Surface Anatomy
The forehead region constitutes the upper third of the face, delineated superiorly by the hairline and inferiorly by the glabella and frontonasal groove (centrally) and the eyebrows overlying the supraorbital ridges (laterally). It plays a significant role in facial expressions and aesthetics. [1] The hairline is not a stable landmark in individuals; factors such as sex, age, familial characteristics, and the influence of culture and fashion decide the position of the hairline for individuals.
Surgery in the upper third of the face, whether reconstructive or cosmetic, is considered to involve at least one of three regions: the central forehead, the hair-bearing scalp, and the temporal regions. Anatomy must be reviewed in the context of the eyebrow-forehead-temple continuum.
Although the hairline defines the anatomic boundary between the forehead and the scalp, consideration must be given to the anticipated patterns of androgenetic alopecia (baldness) in the future because scars may be exposed with a receding hairline.
Detailed analysis has revealed multiple layers within the forehead region — skin, subcutaneous fat layers, fasciae (including suprafrontalis), and underlying muscles (e.g., frontalis). This layered structure is critical in the development of new treatment strategies for cosmetic interventions with soft tissue augmentation or neuromodulators. [2]
Studies using three-dimensional imaging have shown how skin displacement occurs during frontalis muscle contraction. Understanding these displacement patterns helps with surgical techniques aimed at reducing rhytides (wrinkles) or enhancing aesthetic outcomes. [3]
Research indicates that forehead morphology varies significantly based on sex and age. For instance, males typically exhibit a straighter and more protruding forehead profile than females. This morphological understanding aids in assessing facial aesthetics and potential surgical outcomes. [4]
The density of eyebrow hair generally remains stable with age, although it may frequently be altered in appearance by plucking or tattooing. Eyebrow position, contour, and movement are key features of facial expression. The medial eyebrow hairs are almost vertical in orientation, while they become more horizontal laterally. The eyebrow forms an arc laterally, with the peak at the junction of the medial two thirds and the lateral third. The brow is straighter and thicker in males, being at the level of the superior orbital rim; it is more arched, thinner, and higher in females.
The superior orbital margin forms a well-marked prominence that may be palpated along its length. It frequently presents the supraorbital notch, which can be felt at the junction of the medial third and lateral two thirds.
The Latin root of the word glabella means hairless and smooth, and the glabella is such in youth; however, glabellar transverse and vertical rhytides are common with age. Superiorly, between the eyebrows and the hairline, smoothness gives way to horizontal forehead rhytides with age. Studies emphasize the importance of the forehead and temple musculature, particularly the action of the frontalis muscle, which contributes to forehead movement and horizontal rhytides that intensify over time. Rhytides can be considered for scar camouflage in surgery.
The curved arc of the temporal line is palpable at the lateral limits of the forehead and is made more apparent with the action of the temporalis muscle with mastication. The superficial temporal artery (STA) is generally palpable in the temple, which is important in the consideration of a temporal artery biopsy and when local vascularized flaps are planned. The lateral orbital margin is visible and palpable in its extent, and the frontozygomatic suture frequently may be felt as a small depression approximately 10 mm superior to the lateral canthus. The superior margin of the zygomatic arch is generally palpable, extending between the lateral orbital rim and the anterior border of the tragus.
The course of the frontal branch of the facial nerve passes through the temple and forehead, placing this nerve at risk for injury at the time of surgical dissection. The usual trajectory of the nerve is from a point 5 mm below the tragus to a point 15 mm above the lateral extremity of the brow. Over the zygomatic arch, it is situated halfway between the lateral canthus and the inferior helix. This places it about 2.5 cm lateral to the lateral canthus.
