Skin Tension Lines
Skin tension lines (STLs) are the result of a complex interaction between internal and external factors involving the skin. The intrinsic framework, which consists of elastin and collagen, progressively loosens with age. Its interaction with the muscles of facial expression leads to the development of STLs. Generally, STLs are perpendicular to the underlying muscles of the face. Aging, particularly photoaging, tends to accentuate the appearance of STLs (see the image below)
In the repair of STLs, the correct placement of the long axis of an excision parallel to the STLs results in better scar cosmesis. Furthermore, flaps should be placed to allow the suture lines to fall in STLs. Although STLs may vary between individuals, some areas of the face have greater variability than others. Typically, the forehead, which has one major muscle group that pulls it vertically, has little individual variability; nearly everyone has horizontal STLs. In comparison, anatomic areas where multiple muscles act in different directions are likely to have greater variability.
In older patients, the direction of the relaxed STLs is generally obvious. In areas of ambiguity, excising the lesion as a circle and undermining it invariably pulls the surgical defect into an oval, with the long axis corresponding to the relaxed STL.
Research has contributed to greater insights into STLs beyond traditional concepts such as Langer's lines and wrinkle lines. [1] Studies employing biodynamic excisional skin tension (BEST) lines have demonstrated that these lines better represent the direction of least skin tension during excisional surgery. Unlike Langer's lines, which were derived from cadaver studies and static forces, BEST lines are based on real-time measurements of dynamic skin tension in living patients. These studies suggest that following BEST lines during excisions results in optimal wound healing and reduced scarring compared with traditional methods. [2]
BEST lines have been mapped across various body regions using tensiometers during surgeries. For example: [3]
-
On the scalp, BEST lines align coronally.
-
On the limbs, they tend to follow vertical orientations aligned with long bones.
-
On the trunk, they are predominantly horizontal but vary obliquely at regions such as the shoulders and scapulae.
Additionally, histological studies have shown that incisions parallel to collagen fibers minimize tissue destruction and fibroblast activity during wound repair, leading to less conspicuous scars. This reinforces the importance of precise alignment with tension lines during surgery. [4]
The growing understanding of STLs has practical has practical implications: [5, 6]
-
Aligning excisions with BEST or relaxed STLs reduces wound closure tension and improves cosmetic outcomes.
-
Changes in body posture can alter skin reaction forces and influence optimal excision orientation. This highlights the need for dynamic assessment during preoperative planning.
-
Innovations such as parallelogram excision designs have been proposed for high-tension areas to reduce scar length and preserve healthy tissue.
While traditional concepts such as Langer's and wrinkle lines remain useful guides for incisional surgeries, BEST lines provide a more accurate framework for excisional procedures. Adopting these advanced methodologies can significantly enhance surgical outcomes and patient satisfaction.
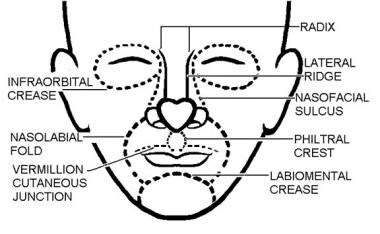
Cosmetic Units and Subunits
Junction lines are fixed landmarks that separate the cosmetic units of the face (see the image below). Placing the suture lines on these boundaries (e.g., eyebrow, nasolabial fold) optimizes scar formation. When a surgical wound is closed, repairing the wound in a cosmetic unit along a junction line is the best approach. In larger defects that require a flap, the best results are achieved using tissue from the same or adjacent cosmetic unit and by placing suture lines on the boundaries of those units.
Subunits within cosmetic units are often subtle and individually variable. Paying attention to subtleties such as color, texture, sebaceous features, and hair characteristics helps in identifying the changes between the subunits.
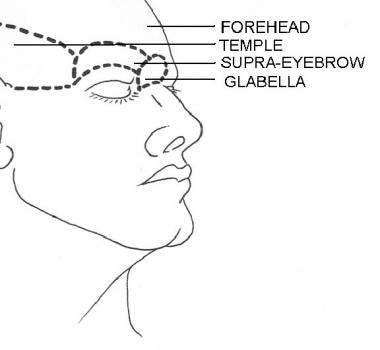
The scalp and forehead are individual cosmetic units that are separated by the hairline. In a bald individual, the top horizontal forehead crease serves as the junction line. Subunits of the forehead include the glabella, temples, and eyebrows (see the image below).
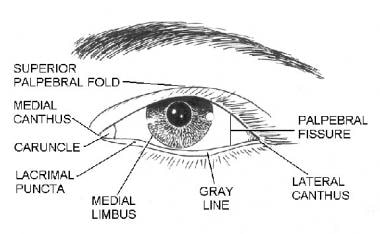
The eyelid is a complex structure with multiple subunits that mimic the underlying orbicularis oculi muscle. The largest component of the eyelid is the orbital portion, which borders the eyebrow superiorly and the cheek inferiorly. Just below the eyebrow is the preseptal area and then the pretarsal portion, where the eyelashes insert. Additional components of the eyelid include the superior palpebral fold, the palpebral fissure, the medial limbus, and the medial canthus (see the image below).
