Overview
The ear is a complex structure that plays a crucial role in hearing and balance. [1, 2] The anatomy of the ear is composed of the following parts: [3, 4, 5, 6]
-
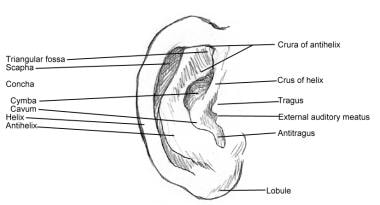
External ear (auricle) - The external ear includes the visible part of the ear, known as the auricle or pinna, and the external auditory canal. This part collects sound waves and funnels them toward the tympanic membrane (eardrum), which separates the external ear from the middle ear. [1, 2] (See the following image.)
-
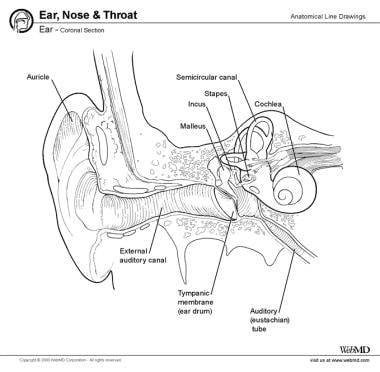
Middle ear (tympanic): An air-filled structure containing the malleus, incus, and stapes. These bones, called the ear ossicles, amplify sound vibrations from the eardrum and transmit them to the inner ear. The middle ear also houses the Eustachian tube, which helps in equalizing air pressure between the middle ear and the nasopharynx (external environment), ensuring proper sound transmission. [1, 2] (See the image below.)
-
Inner ear (labyrinthine): A fluid-filled compartment consisting of semicircular canals, vestibule, and cochlea (see the image below):
-The cochlea is a spiral-shaped structure responsible for converting sound vibrations into electrical signals that are transmitted to the brain via the auditory nerve, also known as the vestibulocochlear nerve (eighth cranial nerve, CN VIII), for sound perception. [1, 2]
-The vestibular system includes the semicircular canals and vestibule, which are essential for maintaining balance by detecting head movements and spatial orientation. [1, 2]
The ear is a multifaceted organ that connects the central nervous system (CNS) to the external head. This structure as a whole can be considered as three separate organs that work collectively to coordinate certain functions such as hearing and balance. Any disharmony in this continuum may disrupt the ear's functionality. [3, 4, 5, 7]
Embryology
The development of the external ear is a complex process that involves the merger of the six auricular hillocks. The complexity inherent in this process creates many areas for abnormal growth and development to occur. Development begins at 3 weeks' gestation, with the formation of the otic disc from a thickening of the ectoderm. The developing otic disc reshapes into an otic pit. This growing auricular complex forms ventrocaudally, near the base of the neck, but moves dorsocranially with the growth of the mandible and ultimately arrives at its final position, level with the eyes, around 32 weeks' gestation. Ears positioned more posteriorly on the head are associated with chromosomal abnormalities. [8]
The six hillocks form from the first and second branchial arches and merge to form the structures of the auricle. The tragus, helical crus, and helix likely form from the first arch (first through third hillocks), which is referred to as the mandibular arch. The antihelix, antitragus, and lobule form from the second arch (fourth through sixth hillocks), also referred to as the hyoid arch. Growth is largely complete by 20 week's gestation, and most abnormalities in ear development occur prior to the seventh week. The final contour of the ear is the result of the fusion of these hillocks and the intrinsic and extrinsic musculature of the ear that forms the various curves and folds. [9, 8]
Gross Anatomy
As noted earlier, the ear is composed of external, middle (tympanic) (malleus, incus, and stapes), and inner (labyrinth) (semicircular canals, vestibule, and cochlea) portions. See the video below.
External ear
The auricle and external acoustic meatus (or external auditory canal) compose the external ear. The external ear functions to collect and amplify sound, which then gets transmitted to the middle ear. The asymmetric shape of the external auricle introduces delays in the path of sound that assists in sound localization.
