Practice Essentials
Coronary artery disease (CAD) is a complex disease that causes reduced or absent blood flow in 1 or more of the arteries that encircle and supply the heart. The disease may be focal or diffuse. Apart from rare congenital anomalies (birth defects), coronary artery disease is usually a degenerative disease, uncommon as a clinical problem before the age of 30 years and common by the age of 60 years. One in four people will have a heart attack. The first recognized symptom may be death. The term coronary is derived from crown, referring to the way these arteries sit on the heart.
CAD is one of the major cardiovascular diseases affecting the global human population. This disease has proved to be the major cause of death in both developed and developing countries. Lifestyle, environmental factors, and genetic factors pose as risk factors for the development of cardiovascular disease. The prevalence of risk factors among healthy individuals elucidates the probable occurrence of CAD in the near future. Risk factors for CAD include diabetes mellitus, hypertension, smoking, hyperlipidemia, obesity, chronic kidney disease, cigarette smoking, diet, family history, homocystinuria, and psychosocial stress. [1, 2]
The American College of Radiology notes that CAD has a long asymptomatic latent period and that early targeted preventive measures can reduce mortality and morbidity.
Radiography
Coronary angiography shows where vessels originate, how they branch, whether they have obstructions or dissections or thrombi, the degree of any obstructions, and which territories they supply. (See the x-ray angiograph below.)
 X-ray angiography is the criterion standard for delineating the coronary anatomy, but it is inferior to MRI and CT in identifying myocardium with impaired blood delivery, in assessing the functional consequences, and in identifying the development of microvascular collaterals.
X-ray angiography is the criterion standard for delineating the coronary anatomy, but it is inferior to MRI and CT in identifying myocardium with impaired blood delivery, in assessing the functional consequences, and in identifying the development of microvascular collaterals.
Key questions answered during an examination of the anatomy include the following:
-
Does a coronary artery pass between the aorta and the pulmonary artery, where it may get pinched?
-
Does a segment tunnel under a myocardial bridge?
-
Which pathway supplies the posterior surface? Is it the right, the left circumflex, or both? That is, is it right dominant, left dominant, or circumflex dominant?
-
Does the left anterior descending artery (LAD) wrap around the apex to supply the distal diaphragmatic surface?
-
What vessel supplies the atrioventricular (AV) node? Is its blood supply impaired?
-
If an infarct is present, which is the infarct-related artery?
-
If abnormal wall motion is seen, which branch obstruction accounts for it?
-
Are any bypass graft vessels present? If so, where do they originate (left internal mammary, saphenous vein graft from anterior aortic root)? Are they long or short, where do they connect, and how do they connect (end to side, side to side)?
The caliber of vessels may be estimated by comparing them with the known diameter of the catheter if it appears on the image. The reviewer should take into account the fact that magnifications differ at different distances from the source to the intensifier with x-ray projection angiography.
After the anatomy is described, location, percentage of narrowing, and character of all focal obstructions (stenoses) are discussed.
For each lesion:
-
Is it concentric (symmetric) or eccentric (1-sided)?
-
Is it long or short?
-
Does it abut a branch vessel (which may be lost after intervention)?
-
Is it calcified?
-
Is any thrombus visible?
-
Is evidence of intimal tear shown?
-
Is evidence of vessel spasm apparent?
-
Is diffuse narrowing revealed?
The flow of contrast agent–labeled blood offers useful information. TIMI criteria may be applied to determine whether the distribution of contrast material is TIMI 0 (incomplete—fails to fill branches and the distal portion of the vessel), TIMI 1 (slow but complete), or TIMI 2 (brisk and complete). When imaging is performed at a rate of 30 frames per second, the number of frames it takes for a vessel to completely fill may be assessed. The normal number is approximately 21 frames. Filling takes longer in patients with disease than in healthy people—not only in the diseased vessel but also in normal vessels.
Consider how findings may affect possible interventions, and report them accordingly. Clinically significant narrowing in the left main coronary artery is a medical emergency because of the amount of myocardium at risk. Other patterns of disease can pose similar risk—for example, proximal disease in both the LAD and a dominant right or left circumflex vessel.
-
What is the caliber of distal vessels that may support a bypass graft?
-
Are the distal vessels calcified?
-
Is any stenosis near a branch point (such that balloon angioplasty of the lesion may obstruct a branch artery)?
-
How long is the left main coronary artery?
-
How much myocardium is at risk?
Examine images for ancillary findings.
-
Which calcifications move with the heart?
-
Is the mitral valve annulus calcified?
-
Is the aortic root or the aortic valve calcified?
