Overview
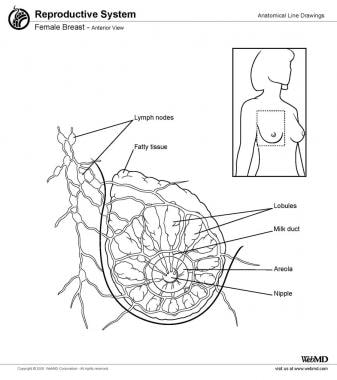
Breast shape varies among patients, but knowing and understanding the anatomy of the breast ensures safe surgical planning (see the image below). The human breasts are compound tubuloalveolar structures. At its core, the breast consists of glandular tissue, which includes milk-producing glands, lobes, and lobules that become active during lactation. A single breast may contain 15-20 lobes around the nipple in a radial pattern. The produced milk travels through lactiferous ducts to the nipple-areolar complex. The terminal duct lobular units or lobules are the milk-producing structures in the breast. They are the most common sites for developing breast cancer. This anatomical understanding plays a crucial role in surgical planning, especially in cosmetic and reconstructive procedures. [1]
When the breasts are carefully examined, significant asymmetries are revealed in most patients. Any preexisting asymmetries, spinal curvature, or chest wall deformities must be identified and the same should be informed to the patient as these may be difficult to correct and can become noticeable in the postoperative period. Imaging technologies, such as four-dimensional photography, have improved the ability to identify and quantify breast and chest wall asymmetries, enhancing surgical outcomes. [2]
Preoperative photographs with multiple views are obtained for all patients and maintained as part of the office record.
Vascular Anatomy and Innervation of the Breast
The blood supply to the breast skin depends on the subdermal plexus, which is in communication with deeper underlying vessels supplying blood to the breast parenchyma. The blood supply is derived from the following:
-
The internal mammary perforators (most notably the second to fifth perforators)
-
The thoracoacromial artery
-
The vessels to serratus anterior
-
The lateral thoracic artery
-
The terminal branches of the third to eighth intercostal perforators
The superomedial perforator supplies from the internal mammary vessels is particularly robust and accounts for some 60% of the total breast blood supply. This rich blood supply allows for various reduction techniques, ensuring the viability of the skin flaps after surgery. [4] The breast is highly vascularized. The majority of the breast's blood supply continues to come from the internal mammary perforators, particularly the superomedial perforators located in the second to fifth intercostal spaces. The lateral thoracic artery, thoracoacromial artery, and perforators between the third and eighth intercostal spaces also play significant roles in supplying blood to the breast. In reconstructive and reduction surgery, preserving the vascular integrity of the nipple-areola complex has become a primary focus to avoid ischemic complications after surgery. [10]
Sensory innervation of the breast is dermatomal in nature. It is mainly derived from the anterolateral and anteromedial branches of thoracic intercostal nerves T3-T5. Supraclavicular nerves from the lower fibers of the cervical plexus also provide innervation to the upper and lateral portions of the breast. Researchers believe sensation to the nipple derives largely from the lateral cutaneous branch of T4. It is important to preserve this nerve during surgeries to maintain nipple sensation, particularly in procedures such as reconstructive or reduction surgeries. [10]
Thorough knowledge of the vascular and nervous systems of the breast has led to improved outcomes in breast surgeries by preventing sensory loss and vascular complications. This enhanced knowledge is especially useful in therapeutic contexts where the focus is on conserving both blood supply and sensation. [10]
Breast Parenchyma and Support Structures
The breast is made up of fatty tissue and glandular, milk-producing tissues (see the image below). The ratio of fatty tissue to glandular tissue varies among individuals. In addition, with the onset of menopause (i.e., decrease in estrogen levels), the relative amount of fatty tissue increases as the glandular tissue diminishes. As our knowledge regarding the anatomy of the breast's parenchyma and support structures has improved, our understanding, particularly for surgical applications in breast reduction and reconstruction has advanced. [11, 12]
The base of the breast overlies the pectoralis major muscle between the second and sixth ribs in the nonptotic state. The gland is anchored to the pectoralis major fascia by the suspensory ligaments first described by Astley Cooper in 1840. These ligaments run throughout the breast tissue parenchyma from the deep fascia beneath the breast and attach to the dermis of the skin. Because they are not taut, they allow for the natural motion of the breast. These ligaments relax with age and time, eventually resulting in breast ptosis. The breast's fascial system is divided into intraglandular and extraglandular structures. This extensive network of connective tissues serves both cosmetic and functional needs, especially in reconstructive procedures. The inframammary fold supports the lower pole of the breast and serves as an anatomical barrier that defines the breast's form, preserving the natural contour of the breast. [11, 12, 13]