Auricle
The auricle, or pinna, is the visible, external part of the ear that plays a key role in capturing and directing sound waves into the external auditory canal. The auricle is made up of elastic fibrocartilage covered by skin, except for the lobule, which contains no cartilage. [1]
The concha surrounds the opening to the external auditory meatus (external auditory canal), whereas the auricle consists of the following (see the image below): [1, 10]
-
Helix - The outermost curved rim
-
Root/crus of helix - The anterior extension of the helix
-
Antihelix - A ridge parallel to the helix that divides into two crura (superior and inferior)
-
Crura of antihelix (superior, inferior) - The inferior crus of the antihelix, also known as the anterior crus, is the lower ridge of the cartilage at the bifurcation of the antihelix, extending beneath the fold of the ascending helix to separate the concha from the triangular fossa. It is sharply defined and less variable than the superior crus. The superior crus, or posterior crus, is the upper ridge of the cartilage that separates the scapha from the triangular fossa, running in a superior and slightly anterior direction, with a less pronounced fold compared with the inferior crus.
-
Scaphoid fossa - The groove between the helix and antihelix
-
Triangular fossa - A depression between the cura of the antihelix
-
Concha - The deepest depression in the auricle leading to the external auditory meatus
-
Tragus - A projection anterior to the concha
-
Antitragus – An arch-shaped cartilage structure opposite the tragus, separated by the intertragic notch
-
Lobule - The soft, fleshy lower part of the auricle
The arterial supply of the auricle is composed of the posterior auricular artery, the anterior auricular branch of the superficial temporal artery, and the occipital artery. Veins accompany the corresponding named arteries.
Sensory innervation of external ear
The sensory innervation of the external ear has been well studied and is composed of the following:
-
The great auricular nerve originates from the C2-3 branches of the cervical plexus; the sensory territory of this nerve is the lower two thirds of the anterior and posterior external ear.
-
The sensory innervation to the anterior superior one third of the ear (tragus, crus helix, and superior helix) is the auriculotemporal nerve (branch of V3).
-
The lesser occipital nerve derives its origin from the C2 branch of the cervical plexus and supplies sensory information from the posterior (cranial) surface of the superior one third of the external ear.
-
The auricular branch of the vagus nerve (Arnold nerve) innervates the external auditory canal floor and concha.
-
The dual innervation of the auricle from the cranial and cervical nerves explains its sensitivity and association with reflexes, such as coughing or gagging, triggered by the stimulation of Arnold's nerve. [11]
External acoustic meatus (external auditory canal)
The external acoustic meatus (external auditory canal) is formed of cartilage and bone (temporal). The canal measures about 4 cm in length (from the tragus) to the tympanic membrane and is curved in an S shape. The mandibular condyle sits anterior to the bony portion of the external acoustic meatus (external auditory canal). The mastoid air cells sit behind the bony portion of the canal (see the image below).
The canal's outer third is cartilaginous, while the inner two thirds are bony. This structural composition supports sound conduction and protects deeper structures from physical damage. [12]
Sensory innervation to the external acoustic meatus (external auditory canal) consists of the following:
-
The auriculotemporal nerve (from the mandibular branch of the trigeminal nerve) provides sensory information from the anterior wall and roof
-
The posterior wall and floor sensibility is carried in the nerve fibers of the auricular branch of vagus (Arnold nerve)
-
The tympanic plexus offers some contributions
The arterial supply includes the posterior auricular artery, deep auricular branch of the maxillary artery, and superficial temporal artery.
