Practice Essentials
Low back pain (LBP) is ubiquitous. An estimated 30-45% of persons aged 18-55 years have some form of back pain in their lifetime. LBP most commonly involves one of the following conditions: sciatic nerve entrapment, herniated nucleus pulposus, direct trauma, muscle spasm due to chronic or overuse injury, or piriformis syndrome.
Piriformis syndrome (see the image below) is characterized by pain and instability. The location of the pain is often imprecise, but it is often present in the hip, coccyx, buttock, groin, or distal part of the leg. The history and physical findings are key elements in differentiating the more common forms of LBP and piriformis syndrome. The literature and general knowledge on piriformis syndrome are limited compared with those on sciatica or disc herniation. However, the common findings associated with piriformis syndrome are agreed upon.
In most cases, conservative treatment (eg, stretching, manual techniques, injections, activity modifications, natural healing, modalities such as heat and ultrasound) is successful in managing piriformis syndrome.
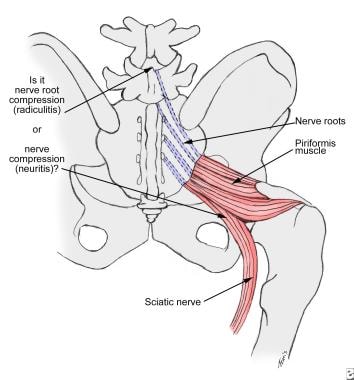 Nerve irritation in the herniated disc occurs at the root (sciatic radiculitis). In piriformis syndrome, the irritation extends to the full thickness of the nerve (sciatic neuritis).
Nerve irritation in the herniated disc occurs at the root (sciatic radiculitis). In piriformis syndrome, the irritation extends to the full thickness of the nerve (sciatic neuritis).
Epidemiology
United States statistics
In one study at a regional hospital, 45 of 750 patients (6%) with LBP were found to have piriformis syndrome. Another author estimated that the incidence of piriformis syndrome in patients with sciatica is also 6%. The overall incidence of piriformis syndrome has been estimated at 2.4 million per year. Most cases occur in middle-aged patients. [1]
Sex
The female-to-male incidence ratio of piriformis syndrome is 6:1.
Functional Anatomy
The function of the piriformis muscle is to externally rotate and abduct the thigh. The sacral plexus is closely associated with the anterior surface of the piriformis muscle. The lumbosacral trunk and the ventral rami of the first three sacral nerves form the sacral plexus. The sciatic nerve passes inferior to the piriformis muscle.
The sciatic nerve exits the pelvis via four routes:
-
The nerve passes anteriorly to the piriformis between the rims of the greater sciatic foramen
-
The peroneal portion of the sciatic nerve passes through the piriformis; the tibial portion passes anterior to the piriformis muscle
-
The peroneal branch of the sciatic nerve loops above and posterior to the piriformis muscle, whereas the tibial branch passes anterior to the piriformis muscle
-
The undivided sciatic nerve penetrates the piriformis muscle
Dysfunction of the piriformis muscle can cause signs and symptoms of pain in the sciatic nerve distribution, that is, in the gluteal area, posterior thigh, posterior leg, and lateral aspect of the foot. [2]
A cadaver study by Iwanaga et al indicated that the superior gluteal nerve is an important source of piriformis muscle innervation. Of 20 sides from 10 cadavers studied, the investigators found that in 80%, the piriformis muscle was innervated by 2-3 nerves. Nerves originated from the superior gluteal nerve on 14 sides (70%); from the inferior gluteal nerve on one side (5%); from the L5 ventral ramus on one side (5%); from the S1 ventral ramus on 17 sides (85%); and from the S2 ventral ramus on 14 sides (70%). [3]
Etiology
Although no general consensus about the etiology and pathophysiology of piriformis syndrome exists, many physicians and physical therapists attribute this syndrome to a specific mechanism involving the sciatic nerve.
Papadopoulos and colleagues proposed the following classifications for piriformis syndrome [4] :
-
Primary piriformis syndrome - This designation would apply to piriformis syndrome resulting from intrinsic pathology of the piriformis muscle itself, such as myofascial pain, anatomic variations, and myositis ossificans
-
Secondary piriformis syndrome (pelvic outlet syndrome) - This classification would encompass all other etiologies of piriformis syndrome, with the exclusion of lumbar spinal pathology
The etiology of piriformis syndrome can be divided into the following categories:
-
Hyperlordosis
-
Muscle anomalies with hypertrophy
-
Fibrosis (due to trauma)
-
Partial or total nerve anatomic abnormalities
Other causes of piriformis syndrome can include the following:
-
Pseudoaneurysms of the inferior gluteal artery adjacent to the piriformis muscle
-
Bilateral piriformis syndrome due to prolonged sitting
-
Cerebral palsy
-
Total hip arthroplasty
-
Fibrodysplasia ossificans progressiva (myositis ossificans)
-
Vigorous physical activity
-
Leg length discrepancy [5]
Piriformis syndrome can be secondary to inflammation due to gluteal trauma or spasm, with trauma to the buttocks or gluteal region being the most common cause of the syndrome. The effect of this inflammatory process on the sciatic nerve is chemical rather than mechanical.
Skiers, truck drivers, tennis players, and long-distance bikers are at high risk for piriformis syndrome.
Several theories suggest that the following are key factors in the muscle hyperfunction or spasm that leads to an interstitial myofibrositis: extravasation of blood, release of serotonin from platelets, and prostaglandin E, serotonin, bradykinin, and histamine release.
Benson and Schutzer attributed the syndrome to blunt trauma to the buttocks that results in hematoma formation and subsequent scarring between the sciatic nerve and the short external rotators. [6]
Entrapment of the sciatic nerve at the sciatic trunk (where it leaves the pelvis and crosses the greater sciatic notch) is an infrequent cause. This entrapment can occur as a result of an enlarged, hypertrophic piriformis; an inflamed piriformis muscle; tumors; cysts; and pseudoaneurysms.
A Morton foot may predispose the patient to developing piriformis syndrome. The prominent second metatarsal head destabilizes the foot during the push-off phase of the gait cycle, causing foot pronation and internal rotation of the lower limb. As a compensatory mechanism, the piriformis muscle (external hip rotator) reactively contracts repetitively during each push-off phase of the gait cycle, leading to piriformis syndrome.
Spinal stenosis can lead to bilateral piriformis tenderness.
Anatomic variations of the divisions of the sciatic nerve above, below, and through the belly of the piriformis muscle may be causative factors. [7]
Prognosis
Piriformis syndrome is not life-threatening, but it can have significant associated morbidity. As calculated for 2016, LBP in general was estimated to have an annual direct cost in the United States of $78.69 billion, and an annual indirect cost of $445.84 billion. [8]
Most patients with piriformis syndrome progress well after a local trigger-point injection. Recurrences are uncommon after 6 weeks of therapy. Following surgery, patients treated with piriformis release return to their activities in an average of 2-3 months.
-
Nerve irritation in the herniated disc occurs at the root (sciatic radiculitis). In piriformis syndrome, the irritation extends to the full thickness of the nerve (sciatic neuritis).

