Practice Essentials
Subchorionic hemorrhage (subchorionic hematoma) is the most common sonographic abnormality in the presence of a live embryo. Subchorionic hemorrhage is bleeding beneath the chorion membranes that enclose the embryo in the uterus and appears to occur because of partial detachment of the chorion membranes from the wall of the uterus. [1] Vaginal bleeding affects 25% of all women during the first half of pregnancy and is a common reason for first-trimester ultrasonography. Subchorionic hematoma occurs in 18-22% of intrauterine pregnancies with vaginal bleeding. [2]
Sonographic visualization of a subchorionic hematoma is important in a symptomatic woman because pregnant women with a demonstrable hematoma have a prognosis worse than women without a hematoma (see images below). However, small, asymptomatic subchorionic hematomas do not worsen the patient's prognosis. [3, 4, 5, 6, 7, 8, 9]
In women whose sonogram shows a subchorionic hematoma, the outcome of the fetus depends on the size of the hematoma, the mother's age, and the fetus's gestational age. [10, 11] Rates of miscarriage increase with advancing maternal age and increasing size of hematoma. Late first- or second-trimester bleeding also worsens the prognosis. The presence of sonographically detected subchorionic hemorrhage (subchorionic hematoma) increases the risk of miscarriage, stillbirth, abruptio placentae, and preterm labor.
Heller et al noted that the earlier in pregnancy a subchorionic hemorrhage is detected, the higher the rate of pregnancy failure.
Computed Tomography
CT scanning is relatively contraindicated during pregnancy because of the risk of radiation to the fetus. Pregnant patients may undergo CT for reasons such as an evaluation of trauma or acute abdomen. Scans may show an incidental or injury-related hyperattenuating subchorionic hemorrhage (subchorionic hematoma).
The sensitivity of CT may be high compared to that of sonography. However, because of the risk of radiation with CT, no large comparisons of the 2 modalities have been reported.
Normal chorioamniotic separation should not be confused with placental abruption.
Magnetic Resonance Imaging
MRI is not routinely performed to detect subchorionic hemorrhage (subchorionic hematoma); a more common indication is the detection of fetal anomalies. [25, 26] MRI may incidentally show a subchorionic hematoma and help in characterizing and determining the acuity of the hematomas by showing changes in signal intensity produced by various blood products. T1-weighted spin-echo and gradient-echo images are particularly useful in evaluating the hemorrhage.
In one study, fetal MRI techniques were evaluated to determine whether they were sufficient for the assessment of placental pathologies, and based on the study findings, MRI was considered by the authors to be a promising tool for the assessment of placental insufficiency. Pathologically, 26 placentas showed infarctions (96.2% on MR scans); 2 retroplacental hematomas were detected by MRI and confirmed by pathology; 9 of 14 subchorionic hematomas were confirmed; 6 of 8 intervillous hemorrhages were seen on MRI; and 3 of 6 cases of severe chorioamnionitis were diagnosed prenatally. [27]
Fetal motion sometimes limits MRI. However, the observer can confidently determine the age of the blood products.
Ultrasonography
Acute subchorionic hemorrhages (subchorionic hematomas) vary in echogenicity and are seen between the chorion and the uterine wall on sonograms (see images below). Isoechoic hematomas may be missed on initial sonograms, or they may be recognized as heterogeneous and thickened placentas.
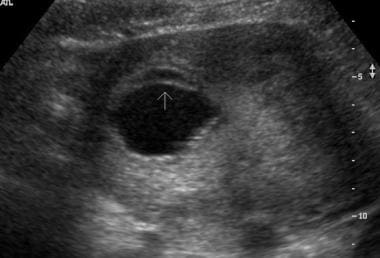 Transverse endovaginal scan of the uterus in a 45-year-old woman in 8th week of gestation. Small subchorionic hematoma is anterior to a gestational sac.
Transverse endovaginal scan of the uterus in a 45-year-old woman in 8th week of gestation. Small subchorionic hematoma is anterior to a gestational sac.