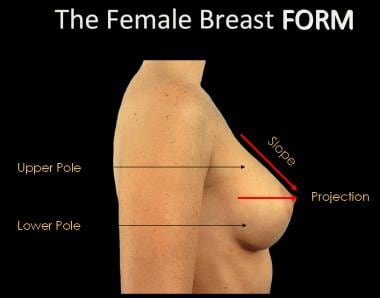
The lower pole of the breast is fuller than the upper pole (see the image below). The inframammary fold is formed by the skin extending from the level of the fourth and fifth ribs. Knowing the structural anatomy of the inframammary fold is crucial for breast reconstruction. [14] The tail of Spence extends obliquely up into the medial wall of the axilla. [4] It is a significant structure that surgeons must consider during axillary and breast surgeries. Furthermore, the horizontal and vertical septa have been recognized as important neurovascular landmarks, guiding surgeons during breast procedures to prevent injury to essential blood vessels and nerves. The pectoralis major muscle, which the breast takes support from, can also be used to fill defects following lumpectomy or during breast reconstruction surgery. These findings are essential for improving outcomes in breast reconstruction and reduction operations because they preserve both the aesthetic appearance and functionality of the breast. [11, 12]
The breast overlies the pectoralis major muscle as well as the uppermost portion of the rectus abdominis muscle inferomedially. The nipple should lie above the inframammary crease and is usually level with the fourth rib and just lateral to the midclavicular line. The average nipple-to-sternal notch measurement in a youthful, well-developed breast is 21-22 cm; an equilateral triangle formed between the nipples and sternal notch measures an average of 21 cm per side. [4]
Musculature Related to the Breast
The breast lies over the musculature that encases the chest wall. The muscles involved include the pectoralis major, serratus anterior, external oblique, and rectus abdominis fascia. The blood supply that provides circulation to these muscles perforates through to the breast parenchyma, thus also supplying blood to the breast. By maintaining continuity with the underlying musculature, the breast tissue remains richly perfused, thus preventing complications arising from aesthetic or reconstructive surgery that requires the placement of a breast implant.
Pectoralis major
The pectoralis major muscle is a broad muscle that extends from its origin on the medial clavicle and lateral sternum to its insertion on the humerus. The thoracoacromial artery is its source of major blood supply, while the intercostal perforators arising from the internal mammary artery provide a segmental blood supply. The medial and lateral anterior thoracic nerves provide innervation for the muscle, entering posteriorly and laterally. The action of the pectoralis major is to flex, adduct, and rotate the arm medially.
The pectoralis major is extremely important in aesthetic and reconstructive breast surgery because it provides muscle coverage for the breast implant. In reconstructive surgery, the pectoralis major muscle covers the implant, providing a decreased risk for exposure of the implant as the skin and underlying subcutaneous tissues are often thin following mastectomy. The muscle also provides additional tissue between implant and skin, thus decreasing the palpability of the implant.
The pectoralis major muscle ensures the implant remains well-protected beneath the skin, particularly following a mastectomy. However, muscle contraction can sometimes make the implant noticeable. To address this, surgeons may release the pectoralis major from its inferior and medial attachments, allowing for better placement of the implant and a more natural appearance. This approach also helps lower the position of the implant, achieving improved aesthetic outcomes. [15]
Often, placement of the implant beneath the muscle causes it to be noticeable when the pectoralis is contracted. In these instances, it may be helpful to release the pectoralis muscle from its inferior and medial attachments to decrease the incidence of noticeable contractions. In addition, with inferior release of the pectoralis muscle, a lower positioning of the implant can be achieved, resulting in a more aesthetically pleasing appearance.
Serratus anterior
The serratus anterior muscle is a broad muscle that runs along the anterolateral chest wall. Its origin is the outer surface of the upper borders of the first through eighth ribs and its insertion is on the deep surface of the scapula. Its vascular supply is derived equally from the lateral thoracic artery and from the branches of the thoracodorsal artery. The long thoracic nerve serves to innervate the serratus anterior, which acts to rotate the scapula, raising the point of the shoulder and drawing the scapula forward toward the body. Transection of the long thoracic nerve is carefully avoided during an axillary lymph node dissection because its loss results in "winging" as the scapula is released from the chest wall and moves upward and outward.
