Practice Essentials
Bronchiectasis is irreversible, abnormal dilatation of the bronchi. [1] Common etiologies for bronchiectasis are congenital abnormalities, recurrent infection, and airway obstruction. The tethering effect of pulmonary fibrosis can also dilate the airways, causing traction bronchiectasis. [2, 3] Involved bronchi are dilated, inflamed, and easily collapsible, resulting in airflow obstruction and impaired clearance of secretions. Bronchiectasis typically presents with cough, sputum production, and airway obstruction, [4] and in severe cases, massive hemoptysis can lead to death. [1]
In bronchiectasis, damaged epithelium impairs removal of mucus and increases the risk of infection by pathogens such as Pseudomonas aeruginosa, Haemophilus, Aspergillus fumigatus, and nontuberculous mycobacteria. [5]
Bronchiectasis is a final common pathway for many diseases with diverse fundamental causes. Knowledge of the root cause of bronchiectasis in a particular patient is more helpful for treatment than an understanding of the generic subject of bronchiectasis. Bronchiectasis is associated with a wide range of disorders, but it usually results from necrotizing bacterial infections, such as infections caused by the Staphylococcus or Klebsiella species or Bordetella pertussis. Unfortunately, in about half the cases, the specific cause of bronchiectasis remains undetermined. [6]
Hemoptysis is common and may occur in as many as 50% of patients. Episodic hemoptysis with little to no sputum production (dry bronchiectasis) is usually a sequela of tuberculosis.
Radiography
Chest radiography helps to identify serious disease, and it was once the standard imaging modality. [2] However, the radiographs may depict no abnormalities, or the findings may be nonspecific in patients with less-severe disease. [3]
Various abnormal radiographic findings have been described as follows (see the images below) [93, 94, 95] :
-
Parallel line opacities (tram tracks) caused by dilated, thickened bronchi are seen along their length
-
Ring opacities or cystic spaces as large as 2 cm in diameter resulting from cystic bronchiectasis, sometimes with fluid levels
-
The signet ring sign corresponds to a dilated bronchus immediately adjacent to a smaller companion pulmonary artery
-
Cysts related to cystic bronchiectasis, sometimes with fluid levels (demilunes)
-
Tubular opacities caused by dilated, fluid-filled bronchi - These may occur as Y- or V-shapes or as "finger-in-glove" opacities, which radiate from the pulmonary hilum
-
Increased size and loss of definition of the pulmonary vessels in the affected areas as a result of peribronchial fibrosis
-
Crowding of pulmonary vessels from the associated loss of volume, usually caused by mucous obstruction of the peripheral bronchi
-
Oligemia as a result of reduction in pulmonary artery perfusion (severe disease)
-
Signs of compensatory hyperinflation of the unaffected lung
(See the images below)
 A close-up radiograph of the left upper lung in a 31-year-old woman with chronic cough since childhood shows nodules in the left upper lung; the right upper lung was similarly involved.
A close-up radiograph of the left upper lung in a 31-year-old woman with chronic cough since childhood shows nodules in the left upper lung; the right upper lung was similarly involved.
 A 65-year-old woman was examined for chronic cough. The lateral chest radiograph shows hyperinflation and accentuation of the central bronchial interstitium.
A 65-year-old woman was examined for chronic cough. The lateral chest radiograph shows hyperinflation and accentuation of the central bronchial interstitium.
Additional nonspecific radiographic findings in bronchiectasis include the following:
-
Volume loss related to mucous plugging and associated crowding of the pulmonary vasculature: Actual destruction of lung parenchyma and/or pulmonary fibrosis can be present
-
Abnormal lung opacities related to inflammation, scars, and/or mucous plugging
-
Signs of compensatory hyperinflation of the unaffected lung
-
Loss of definition of the central bronchi and vessels, related to central interstitial lung disease and retained secretions
Traction bronchiectasis occurs with pulmonary fibrosis. In pulmonary fibrosis, honeycombing and distortion can be visible radiographically. However, the radiographic diagnosis of traction bronchiectasis can be difficult, unless the surrounding lung is opacified. [94] Patients with bronchiectasis are at increased risk for pneumonia. Chest radiography can be used for detection and follow-up of pneumonia associated with bronchiectasis.
