Background
Mechanical low back pain (LBP) is low back pain associated with the spine, intervertebral disks, or surrounding soft tissues. [1] It generally results from an acute traumatic event but may also be caused by cumulative trauma. [2] The severity of an acute traumatic event varies widely, from twisting one's back to being involved in a motor vehicle collision. Mechanical LBP due to cumulative trauma tends to occur more commonly in the workplace.
Mechanical LBP remains the second most common symptom-related reason for seeing a physician in the United States. Of the US population, 85% will experience an episode of mechanical LBP at some point during their lifetime. Fortunately, the LBP resolves for the vast majority within 2-4 weeks. [3]
The image below illustrates a herniated nucleus pulposus at multiple levels, one of the causes of LBP.
 Magnetic resonance image of the lumbar spine. This image demonstrates a herniated nucleus pulposus at multiple levels.
Magnetic resonance image of the lumbar spine. This image demonstrates a herniated nucleus pulposus at multiple levels.
For individuals younger than 45 years, mechanical LBP represents the most common cause of disability and is generally associated with a work-related injury. For individuals older than 45 years, mechanical LBP is the third most common cause of disability, and a careful history and physical examination are vital to evaluation, treatment, and management. [4]
Evidence-based clinical practices on selected rehabilitation interventions for LBP have focused on the timing of interventions.
-
Acute LBP is defined as pain that does not radiate below the knees, with current symptoms that have been present for 4-6 weeks or less
-
Subacute LBP is defined as pain that does not radiate below the knees, with current symptoms that have been present for 4-12 weeks from onset
-
Chronic LBP is defined as pain that does not radiate below the knees, with current symptoms that have been present for greater than 12 weeks
Numerous treatment guidelines have been written regarding the evaluation, treatment, and management of LBP. [5, 6] Perhaps the most widely reviewed (and controversial) guideline was published in 1994 by the Agency for Health Care Policy and Research and titled "Acute Lower Back Problems in Adults: Clinical Practice Guidelines." [7]
At the beginning of the 21st century, 750 national and international organizations partnered to create the Bone and Joint Decade (2002-2011). [8] This initiative involved patient and professional health care organizations, government agencies, and industries working collaboratively to increase the awareness of bone and joint diseases while increasing the information and research to address this major health care issue. Because 1 in 5 Americans will be age 65 or older by 2030, 65 million people (20% of the total population) will be affected by musculoskeletal impairments, with LBP ranking among the most common problems.
The physiatrist represents one type of medical specialist who can evaluate, diagnose, treat, and manage LBP by using medical and nonsurgical procedures and interventions. The physiatrist may have the best functional understanding of all specialists in the treatment and management of mechanical LBP. [9, 10]
Lambeek et al assessed the efficacy of an integrated care program for chronic LBP against that of a more conventional care program, as a means of helping patients with this condition return to work. In the study, 66 patients received integrated care from a team made up of a clinical occupational physician, a physical therapist, an occupational therapist, and a medical specialist. Treatment included workplace intervention involving participatory ergonomics, as well as a graded activity program. Another 68 patients received the usual type of care for chronic back pain, administered by a medical specialist, a general practitioner, an occupational physician, and/or allied health care professionals.
Members of the integrated care group achieved a full, sustainable return to work in a median period of 88 days, while the same was accomplished in the conventional care group after a median 208 days. By 12-month follow-up, the integrated care group had experienced significantly greater improvement in functional status than had the conventional care patients. However, the investigators found no significant difference in pain reduction between the 2 groups at 12 months. [11]
Pathophysiology
Mechanical LBP generally results from an acute traumatic event, but it may also be caused by cumulative trauma. [2] The severity of an acute traumatic event varies widely, from twisting one's back to being involved in a motor vehicle collision. Mechanical LBP due to cumulative trauma tends to occur more commonly in the workplace.
Using data from the 2015 National Health Interview Survey, a study by Peng et al indicated that overweight and obesity are risk factors for LBP. Compared with persons of normal weight, the adjusted odds ratios for LBP in persons with overweight or obesity were 1.21 and 1.55, respectively. However, the link between body mass index and LBP appeared to be impacted by sex and race/ethnicity. For example, the adjusted odds ratios for non-White men and women of normal weight were lower than the LBP risk for normal-weight White men. [12]
(Nonetheless, according to 2023 guidelines from the World Health Organization [WHO] on the non-surgical management of chronic primary LBP (CPLBP) in adults in primary and community care settings, routine care for adults, including older people, with CPLBP should not include pharmacologic weight loss. [13] )
In a systematic study review, Chen et al investigated whether a sedentary lifestyle (which the authors defined as including sitting for prolonged periods at work and during leisure time) is a risk factor for LBP. [14] Examining journal articles published between 1998 and 2006, they identified 8 high-quality reports (6 prospective cohort and 2 case-control studies). While 1 of the cohort studies reported a link between sitting at work and the development of LBP, the other investigations did not find a significant connection between a sedentary lifestyle and LBP. Chen and coauthors concluded that a sedentary lifestyle alone does not lead to LBP.