-
Are valve rings, bypass vessel rings or clips, stents, sternal wires, or other evidence of prior surgeries apparent?
-
If pacer wires are noted, where do they end?
-
Does evidence suggest chamber enlargement, aneurysm, cardiac displacement, abnormal pulmonary venous return, unusual persistence of fetal structures, or other variants?
If left ventriculography is performed, examine left ventricle (LV) function for ejection fraction (EF), for regional wall motion abnormalities, and for valve integrity. Hypokinesis indicates reduced motion, akinesis indicates no motion, and dyskinesis indicates reversed motion, such as ballooning outward during systole. Note any leakage of contrast material back into the left atrium and any restriction of the valve leaflets.
At the time of coronary angiography, the same set of tools can be used to examine other vessels (eg, renal and carotid arteries). [24]
Although it is the method used by most interventional cardiologists to assess the severity of CAD and to guide treatment, coronary angiography has many known limitations, particularly the fact that it is a lumenogram depicting foreshortened, shadowgraph, planar projections of the contrast-filled lumen rather than imaging the diseased vessel itself. Intravascular imaging—intravascular ultrasound and optical coherence tomography—is clinically useful for answering questions such as whether stenosis is clinically relevant, for identifying the culprit lesion, and for indicating whether the patient is at high risk of future adverse events. [25]
Degree of confidence
Coronary angiography is the standard for identifying coronary anatomy and stenoses. In select cases, alternative imaging may appear superior, but one must be careful to distinguish between high-quality or good-looking pictures and reliable results. Coronary angiography may provide a false-negative result if a branch vessel is occluded at its origin, if the disease is asymmetrical, or if the lesion is cracked, such that the contrast agent can extend close to the full diameter of the vessel even though the vessel cross-sectional area is severely reduced (eg, a star-shaped lesion).
It is possible to miss a lesion that is hidden behind another vessel, but this problem is generally resolved by using angled views and by moving the camera (panning) during image collection. If the significance of an obstruction is unclear on coronary angiography, intravascular ultrasound (IVUS) or a flow wire may be used to clarify its spatial extent in relation to the vessel lumen or its impact on flow down a particular branch vessel. A vasodilator may be delivered to assess flow reserve. X-ray angiography is not a good detector of small-vessel disease, epitomized by cardiac syndrome X.
The predictive accuracy of stress ECG can be as low as 50% but rises above 75% if it is combined with proBNP blood testing. [15] Accuracy of stress imaging for detection of CAD ranges from 70 to 90% if the target stress level is achieved while off antianginal medications.
Treadmill or bicycle stress testing is generally preferred, followed by dobutamine stress testing, then adenosine combined with low-level exercise. Adenosine or dipyridamole alone is less reliable. Chest pain during a dipyridamole stress test in the absence of CAD is not uncommon. [26] Target heart rate (peak HR) for exercise or dobutamine stress testing is 85% of age-predicted maximum (85% of peak systolic BP × peak HR). Animal studies have shown that the rate-pressure product is a better predictor of the stress levels that should induce detectible ischemia. A 50% blockage should be detected with more than 50% confidence above a rate-pressure product of 20 kilotorr/min, and with more than 85% confidence above 25 kilotorr/min.
Limitations
Balloon angioplasty can disrupt an obstruction so that the vessel appears to recover its full diameter, when, in fact, the cross-sectional area is improved only minimally and insufficiently. 3-D imaging can be used to examine contrast agent attenuation and percentage of narrowing. On occasion, this condition may be identified by looking at the lesion on different views or by performing IVUS or optical CT.
The introduction of a catheter or a wire can cause intimal dissection (a tear in the lining of a vessel), which may be mistaken for vascular spasm, thrombosis, or a long stenosis on cursory examination. A tissue flap in the endothelial lining may alternate between an open position and an obstructive one, mimicking a spasm; however, it is not responsive to nitrates. The distinction may be a matter of life or death. If clinically significant, stent placement, bypass, placement of a perfusion catheter, or other emergency treatment is typically required to treat a dissection. Sudden obstruction due to dissection can be deadly and does not respond to medication.
Myocardial bridges, or small bands of muscle overlying a vessel, may be mistaken for stenoses; however, these are not amenable to angioplasty. Obstruction from a myocardial bridge is smooth and eccentric. Observation throughout the cardiac cycle shows that the obstruction occurs during systole.
Computed Tomography
Computed tomography (CT) imaging of the coronary arteries can be achieved with fast CT and with electron beam CT (EBCT) systems triggered or gated by electrocardiography (ECG) to accumulate data when the heart is in diastole. The newest technology uses 64-section multidetector-row CT. [23, 27, 28, 29, 30]
With section thickness of 1 or 0.5 mm or less, the coronary anatomy is laid out in a 3-D volume. Image processing can greatly facilitate visualization of the course of vessels and branches and the presence and degree of stenoses. The coronary artery tree may be viewed as a solid rendering of the surface of the heart, but portions may be obstructed from view.