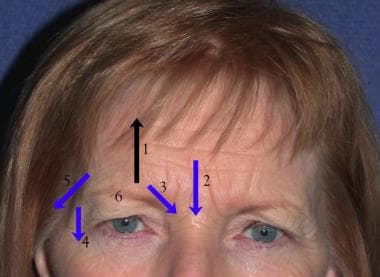
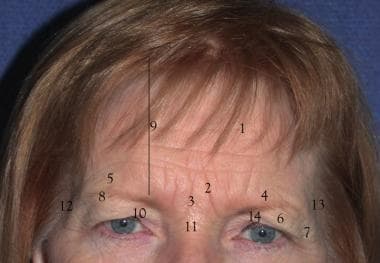 1. Forehead rhytids 2. Corrugator rhytids 3. Procerus rhytids 4. Brow ptosis 5. Brow symmetry/asymmetry 6. Secondary dermatochalasis 7. Crow’s feet 8. Brow fat pad volume and position 9. Forehead height 10. Ptosis 11. “Fat nose” 12. Lateral droop and slide 13. Temporal rhytids and temporal hollowing
1. Forehead rhytids 2. Corrugator rhytids 3. Procerus rhytids 4. Brow ptosis 5. Brow symmetry/asymmetry 6. Secondary dermatochalasis 7. Crow’s feet 8. Brow fat pad volume and position 9. Forehead height 10. Ptosis 11. “Fat nose” 12. Lateral droop and slide 13. Temporal rhytids and temporal hollowing
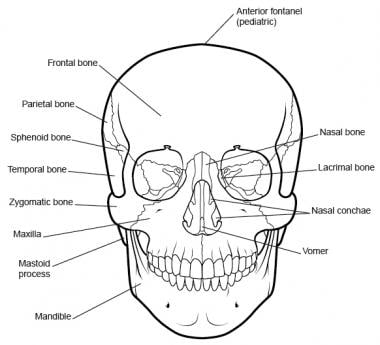
Bones of the Forehead
The bones of the forehead form the scaffold on which the soft tissues are draped. The frontal bone presents an anterior surface that is convex anteriorly (see the image below). It articulates with (1) the parietal bones posteriorly at the coronal suture, (2) the nasal bones and the frontal process of the maxilla anteriorly and medially, (3) the frontal process of the zygoma at the frontozygomatic suture laterally, and (4) within the temporal fossa, with the greater wing of the sphenoid. The frontal bone also presents an orbital surface and an intracranial surface that is not discussed in this article.
The superciliary ridges are prominences of the frontal bone above the orbital margins that meet in the midline in the glabella. They are significantly more prominent in males. The superior orbital rim presents a supraorbital notch or foramen through which courses the supraorbital neurovascular bundle. Bilateral notches are present in 58.33% of the skulls, while bilateral foramina occur in about 18.34%, and one notch on one side and one foramen on the contralateral side in 23.3%. [5]
The temporal crest runs from the zygomatic process of the frontal bone superiorly and posteriorly to become continuous with the temporal line on the parietal bone.
The mean calvarial thickness is 6.8-7.7 mm, which can be safely drilled to a depth of 3-4 mm. The bone is thicker in females than in males and is thickest in the parietal bone behind the coronal suture; the superotemporal site is thinnest, with a thickness of 4.71-6.14 mm. Drilling in the midline should be avoided, keeping in mind the location of the sagittal sinus. [6]
Forehead and Scalp
Skin
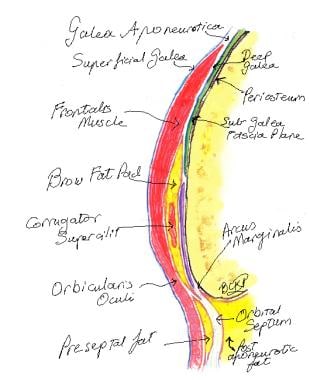
The scalp is traditionally considered in five layers: skin, subcutaneous tissue, galea aponeurotica, loose areolar tissue, and periosteum. These layers continue into the forehead, where the galea gives way to the muscles of facial expression in the region of the eyebrow.
The skin of the forehead is the thickest facial skin and is rich in sebaceous glands and sweat glands.
The forehead has a layered structure, comprising the epidermis, dermis, a superficial fatty layer, and deeper muscular components. The presence of various fat pads — specifically the central forehead fat pad and the lateral temporal fat pad — contributes to the overall contour and aesthetic appearance of this area. [7]
Subcutaneous tissue
Richly vascularized, the subcutaneous tissue contains a homogenous layer of adipose tissue. Numerous transverse fibrous septa from the frontalis muscle to the dermis are found within this layer in the forehead. These septa are partially responsible for the deep, transverse forehead rhytides.