Bronchography
Bronchography was the investigation of choice for bronchiectasis from its introduction in 1922 until the advent of HRCT scanning in the mid-1980s. Bronchography is now rarely used. Bronchography is performed by instilling contrast material via a catheter or bronchoscope under fluoroscopic control and conventional radiographic imaging. The procedure is unpleasant for the patient and is also associated with temporary impairment of ventilation, as well as allergic and foreign body reactions to the contrast medium. In addition, interpretation of bronchographic images is difficult because of underfilling and retained secretions.
Degree of confidence
The accuracy of conventional radiographic findings in the diagnosis of bronchiectasis is unknown, because the findings are variable and nonspecific and depend on the severity and extent of the bronchiectasis. However, the severity of disease as seen on conventional radiography and HRCT scans shows good correlation. Chest radiographic findings may be normal or nonspecific in patients with less severe disease. The prevalence of signs of bronchiectasis at radiography correlates with the severity of bronchiectasis at HRCT, although radiography is less sensitive and less specific. [96]
Many conventional radiographic findings are nonspecific and can be seen in patients with idiopathic pulmonary fibrosis, sarcoidosis, histiocytosis X, rheumatoid lung, and other chronic interstitial lung disorders.
If bronchiectasis is detected radiographically, chest CT is appropriate for categorization of extent and morphologic severity.
Computed Tomography
CT is the primary imaging modality for bronchiectasis. [1, 4, 13, 14, 16, 17, 63, 92, 97, 98, 99, 100]
CT indications of bronchiectasis include the following [10, 90, 101, 102, 103] :
-
An increased bronchoarterial ratio, manifested by the signet ring sign, corresponding to a dilated bronchus immediately adjacent to a smaller companion pulmonary artery
-
Lack of bronchial tapering
-
Distortions of normal bronchial shape, such as varicoid (string of pearls) or cystic (cluster of grapes sign) morphology [104]
-
Bronchi identifiable within 1 cm of the costal surface
The following are commonly associated with bronchiectasis:
-
Bronchial thickening
-
Centrilobular nodularity related to bronchiolitis
-
Mucous plugging
-
Bronchial arterial dilatation
-
Air trapping
-
Volume loss or hyperinflation
(See the image below.)
On axial images, in cylindrical bronchiectasis, bronchi coursing horizontally are seen as parallel lines, and vertically oriented bronchi are seen as circular lucencies that are larger than the adjacent pulmonary artery (signet-ring appearance).
(See the image below.)
 This HRCT scan in a 13-year-old female shows left lower lobe bronchiectasis, secondary to tuberculosis.
This HRCT scan in a 13-year-old female shows left lower lobe bronchiectasis, secondary to tuberculosis.
Varicose bronchiectasis may be seen as nonuniform bronchial dilatation. Other findings include the following:
-
Areas of increased and decreased perfusion and attenuation
-
Tracheomegaly
-
Enlarged mediastinal nodes
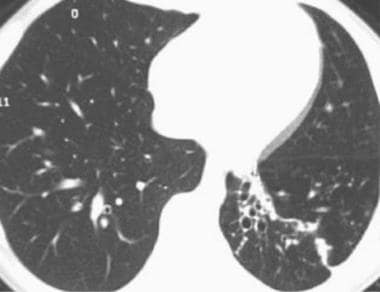
Fluid-filled bronchi present as tubular or branching structures when they course horizontally or as nodules when they are perpendicular to the plane of the CT scan section (see the image below).
 This HRCT scan demonstrates findings of fluid-filled dilated bronchi in the left lower lobe of a 65-year-old man.
This HRCT scan demonstrates findings of fluid-filled dilated bronchi in the left lower lobe of a 65-year-old man.