In a birth cohort study from 1980-2008, Rivinoja et al investigated whether lifestyle factors, such as smoking, being overweight or obese, and participating in sports, at age 14 years would predict hospitalizations in adulthood for LBP and sciatica. [15] The authors found that 119 females and 254 males had been hospitalized at least once because of LBP or sciatica. Females who were overweight had an increased risk of second-time hospitalization and surgery. Smoking in males was linked with an increased risk of first-time nonsurgical hospitalization and second-time hospitalization for surgical treatment.
Similarly, a study by Yang and Haldeman, derived from the 2009-2012 National Health Interview Survey of the civilian US population, indicated that risk factors for LBP include current or previous smoking, current or previous alcohol use, lack of sleep, obesity, and lack of leisure-time physical activity. [16]
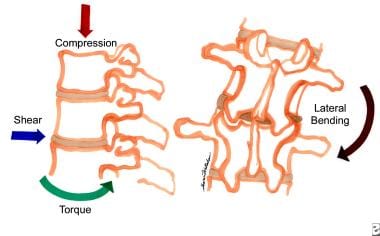
The pathophysiology of mechanical LBP remains complex and multifaceted. Multiple anatomic structures and elements of the lumbar spine (eg, bones, ligaments, tendons, disks, muscle) are all suspected to have a role. (See the images below.) Many of these components of the lumbar spine have sensory innervation that can generate nociceptive signals representing responses to tissue-damaging stimuli. Other causes could be neuropathic (eg, sciatica). Most chronic LBP cases most likely involve mixed nociceptive and neuropathic etiologies.
 Degenerative changes of the lumbar spine, including decreased signal intensity and disk bulging at the L-3/4, L-4/5 and L-5/S-1 disks.
Degenerative changes of the lumbar spine, including decreased signal intensity and disk bulging at the L-3/4, L-4/5 and L-5/S-1 disks.
Biomechanically, the movements of the lumbar spine consist of the cumulative motions of the vertebrae, with 80-90% of the lumbar flexion/extension occurring at the L4-L5 and L5-S1 intervertebral disks. The lumbar spine positions most at risk for producing LBP is forward flexion (bent forward), rotation (trunk twisted), and attempting to lift a heavy object with outstretched hands. Axial loading of short duration is resisted by annular collagen fibers in the disk. Axial loading of a longer duration creates pressure to the annulus fibrosus and increased pressure to the endplates. If the annulus and endplate are intact, the loading forces can be adequately resisted. However, compressive muscular forces may combine with the loading forces to increase intradiskal pressure that exceeds the strength of the annular fibers.
Repetitive, compressive loading of the disks in flexion (eg, lifting) puts the disks at risk for an annular tear and internal disk disruption. Likewise, torsional forces on the disks can produce shear forces that may induce annular tears. (Degenerative disk forces are demonstrated in the image below.) The contents of the annulus fibrosus (the nucleus pulposus) may leak through these tears. Central fibers of the disk are pain free, so early tears may not be painful. Samples of disk material taken at the time of autopsy reveal that the cross-linked profile of pentosidine, a component of the collagen matrix, declines. This may indicate the presence of increased matrix turnover and tissue remodeling.
In lumbar flexion, the highest strains are recorded within the interspinous and supraspinous ligaments, followed by the intracapsular ligaments and the ligamentum flavum. In lumbar extension, the anterior longitudinal ligament experiences the highest strain. Lateral bending produces the highest strains in the ligaments contralateral to the direction of bending. Rotation generates the highest strains in the capsular ligaments.
A review study by Raastad et al of radiographic features in patients with LBP found that in community- and occupation-based studies, such pain was significantly associated with disk-space narrowing. LBP was also significantly linked with the presence of spondylolisthesis, but in occupation-based studies only. The review, which involved 28 studies (26,107 subjects total), also indicated that LBP has only a weak association with spondylosis and osteophytes and a nonsignificant association with endplate sclerosis. [17]
Research since the late 20th century suggests that chemical causes may play a role in the production of mechanical LBP. Components of the nucleus pulposus, most notably the enzyme phospholipase A2 (PLA2), have been identified in surgically removed herniated disk material. PLA2 may act directly on neural tissue, or it may orchestrate a complex inflammatory response that manifests as LBP.
Glutamate, a neuroexcitatory transmitter, has been identified in degenerated disk proteoglycan and has been found to diffuse to the dorsal root ganglion (DRG) affecting glutamate receptors. Substance P (pain) is present in afferent neurons, including the DRG, and is released in response to noxious stimuli, such as vibration and mechanical compression of the nerve. Steady, cyclic, or vibratory loading induces laxity and creep in the viscoelastic structures of the spinal elements. This creep does not recover fully in the in vivo cat model, even when rest periods are equal in duration to the loading period.