The primary role of the external acoustic meatus is to conduct sound waves from the external environment to the tympanic membrane. The canal's shape and ceruminous glands help prevent foreign objects from reaching and damaging the tympanic membrane. Cerumen (earwax) produced by these glands also has antibacterial properties due to enzymes such as lysozyme. [13]
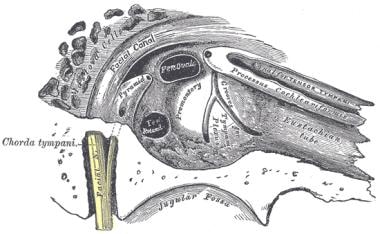
Middle ear (tympanic cavity)
The primary functionality of the middle ear (tympanic cavity) is that of bony conduction of sound via transference of sound waves in the air collected by the auricle to the fluid of the inner ear. The middle ear inhabits the petrous portion of the temporal bone and is filled with air secondary to communication with the nasopharynx via the auditory (Eustachian) tube (see the following image). [14] This connection helps equalize pressure on either side of the tympanic membrane. [1]
The tympanic cavity (middle ear) extends from the tympanic membrane to the oval window and contains the bony conduction elements of the malleus, incus, and stapes. The malleus attaches to the tympanic membrane and articulates with the incus, which in turn connects to the stapes. The stapes footplate fits into the oval window, transmitting vibrations to the cochlear fluid. [1] The walls of the tympanic cavity are complex with important associations as follows:
-
The lateral wall contains the tympanic membrane
-
The posterior wall contains the mastoid antrum and communicates with the mastoid air cells
-
The medial wall contains the oval window; posterior to and separated by the promontory is the round window — this wall is also called the labyrinthine wall.
-
The anterior wall is also termed the carotid wall because a thin plate of bone separates the carotid canal and tympanic cavity; this wall is perforated by the tympanic branch of the internal carotid artery and deep petrosal nerve (connecting the sympathetic plexus of the carotid to the tympanic plexus in the tympanic cavity) and also houses the auditory tube.
-
The roof of the tympanic cavity is the tegmental wall; it separates the epitympanic recess (which contains the malleus and the incus) from the middle cranial fossa.
-
The floor of the middle ear is the jugular wall; it separates the tympanic cavity from the internal jugular vein.
Tympanic membrane
The tympanic membrane is an oval, thin, semitransparent membrane that separates the external and middle ear (tympanic cavity). The tympanic membrane is divided into two parts: the pars flaccida and the pars tensa. The manubrium of the malleus is firmly attached to the medial tympanic membrane; where the manubrium draws the tympanic membrane medially, a concavity is formed. The apex of this concavity is called the umbo. The area of the tympanic membrane superior to the umbo is termed the pars flaccida; the remainder of the tympanic membrane is the pars tensa (see the image below).
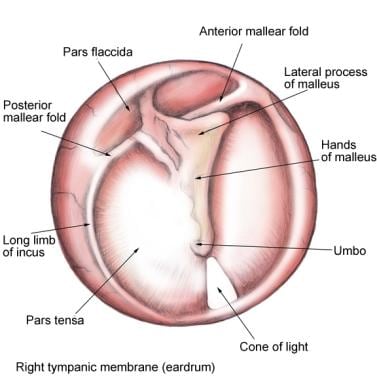 Tympanic membrane (TM): pars flaccida (superior to insertion manubrium) and pars tensa (remainder of TM).
Tympanic membrane (TM): pars flaccida (superior to insertion manubrium) and pars tensa (remainder of TM).
Air vibrations collected by the auricle are transferred to the mobile tympanic membrane, which then transmits the sound to the ossicles.
The sensory nerve supply to the tympanic membrane includes the following:
-
Auriculotemporal nerve (mandibular branch of the trigeminal nerve)
-
Auricular branch of the vagus nerve (Arnold nerve)
-
Tympanic branch of the glossopharyngeal nerve (Jacobson nerve)
Blood supply is derived from the stylomastoid branch of the posterior auricular, deep auricular, and anterior tympanic branches from the maxillary artery. Venous drainage includes the external jugular from veins on the superficial aspect of the tympanic membrane and veins from the deep surface of the tympanic membrane draining to the transverse sinus and dural veins.
Tympanic cavity (middle ear)
Multiple structures are contained within the confines of the tympanic cavity (middle ear). Muscles, nerves, and the auditory tube occupy space within the tympanic cavity. The cavity is covered in mucoperiosteum.