 Sagittal endovaginal scan of the uterus in a 19-year-old woman in 20th week of gestation demonstrates a small anterior subchorionic hematoma adjacent to the lower edge of the placenta.
Sagittal endovaginal scan of the uterus in a 19-year-old woman in 20th week of gestation demonstrates a small anterior subchorionic hematoma adjacent to the lower edge of the placenta.
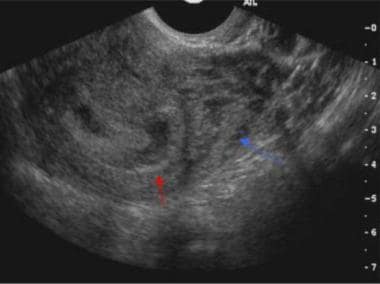 Sagittal endovaginal scan of the uterus demonstrates a small subchorionic hematoma (red arrow) in a 26-year-old woman in the 7th week of gestation. Also note the prominent retroplacental veins (blue arrow), which are normal in pregnancy.
Sagittal endovaginal scan of the uterus demonstrates a small subchorionic hematoma (red arrow) in a 26-year-old woman in the 7th week of gestation. Also note the prominent retroplacental veins (blue arrow), which are normal in pregnancy.
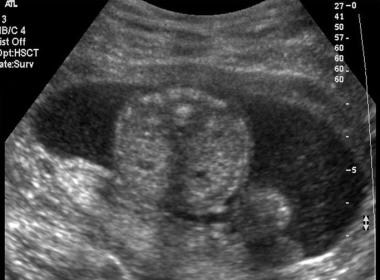
 Transverse endovaginal scan of the uterus in 45-year-old woman in the 13th week of a dichorionic-diamniotic twin pregnancy demonstrates an anterior subchorionic hematoma (cursors). Also note the normal chorioamniotic separation in the posterior sac.
Transverse endovaginal scan of the uterus in 45-year-old woman in the 13th week of a dichorionic-diamniotic twin pregnancy demonstrates an anterior subchorionic hematoma (cursors). Also note the normal chorioamniotic separation in the posterior sac.
 Sagittal endovaginal scan of the uterus in 37-year-old woman in the 13th week of a dichorionic-diamniotic twin pregnancy demonstrates an anterior subchorionic hematoma.
Sagittal endovaginal scan of the uterus in 37-year-old woman in the 13th week of a dichorionic-diamniotic twin pregnancy demonstrates an anterior subchorionic hematoma.
 Sagittal endovaginal scan in 37-year-old woman in the 13th week of a dichorionic-diamniotic twin pregnancy shows extension of the hematoma in the intertwin membrane cleft, where the 2 placentas fuse.
Sagittal endovaginal scan in 37-year-old woman in the 13th week of a dichorionic-diamniotic twin pregnancy shows extension of the hematoma in the intertwin membrane cleft, where the 2 placentas fuse.
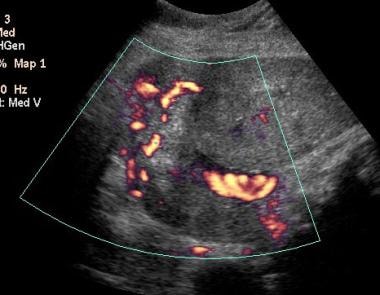
Color Doppler sonography may help in distinguishing the avascular hematoma from the highly vascular placenta. Follow-up sonography may also help in resolving hematomas.
A subchorionic hematoma can be considered large if it is greater than 50% of the size of the gestation sac, medium if it is 20-50%, and small if it is less than 20%. Large hematomas by size (>30-50%) and volume (>50 mL) worsen the patient's prognosis.
Hematomas may resolve over 1-2 weeks. During this time, they may be seen as complex fluid collections with mixed echogenicity. In addition, sonographic findings also confirm fetal viability [28] and can help in differentiating and diagnosing other conditions associated with miscarriage in the first trimester, such as ectopic pregnancy, blighted ovum, and twin gestation.
Follow-up ultrasonography should be performed as clinically indicated.