Degree of confidence
Except for extremely obese patients and examinations compromised by motion, volumetric imaging of the chest provides a very high degree of confidence to confirm or deny the diagnosis of bronchiectasis. HRCT scanning has a sensitivity of 96% and a specificity of 93%. [12]
Some patients without bronchiectasis have a 1.49:1 bronchus-to-artery ratio; therefore, the ratio is reliable only if it is greater than 1.5. If the ratio is less than 1.5, other signs, such as bronchial wall thickening and lack of tapering, should be present for the diagnosis of bronchiectasis, according to the European Respiratory Society. The CT criterion for abnormal bronchoarterial dilatation in children and adolescents is more than 0.8. [20]
Bronchial measurements may vary with the use of different window levels and window widths. [50] Bronchial wall thickening is optimally seen with wide window width, such as 1000, and a low window level, such as -700 HU. Aritfactual wall thickening can be produced by changing window width. [51] Accuracy is improved when images are reconstructed with a slice thickness of 1 mm or less and assessed at a window level of −450 HU. [105]
A bronchial wall thickening finding is not specific and is also seen in patients with asthma and smokers. Bronchiectasis occurs frequently in smokers with chronic obstructive pulmonary disease (COPD). In a quantitative CT study of patients with bronchiectasis who smoked, the BA ratio (bronchial lumen and adjacent artery), wall thickness, and wall area percent were significantly greater for whole lung and 4th-6th airway generations. [100]
False positives/negatives
The variability of the bronchus-to-artery ratio at high altitudes and in patients with pulmonary hypertension may result in an overdiagnosis because of vasoconstriction in these conditions. The bronchial diameter relative to the adjacent pulmonary artery also increases with increasing altitude. [106]
In patients with consolidation, dilated bronchi may not be seen. Cardiac and respiratory artifacts may obscure the results or mimic subtle bronchiectasis in the left lower lobe. Rarely, histiocytosis X and cavitating pulmonary masses mimic cystic bronchiectasis. Traction bronchiectasis occurs in patients with interstitial fibrosis and results from fibrous tethering of the bronchial wall. Rather than a primary bronchial abnormality, the bronchiectasis is caused by tethering and traction.
The patient’s age should be considered, since the bronchoarterial ratio increases with age. [97] In rare instances in adults, but more frequently in pediatric patients, bronchiectasis can be reversible.
A dilated, cystic bronchus should be distinguished from a bulla, since a bronchial cyst has a perceptible wall, while a bulla does not.
At times, severely dilated bronchi with associated volume loss can simulate honeycombing. [101]
Magnetic Resonance Imaging
MRI can be used to find bronchial wall thickening and dilatation of central bronchi, but spatial resolution limits assessment of smaller airways, such as third to fourth generation. [107] Different sequences, including fast breath–hold acquisition techniques and very short echo-time, are increasingly used for better pulmonary detail. [108, 109]
While volumetric CT remains the primary mode of assessment for bronchiectasis in adults, for cystic fibrosis patients and for young patients who may need repeated follow-up examinations, MRI yields useful information.
Teufel et al compared HRCT and 1.5-Tesla MRI using a very short echo time in 51 patients with cystic fibrosis. For these patients, both CT and MRI were able to detect bronchiectasis, mucous plugging, and peribronchial thickening, with MRI strongly correlating with the CT findings. [98] Montella et al compared chest MRI with HRCT in 50 non–cystic fibrosis pediatric patients, and both modalities demonstrated bronchiectasis in approximately 72% of those subjects. Other findings in chronic pediatric lung disease were also assessed, with results supporting the use of chest MRI as a reasonable alternative to CT. [110]
Although CT has better spatial resolution and shows morphology in more detail than MRI, MRI is superior for assessment of functional changes of altered hemodynamics and perfusion. [107] ] [12] Helium-3 (3He) MRI may be used for evaluation of pulmonary ventilation and function. [111]
Nuclear Imaging
Patients with bronchiectasis can suffer from chronic productive cough, recurrent infections, and hemoptysis. V/Q scanning can be useful in determining whether surgical resection is appropriate therapy, especially for hemoptysis. In one series, 23 of 66 patients treated surgically had hemoptysis as a symptom. V/Q scanning demonstrated undiminished perfusion in cylindrical bronchiectasis, but areas of cystic or mixed cystic and cylindrical bronchiectasis showed perfusion defects. If a patient has a scan showing less than 10% perfusion of a bronchiectatic region, that patient can benefit from surgical resection of that nonfunctional region. [112]
The purpose of a V/Q scan is to determine perfused versus nonperfused areas of lung rather than to make a diagnosis of bronchiectasis. Different diseases can cause nonperfused areas of lung, so V/Q is used in conjunction with CT or MRI.
Angiography
Hemoptysis is symptomatic of a potentially life-threatening condition and warrants urgent and comprehensive evaluation of the lung parenchyma, airways, and thoracic vasculature.
Multidetector-row CT angiography permits noninvasive, rapid, and accurate assessment of the cause and consequences of hemorrhage into the airways and helps guide subsequent management. [25, 113] The combined use of thin-section axial scans and more complex reformatted images allows clear depiction of the origins and trajectories of abnormally dilated systemic arteries that may be the source of hemorrhage and that may require embolization.
The vasculature, pulmonary parenchyma, and airways can be assessed with MDCT angiography. In disorders with chronic lung inflammation, including bronchiectasis, abnormal collateral systemic vessels form in the affected parts of the lung. These collateral bronchial arteries appear as tortuous vessels and can bleed. Occasionally, nonbronchial systemic arteries or pulmonary arteries bleed. Multiplanar reformatted images are used for identifying the origins and courses of these vessels.