Proper viewing of each coronary artery branch should include clean views in which the LV blood pool, the aortic root, and all extracardiac structures are removed; vascular projections are limited to zones that include the vessel of interest and a margin for partial-volume effects.
One should not rely on threshold-based renderings, which can cause false stenosis and false obstruction, causing an intravascular thrombus to be missed. Use of a pair of volumes before and after administration of contrast material for elastic matching [31] greatly facilitates evaluation by automatically isolating the coronary tree without thresholding. [16]
CT also enables superb evaluation of blood delivery. In principle, CT combined with catheterization permits accurate definition of the extent of collateral-dependent myocardium. [16] (See the CT image below.)
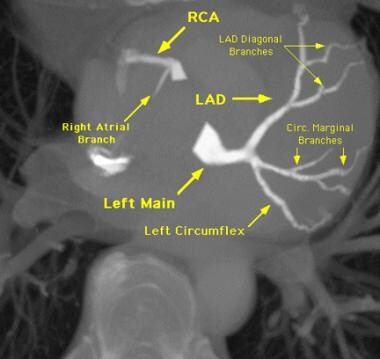 Elastic-match imaging automatically identifies differences between image volumes. The acquisition of 1 set of contrast-enhanced chest CT images via the coronaries and a nonenhanced set provides a 3-dimensional view of the coronary-artery tree. The nonenhanced volume data were rendered as holographic projections to provide the anatomic context, and the elastic-match coronary tree was overlaid. In addition to automation, this method avoids thresholding so that small branches and filling defects, if present, are represented properly.
Elastic-match imaging automatically identifies differences between image volumes. The acquisition of 1 set of contrast-enhanced chest CT images via the coronaries and a nonenhanced set provides a 3-dimensional view of the coronary-artery tree. The nonenhanced volume data were rendered as holographic projections to provide the anatomic context, and the elastic-match coronary tree was overlaid. In addition to automation, this method avoids thresholding so that small branches and filling defects, if present, are represented properly.
Pizzuto et al found that transthoracic Doppler echocardiography can improve the diagnostic accuracy of multidetector computed tomography (MDCT) for detecting left anterior descending coronary artery (LAD) stenosis. In 144 consecutive patients, coronary anatomy was assessed with MDCT, and echocardiography was used to calculate coronary flow reserve (CFR) by measuring the ratio of hyperemic to baseline peak flow velocity; results of both methods were verified by invasive coronary angiography. [32]
In a univariate model, prediction of significant LAD stenosis was slightly, but significantly, better with CFR (sensitivity 90%, specificity 96%, positive predictive value 84%, negative predictive value 97%, diagnostic accuracy 94%) than with MDCT (sensitivity 80%, specificity 93%, positive predictive value 71%, negative predictive value 95%, diagnostic accuracy 90%). [32]
When findings from transthoracic Doppler echocardiography and MDCT were consistent, diagnostic accuracy was increased (96%). Among 13 patients whose condition was missed by MDCT, transthoracic Doppler echocardiography proved 100% accurate for predicting significant LAD stenosis. [32]
In a study of myocardial CT perfusion imaging versus single-photon emission CT (SPECT) perfusion imaging for diagnosis of CAD, overall performance was better for myocardial CT perfusion imaging. Sensitivity and specificity of CT perfusion imaging for diagnosis of CAD were 88% and 55%, respectively, versus 62% and 67% for SPECT. Sensitivities for left main, 3-vessel, 2-vessel, and 1-vessel disease were 92%, 92%, 89%, and 83%, respectively, for CT perfusion imaging, and 75%, 79%, 68%, and 41%, respectively, for SPECT. [33]
Degree of confidence
The ability of MRI and CT to depict anatomy and the absence of notable obstructions is improving rapidly, but performance is not uniform. The value of MRI and CT must be assessed in a truly double-blind fashion until standardized, reliable methods are widely established.
Whether MRI and CT results match in terms of the percentage of stenosis is relatively unimportant. Most important is whether MRI and CT reliably depict normal tissue and culprit lesions, and whether they establish severity and territories supplied by the culprit vessel. Both MRI and CT offer the significant advantage of direct assessment of zones of impaired blood delivery.
Limitations
MRI shows calcifications as black or signal voids, whereas CT shows calcifications as white and similar to contrast-filled blood. These appearances can influence the estimation of stenoses.
