Practice Essentials
Hydrocephalus, also known as a hydrodynamic CSF disorder, is broadly defined as a disturbance of cerebrospinal fluid (CSF) formation, flow, or absorption, leading to an increase in volume occupied by this fluid in the central nervous system (CNS). [1, 2] (See the image below.)
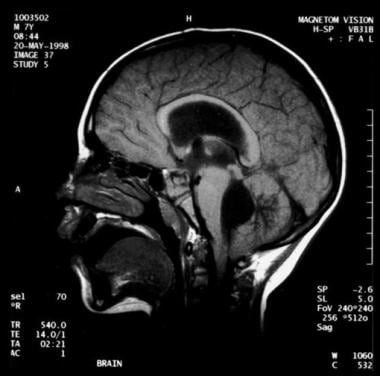 Noncommunicating obstructive hydrocephalus caused by obstruction of the foramina of Luschka and Magendie. This MRI sagittal image demonstrates dilatation of lateral ventricles with stretching of corpus callosum and dilatation of the fourth ventricle.
Noncommunicating obstructive hydrocephalus caused by obstruction of the foramina of Luschka and Magendie. This MRI sagittal image demonstrates dilatation of lateral ventricles with stretching of corpus callosum and dilatation of the fourth ventricle.
Signs and symptoms
Clinical features of hydrocephalus are influenced by the patient's age, the cause of the hydrocephalus, the location of the obstruction, its duration, and its rapidity of onset. [2]
Symptoms in infants include poor feeding, irritability, reduced activity, and vomiting.
Symptoms in children and adults include the following:
-
Slowing of mental capacity, cognitive deterioration
-
Headaches (initially in the morning)
-
Neck pain, suggesting tonsillar herniation
-
Vomiting, more significant in the morning
-
Blurred vision: A consequence of papilledema and, later, of optic atrophy
-
Double vision: Related to unilateral or bilateral sixth nerve palsy
-
Difficulty in walking secondary to spasticity: Preferentially affects the lower limbs because the periventricular pyramidal tract is stretched by the hydrocephalus
-
Drowsiness
Children may also exhibit stunted growth and sexual maturation from third ventricle dilatation. Adults may also have nausea that is not exacerbated by head movements; incontinence (urinary first, fecal later if condition remains untreated) indicates significant destruction of the frontal lobes and advanced disease.
Background
Hydrocephalus, also known as a hydrodynamic cerebrospinal fluid (CSF) disorder, is broadly defined as a disturbance of formation, flow, or absorption of CSF that leads to an increase in volume occupied by this fluid in the CNS. [1, 2] Acute hydrocephalus occurs over days, subacute hydrocephalus occurs over weeks, and chronic hydrocephalus occurs over months or years. Conditions such as cerebral atrophy and focal destructive lesions also lead to an abnormal increase of CSF in CNS. In these situations, loss of cerebral tissue leaves a vacant space that is filled passively with CSF. Such conditions are not the result of a hydrodynamic disorder and therefore are not classified as hydrocephalus.
Benign external hydrocephalus (benign enlargement of the subarrachnoid spaces of infancy) is a self-limiting absorption deficiency of infancy and early childhood with mildly raised intracranial pressure (ICP) and enlarged subarachnoid spaces. The ventricles usually are not enlarged significantly, and resolution within 1 year is the rule. [6]
Communicating hydrocephalus occurs when full communication occurs between the ventricles and subarachnoid space. It is caused by overproduction of CSF (rarely), defective absorption of CSF (most often, includes conditions such as intracranial hemorrhage or meningitis resulting in damage to the arachnoid granulations, where CSF is reabsorbed), or venous drainage insufficiency (occasionally). (See the image below.)
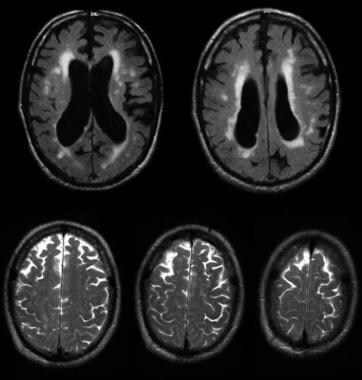 Communicating hydrocephalus with surrounding "atrophy" and increased periventricular and deep white matter signal on fluid-attenuated inversion recovery (FLAIR) sequences. Note that apical cuts (lower row) do not show enlargement of the sulci, as is expected in generalized atrophy. Pathological evaluation of this brain demonstrated hydrocephalus with no microvascular pathology corresponding with the signal abnormality (which likely reflects transependymal exudate) and normal brain weight (indicating that the sulci enlargement was due to increased subarachnoid cerebrospinal fluid [CSF] conveying a pseudoatrophic brain pattern).