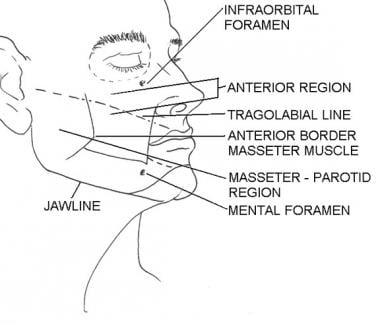
The cheek region is subdivided by the anterior prominence of the clenched masseter muscle. The masseter-parotid region lies posterior to this landmark and is posteriorly bound by the ear. The mandibular region lies anterior to the masseter and inferior to the lower lip. The malar subunit is around the zygoma anterior to the masseter muscle. This subunit is referred to as the anterior region (see the image below).
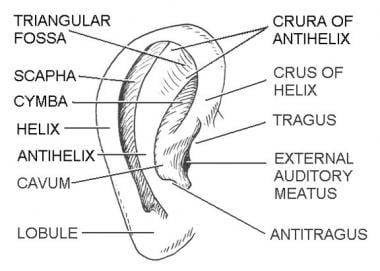
The subdivisions of the external ear allow for good clinical descriptions of skin lesions in this location (see the image below).
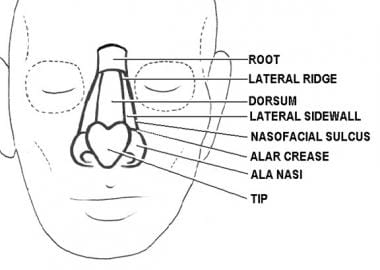
The nose [7] has the most subdivisions on the face (see the image below). The horizontal root, which borders the glabella on the forehead, is positioned superiorly. The midnose contains the dorsum medially and is flanked by the two lateral sidewalls. The dorsum is inferiorly bordered by the tip, which ends in the columella, the thin sliver of tissue that separates the nostrils on the underside of the nose. The tip is bordered by the ala nasi, or alae, on both sides, and the columella is flanked by the soft triangles, which also border the tip and the alae.
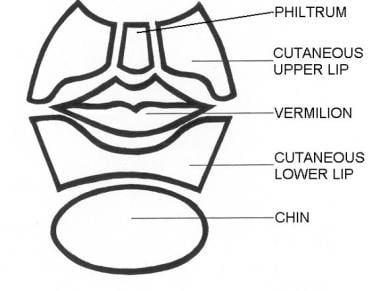
The lower part of the face is dominated by the subunits of the lip (see the image below). Below the nose, in the moustache area, are the cutaneous regions of the upper lip, which are separated from the cheek by the nasolabial fold. The middle depression below the nose, known as the philtrum, is an important anatomic subunit because even minimal displacement of this structure results in significant disfigurement. The lips constitute the vermilion subunit. The cutaneous lower lip, which borders the chin inferiorly and is bound by the nasolabial fold laterally, is below the vermillion.
Principles of reconstruction: [8, 9]
-
Reconstruction should respect cosmetic unit boundaries. For defects involving more than 50% of a subunit, replacing the entire subunit yields better results by minimizing visible scars at junctions.
-
Flaps or grafts should be designed within unit limits to maintain harmony in skin characteristics.
-
Incisions should align with natural tension lines to reduce scar visibility.
Muscles of Facial Expression
The muscles of facial expression are unique in a number of ways. Rather than inserting into bones or tendons, all the muscles of facial expression originate from or insert into the skin. They are all derived from the second embryonic branchial arch and are innervated by the seventh cranial (facial) nerve. Different anatomic areas of the face have synergistic and antagonist groups of muscles that enable individuals to make varied facial expressions. [10]
Muscles affecting the forehead and eyebrow include the frontalis muscle, which creates horizontal wrinkles on the forehead and assists with eyebrow elevation, and the corrugators and procerus muscles, which are antagonistic muscles on the forehead.
The corrugator supercilii pulls the eyebrows medially and downward, producing vertical frown lines. The procerus muscle depresses the medial eyebrow, contributing to transverse wrinkles over the nasal bridge. [11]
The orbicularis oculi is a complex muscle surrounding the eyes; it assists in closing the eyes tightly. This complex lies superficially in the eyelid skin and is encountered with even a shallow incision. The orbicularis oculi consists of orbital, palpebral, and lacrimal parts: [12]
-
The orbital part allows forceful eye closure.
-
The palpebral part facilitates gentle blinking.
-
The lacrimal part aids in tear drainage.
The dominant muscle of the nose is the nasalis muscle, which consists of nasal and alar components. Its function is to compress and dilate the nares.