Muscles and aponeurosis of the forehead
The muscular layer of the eyebrow is below the subcutaneous tissue. This layer is composed of the elevator muscle (frontalis) and the depressor muscles (procerus, corrugator supercilii, orbital portion of the orbicularis oculi) (see the image below). Studies reveal a continuous fatty layer beneath the frontalis muscle, which includes various fat compartments such as preseptal fat in the upper eyelid and retro-orbicularis fat deep to the orbicularis oculi muscle. This layered arrangement enhances our understanding of how these structures interact during surgical procedures and aesthetic treatments. [8]
These muscles are essential for facial expressions, often contracting in response to emotions, and are innervated by the temporal branch of the facial nerve (cranial nerve VII). Additionally, sensory innervation comes from branches of the trigeminal nerve (cranial nerve V), specifically the supraorbital and supratrochlear nerves. These nerves provide tactile feedback, contributing to the forehead's sensory and protective functions. [1, 9]
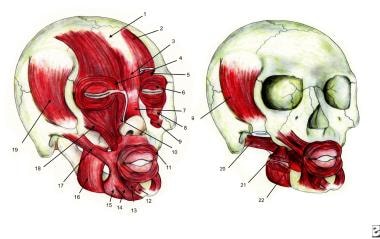 Facial muscles: 1. Galea aponeurotica 2. Frontalis 3. Procerus 4. Depressor supercilii 5. Corrugator supercilii 6. Orbicularis oculi 7. Nasalis 8. Levator labii superioris 9. Levator anguli oris 10. Levator labii superioris alaeque nasi 11. Orbicularis oris 12. Mentalis 13. Depressor labii inferioris 14. Depressor anguli oris 15. Platysma 16. Masseter 17. Zygomaticus major 18. Zygomaticus minor 19. Temporalis 20. Lateral pterygoid 21. Medial pterygoid 22. Buccinator
Facial muscles: 1. Galea aponeurotica 2. Frontalis 3. Procerus 4. Depressor supercilii 5. Corrugator supercilii 6. Orbicularis oculi 7. Nasalis 8. Levator labii superioris 9. Levator anguli oris 10. Levator labii superioris alaeque nasi 11. Orbicularis oris 12. Mentalis 13. Depressor labii inferioris 14. Depressor anguli oris 15. Platysma 16. Masseter 17. Zygomaticus major 18. Zygomaticus minor 19. Temporalis 20. Lateral pterygoid 21. Medial pterygoid 22. Buccinator
Frontalis muscle
The paired frontalis muscles are the primary elevators of the brow. The vertically orientated muscle fibers offer no true bony insertion but blend with the brow depressor muscles, which do have bony insertions (the procerus medially, the corrugator and orbicularis oculi centrally, the orbicularis oculi laterally). Deep to the frontalis muscle, a potential space that allows movement of the frontalis over the periosteum is found. The frontalis also has multiple attachments to the dermis of the forehead skin, causing transverse forehead creases. Innervation is by the frontal branch of the facial nerve.
The frontalis is continued posteriorly by the large, thin epicranial aponeurosis (galea aponeurotica). The galea aponeurotica encloses the frontalis muscle with a thin, superficial layer over the muscle and a deeper, well-defined layer beneath the muscle. This deeper layer is firmly attached to the supraorbital margin, contributing to the arcus marginalis. Laterally, the galea conceptually continues as the superficial temporal fascia (STF). Posteriorly, the galea continues as the occipitalis muscle. The two bellies of the occipitalis take their origin from the periosteum and bone of the superior nuchal line of the mastoid portion of the temporal bone and insert into the galea aponeurotica. Innervation is by the posterior auricular branch of the facial nerve.