Degree of confidence
Ultrasonography lacks high sensitivity for small bleeds. However, it is the most useful modality in a pregnant patient with vaginal bleeding. The finding of a subchorionic or retroplacental hematoma as demonstrated on sonography performed immediately after an episode of vaginal bleeding indicates a prognosis worse than that expected if no hematoma were seen. [21, 22, 29, 30, 31]
Uterine fibroids or focal myometrial contractions (see image below) can cause the placenta to appear thickened, or they may look like subchorionic or retroplacental hematomas. Hematomas are avascular on color Doppler scanning. Fibroids have a characteristic hypoechoic appearance with or without calcifications and typical peripheral blood flow in color Doppler images. Color flow is seen in contracted myometrium, and transient myometrial contractions usually resolve within 30 minutes of scanning.
 Sagittal endovaginal scan of a dichorionic-diamniotic twin pregnancy in the 13th week of gestation in a 45-year-old woman. An empty gestation sac mimics a subchorionic collection (red arrow). Also note the transient uterine contraction (yellow arrow).
Sagittal endovaginal scan of a dichorionic-diamniotic twin pregnancy in the 13th week of gestation in a 45-year-old woman. An empty gestation sac mimics a subchorionic collection (red arrow). Also note the transient uterine contraction (yellow arrow).
Chorioamniotic separation has an anechoic appearance and usually resolves by 16 weeks. It can be distinguished from an anechoic hematoma by finding elevation of the membrane in chorioamniotic separation that extends over the fetal surface of the placenta and that terminates at the origin of the umbilical cord. The amniotic membrane is also thinner than the chorionic membrane (see image below).
 Transverse endovaginal scan of the uterus in 45-year-old woman in the 13th week of a dichorionic-diamniotic twin pregnancy demonstrates an anterior subchorionic hematoma (cursors). Also note the normal chorioamniotic separation in the posterior sac.
Transverse endovaginal scan of the uterus in 45-year-old woman in the 13th week of a dichorionic-diamniotic twin pregnancy demonstrates an anterior subchorionic hematoma (cursors). Also note the normal chorioamniotic separation in the posterior sac.
Primary intra-amniotic hemorrhage can occur with a large subchorionic hematoma, with trauma, or with an invasive procedure such as chorionic villous sampling [32] or amniocentesis. Floating echoes (see Image below) or echogenic clots may be seen in the amniotic cavity.
 Transverse endovaginal scan in a 29-year-old woman in 21st week of gestation demonstrates intra-amniotic hemorrhage as fine echoes dispersed in the amniotic fluid.
Transverse endovaginal scan in a 29-year-old woman in 21st week of gestation demonstrates intra-amniotic hemorrhage as fine echoes dispersed in the amniotic fluid.
Hematomas of the umbilical cord are rare and may result from amniocentesis and sampling of blood from the umbilical cord. These hematomas are seen as echogenic masses limited to the cord itself.
Prominent retroplacental and myometrial vessels should be distinguished from heterogeneous bleeding. The vessels appear as serpentine, anechoic structures and demonstrate flow on color Doppler sonography (see images below); these features differentiate them from avascular hematomas.
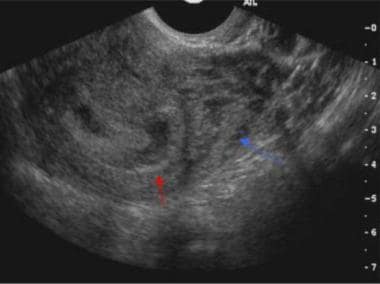 Sagittal endovaginal scan of the uterus demonstrates a small subchorionic hematoma (red arrow) in a 26-year-old woman in the 7th week of gestation. Also note the prominent retroplacental veins (blue arrow), which are normal in pregnancy.
Sagittal endovaginal scan of the uterus demonstrates a small subchorionic hematoma (red arrow) in a 26-year-old woman in the 7th week of gestation. Also note the prominent retroplacental veins (blue arrow), which are normal in pregnancy.