The concept of a biomechanical degenerative spiral has an appealing quality and is gaining wider acceptance. This concept postulates that the breakdown of the annular fibers allows PLA2 and glutamate, and possibly other, as-yet unknown compounds, to leak into the epidural space and diffuse to the DRG. The weakened vertebra and disk segment become more susceptible to vibration and physical overload, resulting in compression of the DRG and stimulating the release of substance P. Substance P, in turn, stimulates histamine and leukotriene release, leading to an altering of nerve impulse transmission. The neurons become sensitized further to mechanical stimulation, possibly causing ischemia, which attracts polymorphonuclear cells and monocytes to areas that facilitate further disk degeneration and produce more pain.
A study by Baumbauer et al indicated that a link exists between the COMT rs4680 genotype (GG) and the transition from acute to chronic LBP. In addition, an independent association with such transition was seen with COMT expression. [18]
Epidemiology
Frequency
United States
The lifetime prevalence of mechanical low back pain (LBP) in the United States is 60-80%. The prevalence of serious mechanical LBP (persisting >2 wk) is 14%. The prevalence of true sciatica (pain radiating down one or both legs) is approximately 2%.
Of all cases of mechanical LBP, 70% are due to lumbar strain or sprain, 10% are due to age-related degenerative changes in disks and facets, 4% are due to herniated disks, 4% are due to osteoporotic compression fractures, and 3% are due to spinal stenosis. All other causes account for less than 1% of cases.
Mechanical LBP is the most common cause of work-related disability in persons younger than 45 years in the United States.
International
Mechanical LBP exists in every culture and country. Worldwide, more disability is caused by LBP than by any other condition, as measured in years lived with disability (YLDs). [19, 20, 21] A report by Hurwitz et al stated that in 2015, LBP of over 3 months’ duration was experienced by more than 500 million people globally. That year, LBP and neck pain together accounted for the fourth highest number of disability-adjusted life years (DALYs) worldwide, behind ischemic heart disease, cerebrovascular disease, and lower respiratory infection. The report concluded that the prevalence of LBP and neck pain had risen since the late 20th century and will probably keep on increasing in response to aging populations. [22]
Estimates by numerous investigators indicate that at some point in their lives, 80% of all human beings experience LBP.
Mechanical LBP is more prevalent in countries with higher per capita income and where more liberal policies and adequate funds provide for compensation (eg, Germany, Sweden, Belgium).
In Sweden, the level of insurance benefits for disabling LBP is 100%, compared with a range of 0-80% in the United States. In 1987, the percentage of the work force placed on a sick list for diagnoses associated with back pain was 8% in Sweden versus 2% in the United States. In the same year, the average number of days of back-related absence from work per patient per year in Sweden was 40, versus 9 in the United States.
Mortality/Morbidity
While mechanical LBP is not associated with mortality, morbidity in terms of lost productivity, use of medical services, and cost to society is staggering. Health-care spending in the United States for low back and neck pain was estimated to be $134.5 billion in 2016, the highest amount among 154 conditions. [23] Indeed, total annual health-care costs for LBP in the United States run from $100-$200 billion. [24]
Race
No published information suggests that race is a factor in the prevalence of mechanical LBP.
Sex
The impact of sex on the prevalence of LBP has not been established as well as have the roles of other risk factors in LBP (eg, previous LBP, age). A reported 50-90% of women develop symptoms of LBP in the course of pregnancy. Discomfort generally develops in the very early weeks, more commonly in the third trimester. Age, race, occupation, baby's weight, prepregnancy maternal weight, weight gain, number of children, exercise habits, sleeping posture, mattress type, and history of previous LBP have not shown any correlation with the development of LBP symptoms during pregnancy.
Age
Age has been shown to be associated more consistently with mechanical LBP than has sex. The prevalence of LBP during pregnancy appears to increase 5% for every 5 years of patient age. Sciatica (pain that radiates down one or both legs) is usually reported in persons aged 40-59 years. Women aged 60 years or older also report more low back symptoms.
Patient Education
Patient education should begin with reassurance and a management plan, even though a precise pathoanatomic diagnosis may not be possible.
The importance of educating patients to understand that uncomplicated mechanical LBP has a natural course of recovery cannot be overemphasized.
One consistent finding from a review of the literature is that people who are depressed, have poor job satisfaction, and can receive compensation as long as their backs hurt have an increased prevalence of mechanical LBP that develops into chronic disability.
Deal with external factors that influence recovery, including anxiety, and increase the patient's understanding of the expectations of key players (eg, family, physician, employer) compared with his or her own goals.
Posture, reconditioning, proper nutrition, and stress management also should be addressed.
For further patient education, see the patient education article Low Back Pain.
-
Magnetic resonance image of the lumbar spine. This image demonstrates a herniated nucleus pulposus at multiple levels.
-
Diskogram showing examples of an intact disk and a disrupted disk at the lumbar level.
-
Sagittal magnetic resonance image showing loss of intervertebral disk height at L5/S1. Herniations of the nucleus pulposus are noted at L4/5 and L5/S1.
-
Degenerative changes of the lumbar spine, including decreased signal intensity and disk bulging at the L-3/4, L-4/5 and L-5/S-1 disks.
-
The process of disk degeneration following internal disk disruption and herniation.
-
The various forces placed on the disks of the lumbar spine that can result in degenerative changes.