The superficial musculoaponeurotic system (SMAS), which includes structures such as the galea aponeurotica, plays a critical role in maintaining facial contours and may be involved in surgical considerations for aesthetic procedures such as brow lifts. [10]
Corrugator superciliaris muscle
The paired corrugator superciliaris muscles arise from the frontal bone near the superomedial orbital rim, anteriorly and slightly cephalad to the trochlea. The muscle runs superolaterally through the fibers of orbicularis oculi and frontalis before inserting into the medial eyebrow skin. The corrugator muscle is a brow depressor, pulling the brow medially and inferiorly, producing vertical glabellar folds. Innervation is from the terminal branches of the frontal branch of the facial nerve.
Its vascular supply is derived from branches of the superficial temporal and ophthalmic arteries. Venous drainage occurs through the superior ophthalmic vein, which connects to the cavernous sinus. Nerve supply is through the temporal branches of the facial nerve. Clinically, the corrugator supercilii is a target in aesthetic treatments such as botulinum toxin injections, which can reduce glabellar lines or treat migraines by inhibiting muscular contraction. [1, 11]
Procerus muscle
The flat, thin procerus muscle originates at the nasal bone and inserts into the glabella and lower midforehead. It lies between the paired frontalis muscles. The procerus is a brow depressor, forming horizontal nasal root creases.
The facial nerve (CN VII) innervates the majority of muscles responsible for facial expression, specifically, the procerus is innervated by the temporal and zygomatic branches of CN VII. Blood supply to the procerus comes from branches of the facial artery, including both angular and lateral nasal branches. The primary action of the procerus muscle is to depress the medial ends of the eyebrows which may create rhytides in the glabellar region. This action is particularly noticeable when a person frowns or squints, often in response to bright light or emotional stimuli. [1, 12]
The procerus muscle's activity can lead to static rhytide formation in overlying skin of the glabellar area due to repetitive contraction over time. Consequently, it is often targeted in cosmetic procedures involving neuromodulators (botulinum toxin) injections to reduce muscle contraction, thereby decreasing dynamic rhytides and preventing static rhytide formation. Studies have shown that understanding its anatomy is vital for effective injection techniques as improper placement can lead to complications or ineffective results. [13]
In some cases, abnormalities in the procerus or related muscles may result in conditions such as blepharospasm, which affects the eyelid movement and may require treatment to alleviate involuntary muscle contractions. [14]
Orbicularis oculi muscle
The orbicularis oculi muscle should be considered a muscle of the eyelid rather than that of the brow; however, the orbital portion extends in a wide, circular fashion around the orbit, interdigitating with muscles of facial expression of the brow. It has a curved origin from the medial orbital margin, being attached to the superomedial orbital margin, maxillary process of the frontal bone, medial palpebral ligament, frontal process of the maxilla, and inferomedial orbital margin. Fibers from the medial origin sweep around the orbital margin in a horseshoe fashion. The muscle fibers extend superiorly to intermix with the frontalis and corrugator supercilii muscles and laterally to cover the STF.
Functionally, the orbital portion of the muscle is used in forced eyelid closure and hence acts as a brow depressor. The superomedial portion of each orbicularis muscle is also referred to as the depressor supercilii muscle. Innervation is from branches of the facial nerve. The nerves are horizontally orientated and innervate the muscle from the undersurface.
Anatomic dissection reveals a distinct layer of fibroadipose tissue posterior to the orbicularis oculi and frontalis muscles, termed the retro-orbicularis oculi fat (ROOF). ROOF is analogous to the suborbicularis oculi fat (SOOF) of the lower eyelid. The ROOF frequently continues inferiorly over the superior orbital rim to overlie the orbital septum. The function of this tissue may be to enhance eyebrow mobility.
Research has characterized the orbicularis oculi muscles as those that are more similar to quadriceps than extraocular muscles in terms of excitation-contraction coupling. These muscles do not express the cardiac isoform of the dihydropyridine receptor typical in extraocular muscles, suggesting unique physiologic properties that may influence their function in facial expressions and eyelid movements. [15]
A detailed examination of the muscular-deep fascial system between the eyebrow and superior orbital margin has uncovered intricate connections between the frontalis and orbicularis oculi muscles. The frontalis muscle partially overlaps with the upper orbital part of the orbicularis oculi, indicating a complex interplay that may affect eyebrow positioning and movement. [16]
Investigations into age-related changes have shown that the thickness of the orbicularis oculi varies significantly across different age groups, with younger individuals exhibiting greater muscle thickness. This change may correlate with a functional decline in eyelid closure and overall facial aesthetics as individuals age. [17]
Loose areolar tissue
The subgaleal space is used as a plane of dissection in forehead surgery. Connective tissue lies between the galea and the periosteum, which can be easily divided with a semisharp dissector. At the supraorbital margin, the space is traversed by the supraorbital and supratrochlear neurovascular bundles.