Ossicles
From the deep surface of the tympanic membrane to the oval window is a chain of movable bones, the ossicles. The ossicles are named as follows (see the following image):
-
Malleus (hammer)
-
Incus (anvil)
-
Stapes (stirrup)
These bony elements serve to transmit and amplify sound waves from the air to the perilymph of the internal ear. Sound waves transmitted to the tympanic membrane push it medially, the malleus pulls the incus laterally through its synovial joint, the incus then causes the footplate of the stapes to displace the oval window (the fenestra vestibuli), causing a pressure wave in the fluid of the inner ear. This bony conduction amplifies the sound wave from air approximately 10 times.
Auditory tube
The auditory tube (Eustachian tube) is the communication between the middle ear and the nasopharynx. Its function is to equalize pressure across the tympanic membrane. Contraction of the tensor veli palatini and the salpingopharyngeus outside of the tympanic cavity (middle ear) dilates and opens the auditory tube (see the image below).
Muscles
Important musculature in the middle ear (tympanic cavity) includes: [1]
-
Tensor tympani - Attaches to the malleus and helps dampen sounds by tensing the tympanic membrane. It is innervated by the nerve to the tensor tympani, a branch of the mandibular nerve (a branch of the trigeminal nerve).
-
Stapedius - It is the smallest skeletal muscle in humans. It attaches to stapes and stabilizes it during loud sounds, preventing excessive movement. Innervation is provided by the nerve to the stapedius from the facial nerve.
Contraction of the stapedius muscle displaces the stapes posteriorly and functions to prevent loud noises from injuring the inner ear. Facial nerve paralysis causes uninhibited movement of the stapes footplate, increasing the perception of sound, which can then cause damage to the inner ear.
The tendon of the tensor tympani attaches to the manubrium of the malleus. Its muscle belly lies in a semicanal superior to the auditory tube. Innervated by the mandibular branch of the trigeminal nerve, contraction of the tensor tympani displaces the malleus (and the tympanic membrane) medially, thus tensing the tympanic membrane and dampening sound vibration as well. This muscle lies within the temporal bone in a plane along the superior aspect of the auditory tube.
Innervation
The horizontal portion of the facial nerve traverses through the tympanic cavity on its labyrinthine wall in a bony canal just superior to the footplate of the stapes.
The chorda tympani, a recurrent branch of the facial nerve, is given off before the facial nerve exits the stylomastoid foramen. It enters the tympanic cavity (middle ear) after exiting a bony canal and passing medial to the neck of the malleus invested in the mucous membrane, then it emerges in the carotid wall. The chorda tympani innervates the submandibular and sublingual salivary glands and the anterior two thirds of the tongue (carrying taste information).
Sensory information about the middle ear is carried by multiple nerves that contribute to the tympanic plexus located on the promontory of the medial wall as follows:
-
Tympanic branch of the glossopharyngeal (Jacobson nerve) - This contributes to the tympanic plexus
-
Superior and inferior caroticotympanic nerves - These are branches from the sympathetic carotid plexus that join the tympanic branch of the glossopharyngeal nerve to contribute to the tympanic plexus.
-
Communication with a branch from the greater petrosal nerve
The tympanic plexus then supplies branches to the mucous membrane of the tympanic cavity (middle ear), the fenestra vestibuli, and the auditory tube, in addition to other regions.
The lesser petrosal nerve leaves the tympanic plexus by passing superiorly into the floor of the middle cranial fossa.
Vascular supply
The arterial supply of the cavity includes the tympanic branch of the maxillary (tympanic membrane), stylomastoid branch of the posterior auricular (posterior cavity and mastoid), petrosal branch of the middle meningeal, branch of the ascending pharyngeal, tympanic branch of the internal carotid, and a branch from the artery of the pterygoid canal (follows the auditory tube). Venous drainage is to the pterygoid plexus and the superior petrosal sinus.