Communicating hydrocephalus with surrounding "atrophy" and increased periventricular and deep white matter signal on fluid-attenuated inversion recovery (FLAIR) sequences. Note that apical cuts (lower row) do not show enlargement of the sulci, as is expected in generalized atrophy. Pathological evaluation of this brain demonstrated hydrocephalus with no microvascular pathology corresponding with the signal abnormality (which likely reflects transependymal exudate) and normal brain weight (indicating that the sulci enlargement was due to increased subarachnoid cerebrospinal fluid [CSF] conveying a pseudoatrophic brain pattern).
Noncommunicating hydrocephalus occurs when CSF flow is obstructed within the ventricular system or in its outlets to the arachnoid space, resulting in impairment of the CSF from the ventricular to the subarachnoid space. The most common form of noncommunicating hydrocephalus is obstructive and is caused by intraventricular or extraventricular mass-occupying lesions that disrupt the ventricular anatomy. [7] (See the images below.)
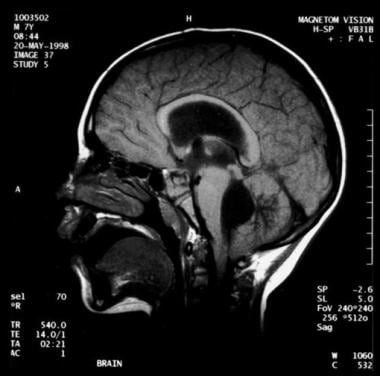 Noncommunicating obstructive hydrocephalus caused by obstruction of the foramina of Luschka and Magendie. This MRI sagittal image demonstrates dilatation of lateral ventricles with stretching of corpus callosum and dilatation of the fourth ventricle.
Noncommunicating obstructive hydrocephalus caused by obstruction of the foramina of Luschka and Magendie. This MRI sagittal image demonstrates dilatation of lateral ventricles with stretching of corpus callosum and dilatation of the fourth ventricle.
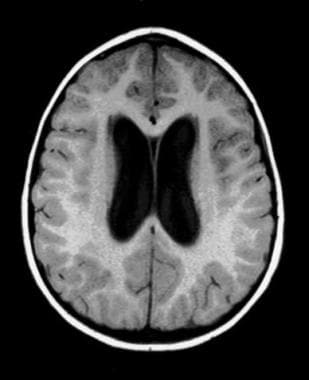 Noncommunicating obstructive hydrocephalus caused by obstruction of foramina of Luschka and Magendie. This MRI axial image demonstrates dilatation of the lateral ventricles.
Noncommunicating obstructive hydrocephalus caused by obstruction of foramina of Luschka and Magendie. This MRI axial image demonstrates dilatation of the lateral ventricles.
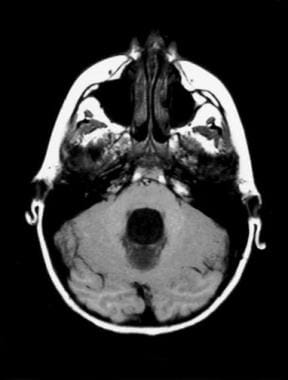 Noncommunicating obstructive hydrocephalus caused by obstruction of foramina of Luschka and Magendie. This MRI axial image demonstrates fourth ventricle dilatation.
Noncommunicating obstructive hydrocephalus caused by obstruction of foramina of Luschka and Magendie. This MRI axial image demonstrates fourth ventricle dilatation.
Congenital hydrocephalus applies to the ventriculomegaly that develops in the fetal and infancy periods, often associated with macrocephaly. [8] The most common causes of congenital hydrocephalus are obstruction of the cerebral aqueduct flow, Arnold-Chiari malformation or Dandy–Walker malformation. [9] These patients may stabilize in later years due to compensatory mechanisms but may decompensate, especially following minor head injuries. During these decompensations, determining the extent to which any new neurological deficits may be due to the new acute event, compared with hydrocephalus that may have gone unnoticed for many years, is difficult. An extremely severe variant of congenital hydrocephalus is hydranencephaly, where the brain's cerebral hemispheres are absent to varying degrees and the remaining cranial cavity is filled with CSF.
Normal pressure hydrocephalus (NPH) is a rare condition characterized by abnormal gait, urinary incontinence, and (potentially reversible) dementia. It can occur in persons of any age but is most common in older adults. See the Medscape article Normal Pressure Hydrocephalus for more information.
Pathophysiology
Normal CSF production is 0.20–0.35 mL/min; most CSF is produced by the choroid plexus, which is located within the ventricular system, mainly the lateral and fourth ventricles. The capacity of the lateral and third ventricles in a healthy person is 20 mL. Total volume of CSF in an adult is 120 mL.