The subgaleal space itself is largely avascular, but it receives blood supply peripherally from perforating branches of all the major scalp vessels which thereby source the galea aponeurotica and the periosteum. Subgaleal dissection for a forehead lift may remove one source of blood to a raised forehead flap. Subperiosteal dissection raises the subgaleal tissue with the forehead flap to preserve this source of blood supply.
Pericranium
The pericranium lies adherent to the bone but can be readily elevated to give a relatively avascular subperiosteal space, suitable for the optical cavity required in endoscopic brow lifting. Anteriorly, the pericranium continues into the orbit as the periorbita. Along the supraorbital rim, the periosteum fuses with the orbital septum at the arcus marginalis.
Sullivan et al showed the presence of the following three retaining ligaments: [18]
-
Inferomedial - 12 mm lateral to the midline at the superior orbital rim
-
Superomedial - 13 mm lateral to the midline and 10 mm above the superior orbital rim
-
Superotemporal - 23 mm lateral to the midline and 10 mm above the rim
 1. Frontalis muscle 2. Brow fat pad 3. Orbital orbicularis muscle 4. Procerus muscle 5. Depressor supercilii 6. Corrugator muscle 7. Supratrochlear nerve 8. Supraorbital nerve 9. Medial branch of the supraorbital nerve (Superficial branch) 10. Lateral branch of the supraorbital nerve (deep branch) 11. Temporal fusion line 12. Conjoint tendon 13. Frontal branch of the facial nerve 14. Orbital orbicularis at the temporal raphe causing crow’s feet
1. Frontalis muscle 2. Brow fat pad 3. Orbital orbicularis muscle 4. Procerus muscle 5. Depressor supercilii 6. Corrugator muscle 7. Supratrochlear nerve 8. Supraorbital nerve 9. Medial branch of the supraorbital nerve (Superficial branch) 10. Lateral branch of the supraorbital nerve (deep branch) 11. Temporal fusion line 12. Conjoint tendon 13. Frontal branch of the facial nerve 14. Orbital orbicularis at the temporal raphe causing crow’s feet
These ligaments play a crucial role in maintaining facial structure and stability. They act as anchor points, stabilizing the skin and superficial fascia (SMAS) to deeper structures, which is essential for achieving desired aesthetic outcomes while minimizing nerve injury during surgical dissection. Literature suggests that these retaining ligaments do not undergo significant age-related changes, indicating their importance in facial rejuvenation techniques. Studies indicated that preserving these ligaments during facelift procedures enhances surgical results and patient satisfaction by maintaining facial contours and reducing complications associated with soft tissue laxity. [19]
Supraorbital and Supratrochlear Nerves
Sensory innervation of the forehead and anterior scalp is supplied by the supraorbital and supratrochlear nerves, being branches of the ophthalmic division of the trigeminal nerve.
The supraorbital nerve and vessels emerge from the supraorbital foramen or notch and continue superiorly. Near this exit, the supraorbital nerve trunk divides into a deep and a superficial branch. The deep branch courses superolaterally, running parallel and 0.5-1.5 cm medial to the superior temporal line of the skull in the loose areolar tissue between the galea and the pericranium.
The terminal branches of this deep supraorbital nerve branch pierce the galea near the coronal suture to provide scalp sensation to the frontoparietal region. The superficial division lies medially at its origin and quickly divides into multiple branches that pierce the frontalis muscle. These smaller branches pass cephalad to supply the forehead and up to 3.5 cm of the frontal scalp. The supraorbital nerve also supplies the upper eyelid sensation by small eyelid branches.
Supratrochlear nerves exit the orbit at the superior orbital rim through a notch, above the trochlea and medial to the supraorbital notch. Most skulls (97%) possess bilateral supratrochlear notches; however, 1% possess bilateral foramina and 2% have a notch on one side and a foramen on the other.