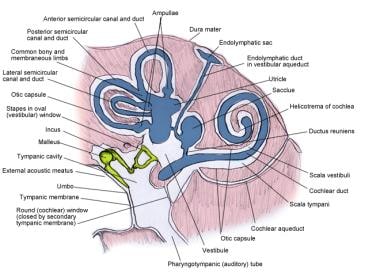
Inner ear (labyrinthine cavity)
The inner ear, also called the labyrinthine cavity, functions to conduct sound to the CNS as well as to assist in balance (see the first image below). Auditory transduction, the conversion of acoustic (mechanical) energy to electrochemical energy, takes place within the labyrinthine cavity (see the second image below).
The labyrinthine cavity is essentially formed of the membranous labyrinth encased in the bony osseus labyrinth (see the following image). The osseus labyrinth is a series of bony cavities within the petrous temporal bone; the membranous labyrinth is the communicating membranous sacs and ducts housed within the osseus labyrinth. The membranous labyrinth is cushioned by the surrounding perilymph and contains the endolymph within its confines. The membranous labyrinth also has cochlear, vestibular, and semicircular components.
The osseus labyrinth consists of the cochlea, vestibule, and semicircular canals (see the image below). These bony cavities are lined with periosteum and contain perilymph. The fenestra vestibuli or oval window is an opening in the lateral wall of the vestibule of the osseous (bony) labyrinth. It articulates with the footplate of the stapes from the middle ear and opens into the fluid-filled inner ear.
Vestibule
The vestibule is the central part of the osseous labyrinth and is found medial to the tympanic cavity (middle ear), in front of the semicircular canals, and behind the cochlea. [15] Its anatomic borders include the following:
-
Its lateral wall, the tympanic wall, contains the fenestra vestibuli (the oval window), which receives information from the base of the stapes of the middle ear.
-
The medial wall of the vestibule contains the filaments of the acoustic nerve to the saccule (part of the membranous vestibule), communicating via perforations in the depression named the recessus sphericus; similarly, filaments of the acoustic nerve that supply the vestibular end of the ductus cochlearis pass through the fossa cochlearis.
-
The roof is perforated, and these apertures transmit the nerves to the utricle (part of the membranous vestibule) and ampullae (part of the membranous semicircular canals).
-
To the posterior are openings to the semicircular canals, and to the anterior is the communication with the scala vestibuli of the cochlea.
The vestibular apparatus is the membranous vestibule and is composed of the utricle and saccule. These "otolithic organs" sense linear acceleration in the horizontal and vertical planes. The utricle is closer in proximity to the semicircular canals, and the saccule is close to the cochlea. The orientation of the utricle is largely axial and registers acceleration in the horizontal plane. Conversely, the saccule is oriented in a coronal plane and senses acceleration in a vertical plane. The saccule is connected to the cochlear duct via the ductus reuniens and to the utricle by the utriculosaccular duct. The endolymphatic duct is a branch of the utriculosaccular duct and terminates as a dilated endolymphatic sac. The endolymphatic duct and sac play an important role in the uptake and removal of endolymph.
Within these organs are hair cells (the saccule macula and utricle macula); the cilia of these cells are intricately associated with a membranous substance containing calcium carbonate granules, or "otoliths." Movement of the head induces shearing of the hair cells by the mobile otoliths. This directional change is sensed by the brain via the superior division of the vestibular nerve at the utricle and via the inferior division of the vestibular nerve to the saccule. Together, the otolithic organs of both ears are of prime importance in directional sensation.
Semicircular and membranous canals
There are three bony semicircular canals; each stands at right angles to the other two canals. The superior, posterior, and lateral semicircular canals sit behind and superior to the vestibule (see the following image). At one end of each canal is the ampulla, a dilatation of the end. These canals open into the vestibule (utricle) via five ampullae.