Mouth muscles
The mouth has the most extensive network of facial musculature and accounts for much of an individual's capability of facial expression. The orbicularis oris encircles the mouth and is a major component of the lips. The major functions of the orbicularis oris muscle are to pull the lips against the teeth, draw the lips together, pull the corners of the mouth together, and pucker the mouth. This muscle is also extremely important for the phonation of sounds that rely on the lips such as the pronunciation of the letters M, V, F, and P. This muscle also interdigitates with adjacent muscles at the modiolus, a fibromuscular hub near the corners of the mouth, enabling complex facial expressions. [13] The modiolus serves as an important anatomical landmark for reconstructive surgeries due to its role as a convergence point for multiple muscles. [14]
A group of six muscles, collectively known as the quadratus labii superioris muscle, controls the upper mouth. These six muscles are as follows:
-
Zygomaticus major muscle - Starts from the posterolateral zygomatic bone and travels medially to insert on the upper portion of the orbicularis oris muscle; the zygomaticus major muscle helps in forming the lower nasolabial fold and is primarily responsible for smiling.
-
Zygomaticus minor muscle - Arises just medially to the zygomaticus major and assists with its functions.
-
Levator labii superioris muscle - Arises from the inferior portion of the maxilla and inserts on the upper lip, more medially than the zygomaticus muscles; the levator labii superioris muscle helps to elevate the medial part of the upper lip and assists the zygomatic muscles in open smiling (the levator and zygomaticus muscles form the nasolabial fold).
-
Levator anguli oris muscle - The most deeply positioned of the lip elevators; inserts on the upper corner of the mouth to assist with lip elevation.
-
Risorius muscle - Arises over the parotid gland, inserts into the skin and mucosa of the lateral corner of the mouth and assists with smiling; the risorius is not always present.
-
The buccinator muscle is neither an elevator nor a depressor of the lip; it arises just posterior and medial to the last molar tooth and extends forward to become continuous with the orbicularis oris muscle.
The buccinator muscle is the major component of the cheek musculature and prevents overdistension of the cheek (e.g., in playing a wind instrument). This muscle assists the orbicularis oris muscle in whistling.
The depressors of the lip, which are innervated by the marginal mandibular branch of the facial nerve (MMBFN), are as follows:
-
Depressor anguli oris muscles - Arise from the lateral part of the mandible and travel superomedially to insert, with the orbicularis oris muscle, in the corners of the mouth; they function to depress and retract the corners of the mouth.
-
Depressor labii inferioris muscles - Arise more medially on the mandible and travel superiorly to insert, with the orbicularis oris muscle, in the lower and medial part of the lip; similar to the depressor anguli oris muscle, these muscles assist with depression and retraction of the lower lip.
-
Mentalis muscle - Deep to the depressor anguli oris and labii inferioris muscles, the mentalis muscle arises from the mandible and lower lateral incisor, coursing inferiorly to insert on the skin covering the chin; the mentalis muscle elevates and wrinkles the chin and assists in protruding the lower lip.
Superficial Musculoaponeurotic System
The facial musculature must work synergistically to allow for a wide range of facial expressions. The superficial musculoaponeurotic system (SMAS) is a discrete fibromuscular layer that envelops and interlinks the muscles to provide these synergies. The SMAS delineates the dissection planes for the extensive undermining necessary in facial rejuvenation procedures.
In addition, the SMAS serves as a useful marker in assessing the location of vital blood vessels and nerves. Its superficial portion generally houses the axial blood vessels and sensory nerves, whereas the deeper levels contain the more vital motor nerves.
The SMAS is generally located beneath the subcutaneous fat and is superficial to the muscles. Superior to the zygoma, the SMAS links the temporalis, frontalis, occipitalis, and procerus muscles into a freely moveable, continuous plane that connects with the subgaleal space. Inferiorly, the fascial anatomy is unclear; however, the SMAS interconnects the platysma, risorius, and depressor anguli oris muscles inferior to the zygoma.
The muscles of the medial aspect of the face, including the orbicularis oculi, lip elevator, and nasal muscles, are not ensheathed by an interconnected SMAS.
Sensory Nerves
The trigeminal nerve, or cranial nerve (CN) V, is primarily responsible for the sensory innervation of the face. The cervical, facial, glossopharyngeal, and vagus nerves have smaller contributions. The sensory nerves are typically located more superficially than the motor nerves, along the junction of the fat and the SMAS. Transection of the sensory nerves does not result in serious morbidity that motor nerve damage causes, and the recovery of sensory function after such injury is typical.
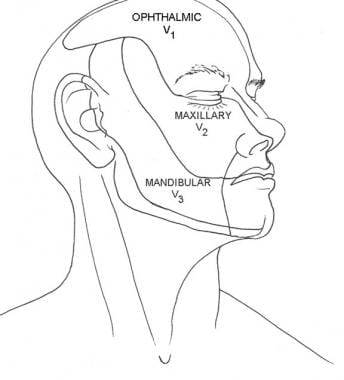
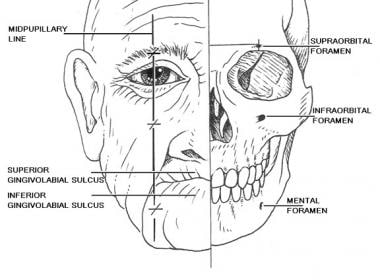
The trigeminal nerve is divided into three branches: ophthalmic (CN V1), maxillary (CN V2), and mandibular (CN V3) (see the image below).