The serratus anterior muscle is an important structure during breast surgeries, particularly in implant-based reconstruction and axillary dissections. In aesthetic and reconstructive surgeries such as breast reconstruction, the serratus anterior is often involved when additional muscle coverage is needed for implant placement. Surgeons may elevate this muscle to provide a thicker muscle layer over the implant, enhancing coverage and reducing the risk for complications such as implant exposure. [15]
The use of serratus anterior fascia flaps has also been explored as a method to achieve better implant coverage, showing promising outcomes in terms of reduced complications and improved aesthetic results. This muscle's involvement is particularly valuable in modern reconstructive approaches where muscle and fascial integrity are essential for successful outcomes. [15]
Because the serratus anterior underlies the lateral aspect of the breast, in aesthetic surgery, blunt elevation of the pectoralis major laterally inadvertently elevates a small portion of the serratus muscle. Often the serratus anterior must be elevated sharply to obtain sufficient muscle layer to provide coverage of the implant. These techniques further emphasize the importance of the serratus anterior in ensuring both functional and cosmetic success in breast reconstruction procedures. [15]
Rectus abdominis
The rectus abdominis muscle demarcates the inferior border of the breast. It is an elongated muscle that runs from its origin at the crest of the pubis and interpubic ligament to its insertion at the xiphoid process and cartilages of the fifth through seventh ribs. It acts to compress the abdomen and flex the spine. The seventh to twelfth intercostal nerves provide sensation to overlying skin and innervate the muscle. Vascularity of the muscle is maintained through a network between the superior and inferior deep epigastric arteries.
The rectus abdominus muscle plays a crucial role in breast reconstruction, particularly in procedures involving the transverse rectus abdominis myocutaneous flap and the deep inferior epigastric perforator flap techniques. In breast reconstruction, the rectus fascia often needs to be elevated to provide sufficient implant coverage, especially when achieving a more natural lower breast contour. Careful attention is given to the blood supply from the superior and inferior deep epigastric arteries, which play a crucial role in maintaining vascularity to both the abdominal wall and the flap used in reconstruction. [16, 17]
When placing an implant for breast reconstruction, in attempting to achieve complete coverage with muscle, the rectus fascia must often be elevated to place the implant sufficiently caudal. This dense, thick fascia is often intimately adherent to the ribs below it. Once the fascia is elevated and released, proper positioning and expansion of the implant can be proceeded with. Elevating and releasing the rectus fascia allows for proper positioning of the implant and adequate expansion. This approach, particularly while using muscle-sparing techniques, helps minimize donor site complications such as abdominal wall weakness or hernias. These muscle-sparing techniques, along with the preservation of critical vascular structures, are key to improving outcomes in breast reconstruction procedures involving the rectus abdominis muscle. [16, 17]
External oblique
The external oblique muscle is a broad muscle that runs along the anterolateral abdomen and chest wall. Its origin is from the lower eight ribs, and its insertion is along the anterior half of the iliac crest and the aponeurosis of the linea alba from the xiphoid to the pubis. It acts to compress the abdomen, flex and laterally rotate the spine, and depress the ribs. The seventh through twelfth intercostal nerves serve to innervate the external oblique. A segmental blood supply is maintained through the inferior eight posterior intercostal arteries.
During breast reconstruction surgeries, the external oblique muscle provides support and proper implant coverage. [17] The external oblique muscle abuts the breast on the inferior lateral aspect. Elevated along with the rectus abdominis fascia to provide inferior coverage of the breast implant during reconstructive surgery, its fascia, like the fascia of the rectus abdominis muscle, must be released adequately for the proper placement and expansion of the implant.
In aesthetic surgery, placement of the implant inferiorly is usually not below these fascial attachments. If the implant is placed behind the fascia, the implant often "rides too high" and may result in a "double bubble" effect, wherein the breast parenchyma slides over and off the implant.
These surgical techniques, supported by advancements in flap-based reconstructions, help reduce complications and improve outcomes, especially in cases where thinner skin follows mastectomies. Proper handling of the external oblique muscle and its fascia is essential for ensuring both functional and cosmetic success in breast reconstruction. [17]
-
The female breast form.
-
Female breast, anterior view.
-
Anatomy of the breast. Courtesy of Wikimedia Commons (Patrick J Lynch, medical illustrator) [https://commons.wikimedia.org/wiki/File:Breast_anatomy_normal_scheme.png].