The superior canal is positioned vertically; its lateral end is ampullated and communicates with the upper vestibule, whereas the opposite end joins the upper posterior canal at the crus commune, which opens into the upper medial vestibule. The posterior canal parallels the posterior petrous temporal bone; its lower end, the ampullated end, opens into the lower vestibule, whereas the upper end joins the crus commune. The lateral canal is directed horizontally, and its ampullated end opens to the upper and lateral vestibule, whereas the opposite end opens to the upper posterior vestibule. As noted earlier, each canal is positioned perpendicular to the others.
The membranous canals are similarly termed superior, posterior, and lateral. Their functionality includes the ability to sense rotational velocity in three dimensions. This function is achieved via the cristae ampullaris, mechanoreceptors within the confines of the membranous ampullae. The endolymphatic flow changes within the substance of the semicircular canals are sensed by these mechanoreceptors, and this information is transmitted to the vestibular nerve. This ability to detect angular acceleration in three dimensions is critical for maintaining balance.
Cochlea
The cochlea is an organ essential to hearing within the inner ear (see the image below). It is responsible for converting sound waves into electrical signals that the brain interprets as sound. [1] The osseus cochlea is shaped like a snail shell, with 2.5 turns of a canal coiled around the central modiolus. The bony cochlea communicates with the bony vestibule. Its base is perforated for the transmission of filaments of the cochlear division of the vestibulocochlear nerve (cranial nerve VIII).
Within the bony cochlea lies the membranous cochlea, wherein the energy of sound via pressure waves is transferred within the middle ear to the cochlear endolymph. The energy created in this liquid medium is converted to electrical energy that is transmitted to the CNS via the cochlear nerve.
The cochlea is split into three chambers (see the image below), the scala vestibuli, the cochlear duct, and the scala tympani.
The scala vestibuli, or the superior chamber, is separated from the cochlear duct by the vestibular membrane (Reissner membrane) and contains perilymph. This chamber originates in the vicinity of the oval window (which communicates with the middle ear and the footplate of the stapes) and spirals toward the apex of the modiolus, the helicotrema, where it communicates with the scala tympani.
The cochlear duct, or the scala media, the central chamber, is well-defined by the vestibular membrane superiorly and the basilar membrane inferiorly. This membranous organ contains the endolymph and the spiral organ (of Corti).
The scala tympani, or the inferior chamber, is separated from the cochlear duct (above) by the basilar membrane and contains perilymph. In contrast to the scala vestibuli, the scala tympani commences at the apex of the modiolus, the helicotrema, and winds down to the round window (fenestra cochleae), which is covered by the secondary tympanic membrane. The round window opens to the middle ear (tympanic canal).
Sound transduction occurs in the membranous cochlea via the spiral organ (of Corti). The spiral organ is composed of four rows of hair cells sitting on the basilar membrane. These hair cells have stereocilia branching outward into the gelatinous tectorial membrane (see the previous image). Sound transmission occurs after transmission to the middle ear via the tympanic membrane.
Once a sound wave has been conducted via the osseus tympanic cavity (middle ear), the energy is transmitted by the footplate of the stapes displacing the oval window medially into the vestibule in the region of the base of the cochlea. Fluid then flows within the scala vestibuli of the cochlea, transmitting pressure to the basilar membrane; eventually, the flow proceeds to the scala tympani, displacing the round window membrane back into the middle ear. This perilymph flow within the cochlea leads to mobility of the hair cells of the spiral organ.
The basilar lamina, when uncoiled, has an apex and base; the apex is wider than the base (see the image below). Acoustic stimulation travels from the base to the apex, with higher frequency stimuli causing excitation at the base, low frequency at the apex. The information transmitted by the hair cells within the spiral organ to the cell bodies, spiral ganglion, of the cochlear nerve. These nerve endings exit on the modiolar side of the spiral organ.
Innervation
The vestibulocochlear nerve (cranial nerve VIII) is the primary nerve of the inner ear. This nerve originates between the pons and medulla oblongata in the brain and passes into the petrous temporal bone through the internal acoustic meatus. It is within the temporal bone that the nerve divides into superior and inferior vestibular nerves as well as a cochlear branch. Vestibular nerves carry information from the saccule, utricle, and ampullae by way of the vestibular (Scarpa) ganglion. Sound information is transmitted through the spiral ganglion to the cochlear nerve from the cochlea.