The V1 division provides sensation to the anterior part of the scalp, forehead, upper eyelid, and nasal bridge. Branches that arise around the superior orbital rim include the supraorbital, supratrochlear, infratrochlear, external nasal, and lacrimal branches: [1]
-
Supraorbital and supratrochlear nerves - Emerge near the superior orbital rim
-
Infratrochlear nerve - Innervates the medial canthus and nasal bridge
-
External nasal branch - Supplies the nasal dorsum
-
Lacrimal branch - Innervates the lateral upper eyelid
The V2 division supplies sensation to the lower eyelid, the nasal sidewalls and columella, the temple, and the upper lip. Its major branch is the infraorbital nerve, which emerges from the infraorbital foramen with the infraorbital artery and vein. Other smaller branches include the zygomaticofacial (innervates the skin on the cheek) and zygomaticotemporal (innervates the skin on the temporal region) nerves. [1]
The V3 division is the largest and most complicated of the divisions of CN V. It is the only division that carries motor fibers. The mandibular nerves provide sensation to the lower lip, chin, mandible, and preauricular areas.
The auriculotemporal, buccal, and mental nerves are the three major cutaneous branches of the mandibular nerve. The auriculotemporal nerve sends sensory fibers to the auricles, the temples, and the temporal parietal aspect of the scalp. In addition, it provides sensation to the external auditory canals, eardrums, and temporomandibular joints, and it carries some secretory fibers to the parotid glands.
The buccal nerve is inaccessible for nerve blocks because of its deep location. It sends fibers to the cheek, mucosa, and gingiva.
The mental nerve is the continuance of the inferior alveolar nerve, and it emerges from the mental foramen on the chin. It provides sensation to the chin, lower lip, mucosa, and gingiva of the lower lip. The motor component of the trigeminal nerve primarily innervates the muscles of mastication.
The cervical plexus lies deep to the sternocleidomastoid muscle (SCM). The plexus provides sensation to several important structures and is derived from C2 through C4. These nerves include the great auricular (C2, C3), lesser occipital (C2), greater occipital (C2), third occipital (C3), transverse cervical (C2, C3), and supraclavicular nerves. They send sensory fibers to the neck, posterior part of the ear, and postauricular scalp. The spinal accessory and cervical nerves emerge near the Erb point in the posterior triangle on the neck and are easily damaged during cutaneous surgery.
Lastly, sensory branches of the vagus, glossopharyngeal, and facial nerves innervate the skin of the external auditory canal, the concha, and the posterior sulcus. Awareness of the sensory branches of the face allows the use of nerve blocks, which provide effective anesthesia with minimal discomfort for the patient. Mental, infraorbital, and supraorbital blocks are easily achieved after the identification of their respective foramina, which lie in the midpupillary plane (see the image below).
Motor Nerves
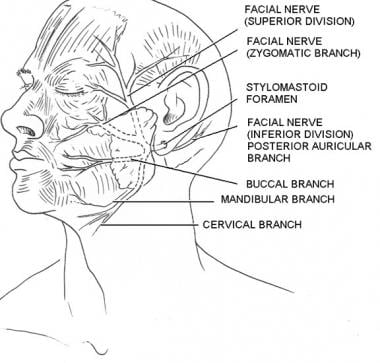
The facial nerve (CN VII, CN VII) is a mixed nerve responsible for motor, sensory, and parasympathetic functions. [1] It provides motor innervation to all the muscles of facial expression. CN VII also provides motor fibers to the digastric, stylohyoid, and stapedius muscles. In addition, sensory innervation to the anterior two thirds of the tongue, external auditory meatus, soft palate, and pharynx is mediated via the facial nerve. Additionally, it carries parasympathetic fibers to the lacrimal gland and submandibular and sublingual salivary glands. [1]
The motor portion of the facial nerve is divided into five major branches, but individual variation is common, with numerous smaller arborizations emanating from each major branch. The main facial nerve trunk emerges from the stylomastoid foramen, which is covered by the mastoid process, and along the posterior deep portion of the parotid gland. The main facial nerve trunk then divides into the following (see the image below):
-
Temporal branch
-
Zygomatic branch
-
Buccal branch
-
Mandibular branch
-
Cervical branch
Temporal branch
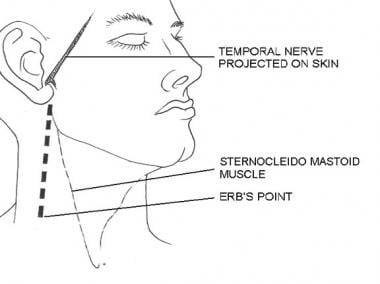
The temporal branch innervates the muscles of the upper part of the face, including the upper orbicularis oculi, frontalis, and corrugator muscles (see the image below.) This branch is extremely susceptible to inadvertent injury because it travels superficially while crossing the middle portion of the zygoma. Transection of the temporal branch most prominently leads to unilateral frontalis dysfunction, which leaves the patient with ptosis and the inability to raise his or her eyebrows.