At the supraorbital rim, the nerves penetrate the corrugator muscle and the frontalis muscle toward the skin and may be damaged here during corrugator resection. The nerves supply cutaneous sensation to a central vertical strip of the forehead and to the medial upper eyelid. The supraorbital notch is a palpable landmark in the medial third of the brow used for performing local nerve blocks with injectable anesthetic for procedures on the forehead.
Anatomical studies have further elucidated variations in these nerves' courses and branching patterns. A study reported two main variants in how these nerves branch from the frontal nerve within the orbit:
-
Variant I (42% of the cases) - The supraorbital and supratrochlear nerves branch off from the frontal nerve in its distal half.
-
Variant II (58% of the cases) - The branching occurs in the proximal half, characterized by a thicker supraorbital nerve and a thinner supratrochlear nerve.
Additionally, dissections reveal that both nerves show significant anatomical variability in their exit points from the orbit, with average distances from midline measuring approximately 26.5 mm for the supraorbital nerve and 21 mm for the supratrochlear nerve at their respective exit points. This variability is crucial for surgical planning, especially in procedures involving neurotization or interventions targeting migraine treatment. [20, 21]
The Temporal Region
The tissue layers in the temporal region are the skin, subcutaneous fat, STF, deep temporal fascia (DTF), and temporal muscle. A problem in the discussion of anatomy in this region is the variable nomenclature used for the various fascial layers and fat pads.
For surgeons, the important features in the temple region include the frontal branch of the facial nerve and the superficial temporal artery.
The skin and subcutaneous tissues continue from the scalp and forehead, with a variable degree of hair-bearing skin in the temples.
The STF represents the continuance of the SMAS of the face and the galea aponeurotica system of the scalp. This multilaminated fascial layer is loosely adherent to the subdermal fat and is intimately associated with the frontal branch of the facial nerve and the superficial temporal vessels. It is also called the temporoparietal fascia.
A loose areolar plane, termed the subaponeurotic plane, separates the STF from the DTF and is the plane of dissection commonly used when operating in the temporal region. It allows dissection to be performed directly on the surface of the DTF. This plane is relatively avascular, but 2-3 perforating veins are frequently sentinels to the approaching zygomatic arch. The one (or sometimes two) sentinel vein present lateral to the orbital rim bears a fairly constant relationship to the bony landmarks. [22] The temporal division of the facial nerve is usually found cephalad to the sentinel vein.
The DTF is a thick, dense connective tissue layer overlying the temporalis muscle. It has a firm attachment to the superior temporal line. Several centimeters above the zygomatic arch, the DTF splits into a superficial layer and a deep layer. The superficial layer of the DTF attaches to the superficial superior margin of the zygomatic arch. The deep layer of the DTF attaches to the deep superior margin of the zygomatic arch.
Enveloped between the two layers of the DTF lies the superficial temporal fat pad. This vascular adipose deposit is supplied by the middle temporal artery. Deep to the deep layer of the DTF lies the deep temporal fat pad, which represents a superior extension of the buccal fat pad. This extension passes superiorly deep to the zygomatic arch, to lie between the deep layer of the DTF and the temporalis muscle proper.
Along the anterior limits of the superior temporal line, the STF and the galea aponeurotica fuse with the DTF and the central forehead periosteum to form a conjoint fascia. Dissection of the fascial layers in this region requires sharp dissection. [23]
Superficial temporal artery
The STA is a terminal branch of the external carotid artery. Its origin lies within the parotid gland, and it ascends to cross the zygomatic arch about 10 mm anterior to the tragus. Above the arch, the vessel is invested within the STF. The average diameter of the STA has been reported to be around 1.5 mm.