Pathologic Variants
Auricle
Variant anatomy of the external ear can be divided into congenital and acquired entities. Acquired entities can further be delineated into intrinsic processes such as cancer and extrinsic processes such as trauma.
Congenital abnormalities of the ear are common and largely affect the shape of the auricle. They are often accompanied with abnormalities of the middle ear because the underlying development of both arises from similar structures. Microtia refers to the abnormal phenotypes of the external ear. Numerous grading systems have been developed to categorize microtia. A common system uses the following terminology:
-
Grade I - A less developed ear that is smaller than the unaffected side but contains most of the structures of a normal ear with good structural definition
-
Grade II - A partially developed ear, smaller than grade I, and with loss of most of the ear's contour definition, often accompanied with a stenotic external ear canal, producing partial conductive hearing loss
-
Grade III - (Most common) Absence of the external ear, excepting a small, unorganized structure, often described as resembling a peanut, and an absence of the external ear canal and ear drum
-
Grade IV - Absence of the total ear, also known as anotia [16]
Congenital auricular anomalies are further divided into deformations (abnormal shape but complete development) and malformations (underdeveloped auricle due to partial deficiencies in the skin and/or cartilage). These conditions can have significant social and psychological impacts due to their appearance. [17]
Acquired abnormalities usually arise from skin cancers that can affect the auricle. These include melanoma, squamous cell carcinoma, and basal cell carcinoma. Trauma can also affect the auricle. Along with various lacerations and avulsions that can occur to any body part, blunt trauma can cause auricular hematomas. Hematomas can disrupt the perichondrium and create an abnormal healing cycle that results in a "cauliflower" ear deformity. [16, 18]
Humid conditions and swimming in contaminated water can predispose patients to infections of the external ear, otitis externa.
Pathologic variants extend beyond visible deformities to include anomalies within the middle and inner ear structures. Chronic otitis media has been linked to anatomical variations such as high jugular bulb and anteriorly located sigmoid sinus, which pose surgical risks but are not typically etiological. Inner ear anomalies associated with congenital aural atresia include lateral semicircular canal dysplasia and high-riding jugular bulb. [19, 20]
Middle ear
Tympanic membrane perforations are not uncommon and usually occur within the pars tensa. Small, central perforations often heal without significant sequela; however, marginal perforations that don't heal can lead to growth of skin from the ear canal into the middle ear. Large, nonhealing perforations decrease the surface area of the tympanic membrane, leading to impaired acoustic collection.
Many etiologies of tympanic membrane perforation exist, including foreign body introduction (i.e., pencil/cotton applicator), sparks from welding in industrial settings. Explosions can also cause intense pressure and perforation to the tympanic membrane. In addition, deep-sea divers and miners are at risk for middle ear hemorrhage and tympanic membrane perforation when descending from/ascending to the surface rapidly.
Otitis media
Acute and chronic inflammation of the middle ear lining, otitis media, can lead to severe swelling and subsequent necrosis and perforation of the tympanic membrane, allowing spontaneous drainage of fluid (usually pus). Chronic inflammation can lead to irreversible scarring of the tympanic membrane, termed tympanosclerosis, leading to poor mobility of the tympanic membrane and poor sound conduction. Chronic fluid and inflammation in the middle ear worsens hearing and can interfere with language skills, often seen in children with auditory tube dysfunction.
Otosclerosis and trauma
Bone formation around the ossicular chain of the middle ear can lead to poor mobility of the joints, specifically the stapes and oval window. This leads to discontinuity of the ossicular chain of the middle ear with the inner ear, resulting in progressive conductive hearing loss. This condition is termed otosclerosis.
An additional etiology of hearing impairment in the middle ear is trauma; shearing forces can uncouple the ossicular chain, thus leading to disrupted conduction of sound.