The temporal branch emerges from the parotid gland and travels superiorly and anteriorly over the zygomatic arch. It is often located within a relatively thin layer of subcutaneous tissue, making it highly susceptible to iatrogenic injury during surgical procedures in this region such as temporal browplasty or skin surgeries near the lateral orbital area. Studies have highlighted that landmarks such as the medial zygomaticotemporal vein may serve as consistent guides for identifying and preserving this nerve during surgery. [14]
Zygomatic and buccal branches
The zygomatic branch provides motor fibers to the lower orbicularis oculi and procerus muscles and some lip elevator and nasal muscles. It typically arises from the parotid plexus after the facial nerve exits the stylomastoid foramen. Anatomical studies have shown that the zygomatic branch often divides into proximal and distal branches. The proximal branches primarily innervate the zygomaticus major muscle near its origin, while distal branches may contribute to the zygomaticobuccal plexus, forming connections with the buccal branch. In many cases, a dominant branch of the zygomatic system supplies critical motor input to midface muscles, with variability in branching patterns observed across individuals. [15, 16]
The buccal branch also originates from the parotid plexus and travels superficially over the masseter muscle and buccal fat pad. It provides motor fibers to a broader range of muscles compared with the zygomatic branch, including the buccinator, orbicularis oris, depressor anguli oris, risorius, and some lip elevators. The buccal branch often forms numerous anastomoses with the zygomatic branch within the zygomaticobuccal plexus. These interconnections contribute to redundancy in innervation, which can mitigate functional deficits following nerve injury. [16]
The buccal and zygomatic branches travel superficially over the buccal fat pad and just below the SMAS. This orientation makes them susceptible to injury during face-lift procedures. Transection of the nerves of the zygomatic and buccal branch leads to unpredictable defects because muscular innervation in the midface is variable.
Studies have highlighted significant anatomical variability in these branches. For instance, according to one study, the zygomatic branch typically has 2-4 twigs at its distal level, with one dominant twig present in 50% of cases. The buccal branch exhibits 2-5 twigs on average, with a single dominant twig identified in 66% of specimens. This variability shows the importance of careful surgical planning and intraoperative nerve identification techniques. [16]
Mandibular branch
The MMBFN is a critical motor nerve that innervates the muscles of facial expression in the lower face, including the orbicularis oris, depressor anguli oris, depressor labii inferioris, and mentalis muscles. The MMBFN originates from the inferior division of the facial nerve within the parotid gland. It runs anteriorly and inferiorly, passing below or near the inferior border of the mandible. In many cases, it lies between the platysma muscle and the investing layer of deep cervical fascia. The nerve's position relative to the mandible is highly variable: [17, 18]
-
It may be located above, at, or below the inferior border of the mandible.
-
Studies have shown that in some cases, it can extend up to 17.7 mm below the mandible on the left side and 10.8 mm on the right side, with an average distance of 7.12 ± 2.97 mm.
-
It is frequently found superficial to the facial artery and vein, making these vessels useful landmarks during surgical procedures.
The anatomic course of the marginal mandibular nerve is unpredictable, but it should be considered in any excision near the angle of the mandible and the inferior margin of the parotid gland. The MMBFN has a superficial course near the mandible and chin. This nerve usually lies anterior to the facial artery, which is palpable anterior to a clenched masseter muscle (see the image below).
Transection of the marginal mandibular nerve leads to extreme cosmetic and functional loss because the muscles of the mouth enable a significant amount of facial expression. Transection of this nerve results in a droopy lip and subsequently drooling. Excisions on the lips can also lead to drooling, but not because of the transection of a motor nerve in this location.
To minimize the risk for injury: [19]
-
Skin incisions should ideally be placed more than 2 cm below the mandible.
-
The dissection plane should remain immediately deep to the platysma but superficial to the investing layer of cervical fascia.
-
Surgeons should consider visualizing and preserving the nerve when operating within 3-4 cm of its typical course.
Contrary to earlier beliefs that the MMBFN does not form anastomoses, some studies suggest that it may have small communicating branches with other facial nerve divisions or adjacent nerves such as the mental nerve. However, these connections are inconsistent and often clinically insignificant. [20]
Cervical branch
The cervical branch is posterior and deep to the marginal mandibular nerve and innervates the platysma muscle. The cervical branch is of little importance to the cutaneous surgeon because its transection does not result in great functional or cosmetic loss.