Normal route of CSF from production to clearance is the following: From the choroid plexus, the CSF flows to the lateral ventricle, then to the interventricular foramen of Monro, the third ventricle, the cerebral aqueduct of Sylvius, the fourth ventricle, the two lateral foramina of Luschka and one medial foramen of Magendie, the subarachnoid space, the arachnoid granulations, the dural sinus, and finally into the venous drainage.
ICP rises if production of CSF exceeds absorption. This occurs if CSF is overproduced, resistance to CSF flow is increased, CSF resorption is decreased, or venous sinus pressure is increased. CSF production falls as ICP rises. Compensation may occur through transventricular absorption (subependymal flow) of CSF and also by absorption along nerve root sleeves (which may result in enlarged optic nerve sheaths). The temporal and frontal horns dilate first, often asymmetrically. This may result in elevation of the corpus callosum, stretching or perforation of the septum pellucidum, thinning of the cerebral mantle, or enlargement of the third ventricle downward into the pituitary fossa (which may cause pituitary dysfunction) as well as dorsal midbrain compression resulting in Parinaud's syndrome (aralysis of upgaze, Pseudo-Argyll Roberson pupils, convergence-retraction nystagmus, eyelide retraction, and setting sun sign).
Mortality/Morbidity
In untreated hydrocephalus, death may occur by tonsillar herniation secondary to raised ICP with compression of the brain stem and subsequent respiratory arrest.
Shunt dependence occurs in 75% of all cases of treated hydrocephalus and in 50% of children with communicating hydrocephalus. Patients are hospitalized for scheduled shunt revisions or for treatment of shunt complications or shunt failure. Poor development of cognitive function in infants and children, or loss of cognitive function in adults, can complicate untreated hydrocephalus. It may persist after treatment. Visual loss can complicate untreated hydrocephalus and may persist after treatment.
Epidemiology
Frequency
The global prevalence of hydrocephalus is estimated at approximately 85 cases per 100,000 individuals, with notable variation across age groups: 88 per 100,000 in the pediatric population and 11 per 100,000 in adults. [10]
Demographics
Generally, incidence is equal in males and females. The exception is Bickers-Adams syndrome (X-linked hydrocephalus with stenosis of aqueduct of Sylvius), transmitted by females and manifested in males. NPH has a slight male preponderance.
Incidence of human hydrocephalus presents a bimodal age curve. One peak occurs in infancy and is related to the various forms of congenital malformations and premature birth. Another peak occurs in adulthood, mostly resulting from NPH. Adult hydrocephalus represents approximately 40% of total cases of hydrocephalus.
The outcome of pediatric hydrocephalus has been studied frequently, but much remains unresolved about long-term and social outcomes. [11]
Prognosis
Long-term outcome is related directly to the cause of hydrocephalus.
Up to 50% of patients with large intraventricular hemorrhage develop permanent hydrocephalus requiring shunt.
Following removal of a posterior fossa tumor in children, 20% develop permanent hydrocephalus requiring a shunt. The overall prognosis is related to type, location, and extent of surgical resection of the tumor.
Satisfactory control was reported for medical treatment in 50% of hydrocephalic patients younger than 1 year who had stable vital signs, normal renal function, and no symptoms of elevated ICP.
Patient Education
Knowledge of the signs and symptoms of shunt malfunction or infection and the necessity for emergent medical evaluation in these instances is mandatory in patients, family members, and caregivers.
The patient, family, and caregivers should know that periodic re-evaluation is necessary.
Pumping the shunt is contraindicated in most cases.
Patients with vascular shunts, and some patients with other types of shunts, should receive prophylactic antibiotics before dental procedures or instrumentation of the bladder.
-
Noncommunicating obstructive hydrocephalus caused by obstruction of the foramina of Luschka and Magendie. This MRI sagittal image demonstrates dilatation of lateral ventricles with stretching of corpus callosum and dilatation of the fourth ventricle.
-
Noncommunicating obstructive hydrocephalus caused by obstruction of foramina of Luschka and Magendie. This MRI axial image demonstrates dilatation of the lateral ventricles.
-
Noncommunicating obstructive hydrocephalus caused by obstruction of foramina of Luschka and Magendie. This MRI axial image demonstrates fourth ventricle dilatation.
-
Communicating hydrocephalus with surrounding "atrophy" and increased periventricular and deep white matter signal on fluid-attenuated inversion recovery (FLAIR) sequences. Note that apical cuts (lower row) do not show enlargement of the sulci, as is expected in generalized atrophy. Pathological evaluation of this brain demonstrated hydrocephalus with no microvascular pathology corresponding with the signal abnormality (which likely reflects transependymal exudate) and normal brain weight (indicating that the sulci enlargement was due to increased subarachnoid cerebrospinal fluid [CSF] conveying a pseudoatrophic brain pattern).