Cholesteatomas
Benign epidermoid tumors, cholesteatomas (see the image below), can occur in the middle ear and mastoid. These traditionally form from acquired etiologies such as tympanic membrane perforations, with the skin healing into the middle ear and chronic auditory tube dysfunction. These can also arise from congenital skin remnants in the middle ear. Cholesteatomas are not malignant, but they become problematic as they are locally destructive secondary to erosion and the dead debris that accumulates, and they can become a nidus for infection. Studies indicate a strong hereditary component for cholesteatomas, with individuals having a first-degree relative with the condition being at higher risk. [21]
Inner ear
Infectious disease
Inner ear dysfunction can occur secondary to congenital etiologies such as rubella. Pregnant mothers can contract this virus, leading to destruction of the developing fetal cochlea and subsequent deafness. Acquired measles and mumps can also lead to cochlear damage and childhood deafness. Additionally, congenital cytomegalovirus infection is recognized as a prevalent nongenetic cause of sensorineural hearing loss. [22]
Meningitis
Meningitis can produce inner ear pathology and symptoms as a consequence of communication between the perilymph of the inner ear and cerebrospinal fluid. The cochlea can be destroyed, eventually leading to permanent deafness.
Ménière's disease and Ménière syndrome
Ménière's disease and Ménière syndrome are pathologic entities that are incurred as a result of an inflammatory response and endolymphatic accumulation in excess, endolymphatic hydrops. This endolymphatic hydrops and subsequent increased pressure leads to episodic hearing loss, tinnitus, severe vertigo, and a sense of fullness in the ear. Increasing endolymphatic pressure ruptures the lining of the membranous labyrinth, creating an avenue for a mixture of endolymph and perilymph and subsequent permanent hearing loss. The disease and syndrome are differentiated by idiopathic etiology (disease) versus excess endolymphatic accumulation secondary to increased production or decreased resorption (syndrome).
Benign paroxysmal positional vertigo
Benign paroxysmal positional vertigo (BPPV) is a pathologic disorder of the inner ear. Patients traditionally experience repetitive episodes of vertigo incurred after changes in the position of the head relative to gravity. The pathologic mechanism is thought to be caused by dislodgement of the otoconia, "ear rocks," within the utricle. The mobilized otoconia, crystals made of calcium carbonate, migrate into the semicircular canals. Head reorientation relative to gravity induces movement of these crystals within the semicircular canal, inducing endolymphatic fluid displacement and a sensation of vertigo. This disorder can be diagnosed using the Dix-Hallpike maneuver, which reorients the head to align the posterior canal with gravitational forces, provoking the classic positional vertigo.
Presbycusis
Hair cells often degenerate with age, a condition known as presbycusis. This gradual hearing loss varies among individuals with regard to severity. Hearing loss can also be spurred by prolonged sound exposure greater than 85 dB, such as that in industrial settings. Prolonged exposure exhausts ear hair cells, with eventual irreversible hair cell injury.
Head trauma
Head injuries deserve mention as well. Temporal bone fractures can produce middle ear pathology and conductive hearing loss. Disruption of the cochlea can occur, leading to sensorineural hearing loss.
-
External ear anatomy.
-
Cross-section of the middle and inner ear.
-
Tympanic membrane (TM): pars flaccida (superior to insertion manubrium) and pars tensa (remainder of TM).
-
Auditory tube cross-section.
-
The middle ear ossicles. Inf = inferior; Lat = lateral; Med = medial; Sup = superior.
-
Inner ear. Ant = anterior; Inf = inferior; Lat = lateral; Sup = superior.
-
Inner ear: bony and membranous labyrinths.
-
Cross-section of cochlea.
-
Cholesteatoma.
-
Sound transmission pathway.
-
Inner ear in relation to middle and external ear.
-
Osseous labyrinth.
-
The cochlea.
-
Higher frequencies stimulate the base of the cochlea, whereas lower frequencies stimulate the apex.
-
Auricular hematoma.
-
Ear anatomy. Courtesy of Hamid R Djalilian, MD.