Upon reaching the temporal region, the STA bifurcates into two primary terminal branches: the anterior (frontal) branch and the posterior (parietal) branch. The anterior branch supplies the pericranium and skin of the lateral frontal area, while the posterior branch supplies the parietal area of the scalp. Additionally, several other branches arise from the STA, including [24] :
-
Transverse facial artery
-
Middle temporal artery
-
Parietal branch
-
Frontal branch
-
Zygomatico-orbital artery
-
Anterior auricular branch
The transverse facial artery runs parallel to the zygomatic process and supplies various facial structures, including parts of the parotid gland and masseter muscle. The zygomatico-orbital artery, which is present in approximately 85% of the cases, often bifurcates from the frontal branch of the STA and follows a path along a line connecting the tragus to the superciliary arch. [24, 25]
Studies emphasize anatomical variations in the STA's course and branching patterns. For instance, a meta-analysis revealed that in about 79% of the cases, bifurcation occurs above the zygomatic arch. Furthermore, variations in branching can influence surgical approaches and aesthetic procedures in this region, highlighting its clinical significance. [26]
Additionally, the STA's proximity to the temporalis muscle and its role in providing collateral blood flow make it a valuable artery for bypass surgeries, especially in conditions such as Moyamoya disease or middle cerebral artery insufficiency. The artery’s superficial location allows easy access for such interventions, and its layered structure — comprising the intima, media, and adventitia — supports its flexibility in various reconstructive surgeries. [27]
Frontal branch of the facial nerve
The frontal branch of the facial nerve supplies motor innervation to the muscles of facial expression of the eyebrows and forehead. It courses within the STF, traveling within its deep surface. The course of the nerve places it at risk for injury at the time of surgical dissection over the zygomatic arch and in the temple and forehead. Its usual trajectory is from a point 5 mm below the tragus to a point 15 mm above the lateral extremity of the brow. Over the zygomatic arch, it is found about 2.5 cm lateral to the lateral canthus, placing it halfway between the lateral canthus and the inferior helix. [28, 29]
A study examined the depth transitions of the frontal branch relative to the zygomatic arch. It was found that in 94.4% of the dissected specimens, the frontal branch transitioned to an intra-SMAS plane approximately 9.6 mm above the zygomatic arch, with all specimens showing this transition about 12.2 mm posterior to Pitanguy's line. This research highlights a surgical "caution zone" intended to minimize intraoperative nerve injuries during procedures such as rhytidectomy. [30]
Another study emphasized that the frontal branch of the facial nerve is protected by a deep layer of fascia known as parotid-temporal fascia, which is distinct from the SMAS. This anatomical detail is essential for surgeons to consider when planning incisions and dissections in this area. [31]
-
Skull.
-
Facial muscles: 1. Galea aponeurotica 2. Frontalis 3. Procerus 4. Depressor supercilii 5. Corrugator supercilii 6. Orbicularis oculi 7. Nasalis 8. Levator labii superioris 9. Levator anguli oris 10. Levator labii superioris alaeque nasi 11. Orbicularis oris 12. Mentalis 13. Depressor labii inferioris 14. Depressor anguli oris 15. Platysma 16. Masseter 17. Zygomaticus major 18. Zygomaticus minor 19. Temporalis 20. Lateral pterygoid 21. Medial pterygoid 22. Buccinator
-
1. Forehead rhytids 2. Corrugator rhytids 3. Procerus rhytids 4. Brow ptosis 5. Brow symmetry/asymmetry 6. Secondary dermatochalasis 7. Crow’s feet 8. Brow fat pad volume and position 9. Forehead height 10. Ptosis 11. “Fat nose” 12. Lateral droop and slide 13. Temporal rhytids and temporal hollowing
-
1. Frontalis action 2. Procerus action 3. Corrugator action 4. Action of lateral orbicularis 5. Temporal slide 6. Weight of brow
-
1. Frontalis muscle 2. Brow fat pad 3. Orbital orbicularis muscle 4. Procerus muscle 5. Depressor supercilii 6. Corrugator muscle 7. Supratrochlear nerve 8. Supraorbital nerve 9. Medial branch of the supraorbital nerve (Superficial branch) 10. Lateral branch of the supraorbital nerve (deep branch) 11. Temporal fusion line 12. Conjoint tendon 13. Frontal branch of the facial nerve 14. Orbital orbicularis at the temporal raphe causing crow’s feet
-
Sagittal section of the forehead and brow illustrating the cross-sectional anatomy.