Practice Essentials
Patent foramen ovale (PFO) is a flaplike opening between the atrial septa primum and secundum at the location of the fossa ovalis (see the image below) that persists after age 1 year. With increasing evidence being found that PFO is the culprit in paradoxical embolic events, the relative importance of the anomaly is being reevaluated.
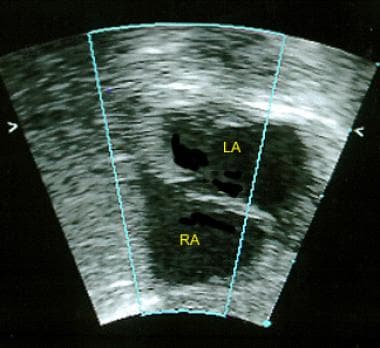 This 2-dimensional echocardiogram in an infant (subcostal long-axis view) shows a patent foramen ovale. Right atrium (RA) and left atrium (LA
This 2-dimensional echocardiogram in an infant (subcostal long-axis view) shows a patent foramen ovale. Right atrium (RA) and left atrium (LA
Signs and symptoms
Most patients with isolated PFO are asymptomatic. Possible of the signs and symptoms can include:
-
History of stroke or transient ischemic event of undefined etiology
-
Migraine or migraine-like symptoms - Whether symptoms are due to transient ischemic attacks or paradoxical embolism is not clear
-
Neurologic decompression sickness - Seen with PFO in a small percent of scuba divers
Other, less common clinical manifestations of PFO include the following:
-
Acute myocardial infarction
-
Systemic embolism, such as renal infarction
-
Fat embolism
-
Paradoxical embolism caused by right atrial tumors that increase right atrial pressure
-
Left-sided valve disease in carcinoid syndrome
See Presentation for more detail.
Diagnosis
The following types of echocardiography can be used in the detection of PFO:
-
Color flow Doppler imaging: A small "flame" of color signal may be seen in the middle region of the atrial septum
-
Contrast echocardiography: Usually required to detect a small PFO
-
Two-dimensional transesophageal echocardiography (2-D TEE) with contrast medium: Provides superior visualization of the atrial septum
-
Three-dimensional transesophageal echocardiography (3-D TEE): Provides direct visualization of the entire PFO anatomy and surrounding structures
-
Transmitral Doppler (TMD) echocardiography: Relatively limited evidence is available for the role of TMD. This modality measures blood flow across the mitral valve with the aid of a contrast medium
-
Transcranial Doppler (TCD): An alternative to TEE; however, although it can detect a right-to-left shunt, it cannot show the shunt’s location [1]
See Workup for more detail.
Management
PFO is an incidental finding in most patients. It requires no treatment or follow-up.
When PFO is associated with an otherwise unexplained neurologic event, traditional treatment has been antiplatelet (ie, aspirin) therapy alone in low-risk patients. However, it can be combined with anticoagulant in high-risk individuals to prevent cryptogenic stroke. A number of clinical trials have shown PFO closure is more effective than antiplatelet therapy. [2, 3, 4, 5, 6]
Background
Patent foramen ovale (PFO) is an anatomic interatrial communication with potential for right-to-left shunt. Foramen ovale has been known since the time of Galen. In 1564, Leonardi Botali, an Italian surgeon, was the first to describe the presence of foramen ovale at birth. However, the function of foramen ovale in utero was not known at that time. In 1877, Cohnheim described paradoxical embolism in relation to PFO.
PFO is not atrial septal defect because no septal tissue is missing.
See also the Medscape Drugs & Disease articles Atrial Septal Defect and Pediatric Atrial Septal Defects.
Pathophysiology
Patent foramen ovale (PFO) is a flaplike opening between the atrial septa primum and secundum at the location of the fossa ovalis that persists after age 1 year. In utero, the foramen ovale serves as a physiologic conduit for right-to-left shunting. Once the pulmonary circulation is established after birth, left atrial pressure increases, allowing functional closure of the foramen ovale. This is followed by anatomical closure of the septum primum and septum secundum by the age of 1 year.
The Mayo Clinic autopsy study revealed that the size of a PFO increases from a mean of 3.4 mm in the first decade to 5.8 mm in the 10th decade of life, as the valve of fossa ovalis stretches with age. [7]
With increasing evidence that PFO is the culprit in paradoxical embolic events, the relative importance of the anomaly is being reevaluated. James Lock, MD, postulated that PFO anatomy results in a cul-de-sac between the septa primum and secundum, predisposing individuals to hemostasis and clot formation. Any conditions that increase right atrial pressure more than left atrial pressure can induce paradoxical flow and may result in an embolic event.
This reasoning has greatly altered the previous conception of PFO and has changed management of the condition.
Epidemiology
United States statistics
Patent foramen ovale (PFO) is detected in 10-15% of the population by contrast transthoracic echocardiography. Autopsy studies show a 27% prevalence of probe-patent foramen ovale. [7] This difference is probably due to the ability to directly visualize PFO on autopsy study, while contrast echocardiography relies on detection of secondary physiologic phenomena.
Sex- and age-related demographics
The prevalence and size of probe-patent PFO is similar in males and females.
The prevalence of PFO declines progressively with age—34% up to age 30 years, 25% for age 30-80 years, and 20% older than 80 years.
-
This 2-dimensional echocardiogram in an infant (subcostal long-axis view) shows a patent foramen ovale. Right atrium (RA) and left atrium (LA
-
Color Doppler of the patent foramen ovale (PFO) seen in the previous image. A small amount of left-to-right flow is present. This left-to-right flow pattern is typical for PFO seen in newborn infants
-
Color Doppler of the patent foramen ovale (PFO) seen in the previous image. A small amount of left-to-right flow is present. This left-to-right flow pattern is typical for PFO seen in newborn infants





