricular leukomalacia (PVL). Courtesy of Matthew Omojola, MD.
-
Pediatric Periventricular Leukomalacia. Cranial ultrasound, sagittal view, in a 3-week-old premature infant. Multiple periventricular cysts are typical of this stage of periventricular leukomalacia (PVL). Courtesy of Matthew Omojola, MD.
-
Pediatric Periventricular Leukomalacia. Cranial computed tomography (CT) scan, axial image, in a 5-week-old premature infant with periventricular leukomalacia (PVL). The ventricular margins are irregular, which is consistent with incorporation of the periventricular cysts of PVL. Mild ventriculomegaly and loss of the periventricular white matter is observed. Courtesy of Matthew Omojola, MD.
-
Pediatric Periventricular Leukomalacia. Cranial computed tomography (CT) scan, axial image, in a 14-month-old child with periventricular leukomalacia (PVL). Ventriculomegaly is limited to the lateral ventricles secondary to diffuse loss of periventricular white matter. Courtesy of Matthew Omojola, MD.
-
Pediatric Periventricular Leukomalacia. Cranial magnetic resonance image (MRI), T1-weighted axial image, in an 18-month-old with periventricular leukomalacia (PVL). The lateral ventricles are enlarged without hydrocephalus. The periventricular white matter is diminished. Courtesy of Matthew Omojola, MD.
-
Pediatric Periventricular Leukomalacia. Cranial magnetic resonance image (MRI), T2-weighted axial image, in an 18-month-old with periventricular leukomalacia (PVL). Again, enlarged ventricles and loss of white matter are demonstrated. Also noted is the abnormal increased signal in the periventricular regions on this T2-weighted image. Courtesy of Matthew Omojola, MD.
-
Pediatric Periventricular Leukomalacia. Cranial magnetic resonance image (MRI), sagittal T1-weighted image in the midline, in an 18-month-old child with periventricular leukomalacia (PVL). Hypoplasia of the corpus callosum is present and is most evident, involving the body. Courtesy of Matthew Omojola, MD.
-
Pediatric Periventricular Leukomalacia. This image depicts cerebral white matter abnormalities in preterm infants found on neuropathological (autopsied) specimens correlating with neuroradiological findings on magnetic resonance images (MRIs) and outcomes. (Data extracted from references 2 Volpe, Pediatr Neurol, 2017], 9 [Volpe et al, Int J Dev Neurosci, 2011], 30 [Guo et al, Neurology, 2017], and 62 [Wagenaar et al, J Pediatr, 2017].)