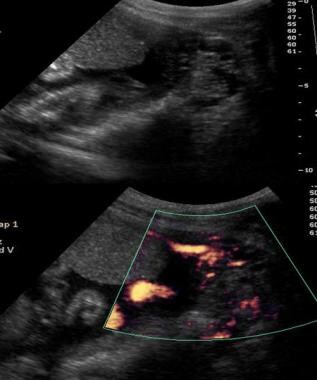 Sagittal gray-scale endovaginal scan (top) of the uterus in a 16-year-old mother in 25th week of gestation demonstrates a hypoechoic area adjacent to the lower edge of the placenta; this finding suggests a small subchorionic hematoma. However, color Doppler scan (bottom) at the same level confirms that this finding represents prominent vessels mimicking a subchorionic hematoma.
Sagittal gray-scale endovaginal scan (top) of the uterus in a 16-year-old mother in 25th week of gestation demonstrates a hypoechoic area adjacent to the lower edge of the placenta; this finding suggests a small subchorionic hematoma. However, color Doppler scan (bottom) at the same level confirms that this finding represents prominent vessels mimicking a subchorionic hematoma.
 Sagittal endovaginal gray-scale scan in a 21-year-old woman in 33rd week of pregnancy demonstrates prominent retroplacental vessels mimicking a retroplacental hematoma.
Sagittal endovaginal gray-scale scan in a 21-year-old woman in 33rd week of pregnancy demonstrates prominent retroplacental vessels mimicking a retroplacental hematoma.
-
Transverse endovaginal scan of the uterus in a 45-year-old woman in 8th week of gestation. Small subchorionic hematoma is anterior to a gestational sac.
-
Sagittal endovaginal scan of the uterus in a 19-year-old woman in 20th week of gestation demonstrates a small anterior subchorionic hematoma adjacent to the lower edge of the placenta.
-
Transverse scan demonstrates a hematoma in a 19-year-old woman in 20th week of gestation.
-
Sagittal endovaginal scan of the uterus demonstrates a small subchorionic hematoma (red arrow) in a 26-year-old woman in the 7th week of gestation. Also note the prominent retroplacental veins (blue arrow), which are normal in pregnancy.
-
Transverse endovaginal scan of the uterus in 45-year-old woman in the 13th week of a dichorionic-diamniotic twin pregnancy demonstrates an anterior subchorionic hematoma (cursors). Also note the normal chorioamniotic separation in the posterior sac.
-
Sagittal endovaginal scan of the uterus in 37-year-old woman in the 13th week of a dichorionic-diamniotic twin pregnancy demonstrates an anterior subchorionic hematoma.
-
Sagittal endovaginal scan in 37-year-old woman in the 13th week of a dichorionic-diamniotic twin pregnancy shows extension of the hematoma in the intertwin membrane cleft, where the 2 placentas fuse.
-
Sagittal endovaginal scan of a dichorionic-diamniotic twin pregnancy in the 13th week of gestation in a 45-year-old woman. An empty gestation sac mimics a subchorionic collection (red arrow). Also note the transient uterine contraction (yellow arrow).
-
Sagittal endovaginal scan of the uterus in a 29-year-old woman in 9th week of gestation demonstrates nonfusion and separation of chorion and amnion.
-
Transverse endovaginal scan in a 29-year-old woman in 21st week of gestation demonstrates intra-amniotic hemorrhage as fine echoes dispersed in the amniotic fluid.
-
Sagittal gray-scale endovaginal scan (top) of the uterus in a 16-year-old mother in 25th week of gestation demonstrates a hypoechoic area adjacent to the lower edge of the placenta; this finding suggests a small subchorionic hematoma. However, color Doppler scan (bottom) at the same level confirms that this finding represents prominent vessels mimicking a subchorionic hematoma.
-
Sagittal endovaginal gray-scale scan in a 21-year-old woman in 33rd week of pregnancy demonstrates prominent retroplacental vessels mimicking a retroplacental hematoma.
-
Color Doppler scan in a 21-year-old woman in 33rd week of pregnancy demonstrates prominent retroplacental vessels mimicking a retroplacental hematoma.