Effects of local anesthetic
A cutaneous surgeon must be aware of the delayed effects of local anesthetics on motor fibers. Unmyelinated sensory fibers lose conduction instantaneously, whereas the deeper, myelinated motor fibers may lose their function only after a prolonged procedure with possibly greater anesthetic volume. Thus, surgeons should not be alarmed by the delayed onset of a facial muscle paralysis. This effect on the motor nerves can last as long as 12 hours, and the patient should be appropriately counseled.
Lidocaine with epinephrine prolongs the anesthetic effect due to vasoconstriction, which slows systemic absorption and clearance of the drug. [21]
Additionally, complications such as transient ischemia, blanching, or vascular effects may occur due to vasoconstrictors such as epinephrine present in the anesthetic solution. These effects are typically temporary and resolve within minutes to hours. However, rare complications such as facial nerve neuropraxia or transient complete facial paralysis have been reported following the administration of local anesthetics near facial nerve branches. These cases are usually self-limiting but highlight the importance of understanding anatomical variations and careful injection techniques to minimize risks. Proper preoperative counseling and careful administration techniques can help mitigate patient anxiety and enhance procedural outcomes. [22]
Blood Vessels
External carotid artery
The external carotid artery (ECA) provides most of the arterial blood supply to the face; the internal carotid artery makes a smaller contribution. The ECA originates from the common carotid artery at the level of the superior border of the thyroid cartilage and gives rise to several branches that vascularize the face, scalp, and neck. [23]
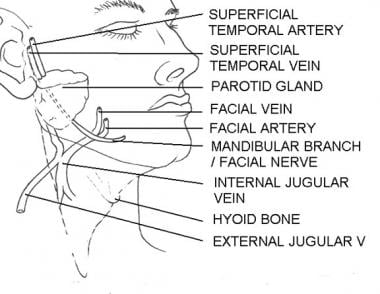
The ECA is the origin of the facial artery, deep to the mandible near the pharynx. The facial artery courses around the jaw anterior to the masseter, where it is palpable, and continues superomedially to end as the angular artery near the medial canthus. Along its path, the facial artery serves as the origin of the inferior and superior labial arteries as well as the smaller nasal branches: [24]
-
Inferior labial artery - Supplies the lower lip
-
Superior labial artery - Supplies the upper lip and nasal septum
-
Lateral nasal branch - Supplies structures such as the ala and dorsum of the nose
-
Angular artery - The terminal branch that anastomoses with branches of the ophthalmic artery from the ICA
The facial artery provides blood supply to various facial muscles and skin regions, including key anastomoses with branches of both external and internal carotid systems. Its cervical branches include the ascending palatine, tonsillar, submental, and glandular arteries. [24]
Before terminating into its two final branches — the superficial temporal artery (STA) and maxillary artery — the ECA gives rise to: [25]
-
Superior thyroid artery - Supplies the thyroid gland and adjacent structures
-
Lingual artery - Supplies blood to the tongue and floor of the mouth
-
Ascending pharyngeal artery- A small branch that supplies parts of the pharynx and surrounding areas
-
Occipital artery - Vascularizes portions of the posterior scalp
-
Posterior auricular artery - Supplies areas around and behind the ear
Superficial temporal artery
The STA arises in the parotid gland superficial to the branches of the facial nerve. The artery courses superiorly andresults in the horizontal transverse facial artery 2 cm inferior to the zygoma, which supplies blood to the scalp, forehead, and temporal regions. [26] The resultant artery connects with the facial artery. Along its course, it also gives rise to smaller branches such as the transverse facial, zygomatico-orbital, auricular, and middle temporal arteries, which supply midfacial structures and surrounding tissues. [26]
As it continues superiorly, the STA also becomes more superficial and is palpable posterior to the temporal mandibular joint and anterior to the ear. Its frontal branch supplies the forehead and anastomoses with the supraorbital and supratrochlear arteries, while its parietal branch supplies the temporal and parietal regions. These branches form numerous anastomoses with adjacent arteries such as the middle and deep temporal arteries. [27]
Anatomical variations in STA morphology are notable. Studies have documented retrocondylar or laterocondylar positioning near the mandibular condyle in most cases. Variations such as kinking or coiling along its course are common (88.4% of cases), which may pose challenges during surgical procedures. [28]
Internal maxillary artery
The internal maxillary is a deep artery that forms where the STA arises from the ECA. Because of its deep location, cutaneous surgeons rarely encounter the internal maxillary artery. Important branches of this artery include the infraorbital artery and the inferior alveolar artery, which continues through the mental foramen as the mental artery to provide blood to the chin.
Internal carotid artery
The internal carotid artery supplies arterial blood to the eyelids, the upper and dorsal parts of the nose, the lower part of the forehead, and the scalp. An important major branch of the internal carotid artery is the ophthalmic artery. The ophthalmic artery has supraorbital, supratrochlear, infratrochlear, dorsal nasal, and external nasal branches that may form anastomoses with the external carotid system through the angular artery.