Bronchiectasis, chronic bronchitis, lung malignancy, tuberculosis, and chronic fungal infection are some of the most common underlying causes of hemoptysis and are easily detected with CT angiography.
Results from multidetector CT angiography can be used to direct therapeutic angiography for bronchial or pulmonary arterial embolization or surgical resection.
Occasionally, an examination is limited by artifact from patient motion, data depletion from a very large patient, or timing of contrast bolus. Otherwise, MDCT usually demonstrates the vasculature and the pulmonary parenchyma well.
In a series of 22 patients in whom 16-detector row CT was used, bronchial (100%) and nonbronchial (62%) arteries causing hemoptysis were visible, with most being traceable throughout their length. [114] Substantial technological advances in CT since allow detailed visualization.
-
A 27-year-old man diagnosed with reactive airway disease as a child was examined because of frequent respiratory infections. The posteroanterior chest radiograph shows ill-defined pulmonary nodular opacities, mild scoliosis, and moderate overaeration.
-
A 27-year-old man diagnosed with reactive airway disease as a child was examined because of frequent respiratory infections. This high-resolution computed tomography (HRCT) scan through the upper lungs shows extensive bronchiectasis. The sweat test was positive, and cystic fibrosis was diagnosed.
-
A close-up radiograph of the left upper lung in a 31-year-old woman with chronic cough since childhood shows nodules in the left upper lung; the right upper lung was similarly involved.
-
The HRCT scan shows thick-walled, slightly ectatic bronchi. The patient has cystic fibrosis, which was diagnosed and treated since childhood.
-
A 65-year-old woman was examined for chronic cough. The lateral chest radiograph shows hyperinflation and accentuation of the central bronchial interstitium.
-
This posteroanterior chest radiograph shows hyperinflation and partially obscured heart borders.
-
This HRCT scan through the right upper lobe demonstrates bronchiectasis. Despite conventional antibiotic treatment, the patient continued to be symptomatic. Eventually, she underwent bronchoscopy, and sampled cultures grew Mycobacterium avium-intracellulare complex.
-
A 54-year-old asymptomatic woman with a history of tuberculosis was referred for preoperative chest radiography. The radiograph shows tracheal deviation to the right, an elevated minor fissure, and linear lucencies in the partially atelectatic right upper lung; these findings indicate bronchiectasis.
-
This lateral chest radiograph shows a partially atelectatic right upper lobe (same patient as in the previous image). The patient has cicatricial tuberculous bronchiectasis.
-
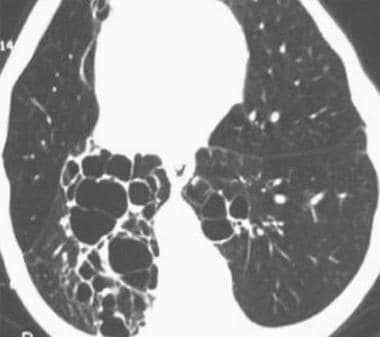
HRCT scan in a 75-year-old man with cystic bronchiectasis, right worse than left lower lobes.
-
This HRCT scan in a 13-year-old female shows left lower lobe bronchiectasis, secondary to tuberculosis.
-
This HRCT scan demonstrates findings of fluid-filled dilated bronchi in the left lower lobe of a 65-year-old man.
-
Posteroanterior chest radiograph demonstrates central bronchial thickening and widespread bilateral bronchiectasis, worst in the right upper lobe, in this 25-year-old male with cystic fibrosis.
-
This magnified view of the right upper lobe in a 25-year-old male with cystic fibrosis shows tram tracks and rings, reflecting bronchial thickening. Dilated bronchi filled with mucus are seen as branching tubular opacities.
-
Axial image from volumetric CT of a 25-year-old male with cystic fibrosis shows thick, dilated bronchi, some with mucus plugging.
-
Coronal reconstruction from volumetric CT of a 25-year-old male with cystic fibrosis shows thick bronchial walls and dilatation as well as areas of mucous plugging, worst in the right upper lobe.
-
Coronal reformat from volumetric CT shows tracheomegaly and cystic bronchiectasis of Mounier-Kuhn disease.
-
Coronal reconstruction image from volumetric CT in patient with rheumatoid arthritis shows upper lobe predominant cylindrical bronchiectasis.