Venous system
The venous network of the face parallels the arterial system. Unlike the arteries, the veins tend to be straighter and less tortuous. The facial vein parallels the facial artery and drains blood from the middle of the face into the internal jugular vein. This vein is a critical component of the venous drainage system and exhibits a predictable anatomical course. It is consistently located posterior to the facial artery, with an average distance of 6.2 mm at the inferior margin of the mandible, and takes a direct course toward the medial canthus of the eye. [29]
The venous system of the medial aspect of the face (the dangerous triangle) involves drainage of the upper lip and paranasal areas. In this area, the facial vein directly connects with the cavernous sinus via the ophthalmic vein or indirectly connects with it via the pterygoid plexus, which can facilitate the spread of infections, specifically: [30]
-
The angular vein, a tributary of the facial vein, which connects with the superior ophthalmic vein, which in turn communicates with the cavernous sinus
-
The deep facial vein, which provides an indirect route via its connection to the pterygoid venous plexus
These connections pose risks for retrograde infections from superficial areas to intracranial structures due to the absence of valves in these veins. [30]
The lateral part of the face and the scalp drain into the superficial temporal and retromandibular veins, which lead into the external jugular vein.
Studies have highlighted variations in venous anatomy. Anastomoses between right and left facial veins are common in certain regions, such as the frontal area, forming ring-shaped venous networks. The angular vein was present in nearly all the cases studied and served as a key conduit for venous drainage from areas such as the orbit. [30]
Lymphatics
Cutaneous surgeons often remove malignancies that can cause lymph node metastases. Knowledge of lymph flow is essential for an adequate clinical examination of the lymph nodes. Lymph flows from superficial areas to deep areas and then flows along four major tracts in an inferolateral direction to the collecting nodes in the neck and jaw. Considerable individual variability exists in the lymph flow; however, a general framework exists.
All the lymphatic fluid from the face eventually collects in a triangle of lymph nodes in the neck. A transverse cervical chain forms the inferior horizontal leg of the triangle, a spinal accessory chain forms the lateral leg, and an internal jugular chain forms the medial leg. The superior point of the triangle includes the superficial cervical and parotid nodes. The legs of the triangle are known as the deep lateral cervical nodes.
At the junction of the internal jugular and transverse cervical chains, the lymphatics enter the venous circulation at the jugulosubclavian junction. The spinal accessory chain travels along the spinal accessory nerve, making its removal more treacherous. This chain may be involved with early metastases from malignancies in the nasopharyngeal and thyroid areas. The transverse cervical chain is found along the transverse cervical vessels above the clavicle. The internal jugular chain is the major collection point for the head and neck, and it is divided into anterior and lateral divisions. By turning the patient's chin ipsilaterally and by rolling the relaxed SCMs between their fingers, physicians can clinically examine this group.
The postauricular node can be single or multiple, and it is located in the mastoid area attached to the insertion of the SCM. Drainage from the ear can course anteriorly to the parotid nodes or inferiorly to the spinal accessory and internal jugular chains. Superficial and deep occipital nodes drain the posterior aspect of the scalp and the nuchal area. These nodes subsequently flow into the spinal accessory chain.
The parotid nodes have extraglandular and intraglandular components. The extraglandular nodes include the preauricular and infra-auricular subnodes and are located in the parotid fascia. These nodes function as a unit with the intraglandular nodes, which are deep in the gland. The parotid nodes drain into the submandibular chain or transverse cervical chain.
The facial nodes drain the midface and are extremely variable between individuals. From superior to inferior, they are the infraorbital, malar, buccinator, and mandibular nodes. When present, these nodes are found in the subcutaneous layer above the muscles of the face. These nodes drain into the submandibular and submental chains.
The submandibular nodes are divided into five groups on the basis of their relationship with the facial vein and the submandibular gland. The preglandular nodes are below the platysma and anterior to the gland. The prevascular node is in a precarious position on the facial artery and touches the marginal mandibular nerve.
The postvascular nodes are also adjacent to the motor nerve. The existence of a retroglandular group is disputed. The submandibular gland surrounds a large group of intracapsular nodes. Many individuals have palpable nodes in the submandibular triangle. For clinical examination, the submandibular nodes can be palpated when patients relax their neck muscles and move their chin downward.
The submental nodes are located above the mylohyoid and deep to the platysma in the submental triangle. They drain the middle two thirds of the lower lip, the medial aspect of the cheek, and some facial nodes, and they can drain into the ipsilateral and contralateral nodes in the neck. Examination of the submental nodes is best accomplished by bimanually palpating the floor of the mouth and by pushing up under the patient's chin.
The superficial lateral cervical nodes receive drainage from the parotid, submandibular, and postauricular nodes. These cervical nodes are located on the superior external jugular vein, and some believe that they are part of the parotid infra-auricular nodes. The superficial lateral cervical nodes drain into the internal jugular chain.
Cutaneous Anatomy of the Neck
Muscles of the neck
The key cutaneous muscles of the neck are the platysma and SCM. The platysma is covered by the SMAS, which is continuous with the lower muscles of the face, and it is also considered a muscle of facial expression. The platysma is an extremely thin muscle that is superficial in the neck. The platysma's fibers transition from a vertical orientation in the neck to a horizontal alignment in the submandibular region, reflecting adaptations associated with bipedalism. [31]
The SCM originates from two heads: the sternal head from the manubrium of the sternum and the clavicular head from the medial third of the clavicle. These heads merge into a single belly that inserts at the mastoid process of the temporal bone and the superior nuchal line of the occipital bone. [32] The SCM divides the neck into posterior and anterior triangles.
The anterior triangle is bordered by the anterior border of the SCM, inferior border of the mandible, and midline of the neck. [1] Key components of the anterior triangle include the internal and external carotid arteries, the internal jugular vein, the vagus and hypoglossal nerves, and the suprahyoid and infrahyoid muscles. [1]
The posterior triangle is bordered by the posterior border of the SCM, anterior border of trapezius, and middle third of the clavicle. [1] A structure considered important for the posterior triangle is the spinal accessory nerve (CN XI), which innervates the sternocleidomastoid and trapezius muscles. Transection of the spinal accessory nerve results in a winged scapula and difficulty with arm abduction. Also found in the posterior triangle is the superficial cervical plexus, which has sensory, motor, and sympathetic functions.
A crucial anatomic landmark in the posterior triangle is the Erb point. The spinal accessory, great auricular, lesser occipital, and transverse cervical nerves all pass within 2 cm above or below this location. The Erb point can be located by drawing a line between the angle of the mandible and the mastoid process with the patient's head slightly turned. The Erb point lies at the junction of the posterior border of the SCM and a point 6 cm inferior to the midpoint of the line drawn (see the image below).
Blood vessels of the neck
The key blood vessels of the neck include the common and external carotid arteries and the jugular veins. The common carotid, internal jugular, and vagus nerves are found in the carotid sheath under the sternocleidomastoid and infrahyoid muscles before the carotid arteries bifurcate into their external and internal branches.
The external jugular vein forms below the parotid gland and travels inferiorly along the surface of the SCM. This vein empties into the subclavian or internal jugular veins after piercing through the superficial portion of the deep cervical fascia in the posterior triangle.
Skin tension lines
STLs typically lie in a transverse direction on the neck. The placement of excision lines in this orientation is essential because hypertrophic or reddened scars often result from misplaced excisions on the neck.
Anatomic Surgical Considerations
Free margins are located on the eyelids, helices of the ears, lips, and alar rim and columella. Unopposed tension caused by surgical repair may distort these structures. Wound closure in these locations often requires flap and/or graft placement to lower the risk. [33]
When designing flaps, borrow tissue from the same or adjacent cosmetic units to minimize anatomic distortion and maximize tissue match.
A reservoir of skin for flaps or primary closure can be found on the lower and posterior part of the cheek near the angle of the mandible. In older people, this area is the jowl. Other areas with redundant skin include the preauricular aspect of the cheek, the temple, and the neck.
Place the suture lines along STLs and on the boundaries of the cosmetic units whenever possible. Preoperatively identify the vital structures that might be damaged in the operative field, and stay vigilant to avoid them. Examples of vital structures include the temporal nerve in the upper part of the cheek and temple, the marginal mandibular nerve on the jaw line, and CN XI at the Erb point.
Identify sensory innervation to structures in the operative field, and perform a nerve block wherever possible to minimize the patient's discomfort and distortion of the operative field by using large amounts of lidocaine. Examples of sensory innervations include the mental nerve on the chin and the supraorbital and supratrochlear nerves in large lesions on the forehead.
When working in deeper planes, attempt to identify the SMAS, which can help in locating and avoiding vital vessels and nerves.
Studies emphasize understanding facial glide planes and retaining ligaments for advanced surgical techniques such as facelifts. Glide planes allow for safe mobilization of soft tissues without excessive tension, while retaining ligaments provides structural support that must be preserved or released judiciously during surgery to achieve optimal redraping of tissues. [34]
-
Skin tension lines. Illustrated by Charles Norman.
-
Cosmetic subunits. Illustrated by Charles Norman.
-
Forehead subunits. Illustrated by Charles Norman.
-
Eyelid subunits. Illustrated by Charles Norman.
-
Subunits of the anterior region. Illustrated by Charles Norman.
-
Subunits of the ear. Illustrated by Charles Norman.
-
Subunits of the nose. Illustrated by Charles Norman.
-
Subunits of the lower part of the face. Illustrated by Charles Norman.
-
Distribution of cranial nerve V. Illustrated by Charles Norman.
-
Foramina for nerve blocks. Illustrated by Charles Norman.
-
Branches of the facial nerve. Illustrated by Charles Norman.
-
Course of the temporal nerve and location of the Erb point. Illustrated by Charles Norman.
-
Course of the marginal mandibular nerve. Illustrated by Charles Norman.