Heavy calcification causes a beam-hardening artifact on CT that can interfere with visualization. Stents cause a local disturbance stronger on MRI than on CT. Also, with 3-D MRI or CT, one must be certain to understand how images account for local curvature in and out of the imaging planes. In finding the best plane to show a vessel, radiologists can mistake a local curve that is out of plane for an apparent stenosis. Proper image processing helps to resolve this problem.
Magnetic Resonance Imaging
Coronary magnetic resonance imaging (MRI) has improved from early methods [8] and equipment sufficient to identify normal proximal coronary arteries and courses, but it is not a clinical replacement for coronary angiography, apart from ruling out aberrant coronary origins, demonstrating graft or native vessel patency, or following up on specific lesions.
Coronary MRI may be performed by using 3-D volume, but the trade-off in time and resolution favors imaging in selective planes that address each branch of interest. At 3-D volume, MRI may show the coronary tree in a way similar to the methods described for CT. Background tissue may be suppressed with fat saturation, tissue saturation, magnetization transfer, and/or T2 preparation (90°-180°-180°- ... -180°-90°). [34]
The vessel plane approach is as follows: Any desired target plane can be obtained by specifying 3 points for inclusion in the plane, by drawing lines of intersection with 2 previous images at different angles, or (commonly) by drawing a single line of intersection with a previous image that is perpendicular to the desired view. For example, to obtain a short-axis view of the coronary sinus, one must first obtain a long-axis view of the left ventricle (LV) parallel to the septum and perpendicular to the atrioventricular (AV) groove, then prescribe a plane in the AV groove perpendicular to that view, passing through the 2 observed points of intersection on the first view with the coronary sinus, seen as bright dots anterior and posterior to the mitral valve.
Other points regarding MRI for evaluation of CAD include the following:
-
A transverse stack of images covering the aortic root depicts the origin of the right coronary artery (RCA) and the left main coronary artery. Typical section thickness should be 3 mm or less. A bright- or dark-blood technique can be applied with the use of single frames or with a dynamic movie series.
-
An additional distal transverse image shows a cross-section of the right coronary artery (RCA), the left anterior descending artery (LAD), and the left circumflex artery (LCX).
-
From 2 points along the proximal vessel and from 1 point in the distal vessel, a plane that captures the desired segment is selected. The plane may be adjusted to be thick enough to encompass out-of-plane bends. As an alternative, it may be subdivided into a stack of thin imaging planes for a localized 3-D stack of images.
-
The course of the RCA in the atrioventricular (AV) groove can be ascertained quickly from a 4-chamber long-axis view of the heart by obtaining 1 preliminary image perpendicular to the AV groove and parallel to the septum through the mid right ventricle (RV). This provides 2 points of intersection with the RCA: 1 anterior and 1 posterior in the AV groove. Prescribing a plane through these 2 points from the long-axis image gives the desired view.
-
The posterior descending artery requires a different imaging plane, as do the LAD, the LCX, and major branches. The course of the LCX in the AV groove is assessed similarly to the RCA, by acquiring a scout image parallel to the septum to identify 2 points for inclusion in 1 final short-axis image. However, in this case, the scout image should be laterally displaced to the outer third because the distal LCX is often hard to identify.
-
Clinicians routinely identify the proximal course of the coronary arteries to look for aberrant origins in young patients who have had syncope. Complete absence of abnormalities suggests a good prognosis.
-
MRI with contrast is an excellent method of identifying myocardial scar (infarction) as small as 1% of the myocardium, which is a very strong prognostic factor, [35] while also assessing perfusion and precise function of left and right ventricles. It can be combined with stress testing and coronary imaging for a "1-stop shop."
-
MRI is the preferred test for right ventricular injury or infarction.
-
Apparent stenosis must be distinguished from an out-of-plane bend.
-
A signal void from flow disturbance may exaggerate apparent stenosis.
-
MRI is well established as a means to assess the patency of a bypass graft.
One study reported that infarct tissue heterogeneity identified by cardiac MRI is associated with mortality beyond that of left ventricular EF in patients who have both CAD and left ventricular dysfunction. Researchers found that this is particularly true for patients with mild or moderate left ventricular dysfunction. They have suggested that additional studies incorporating cardiac MRI in clinical decision-making for defibrillator therapy are warranted. [36]
Cardiovascular magnetic resonance (CMR) assesses cardiac function, ischemia, viability, and tissue characterization, all within a single scan. CMR has emerged as a highly accurate technique for diagnosis and risk stratification in stable CAD and has been incorporated into national and international guidelines. Furthermore, clinical pathways utilizing CMR have been shown to be the most cost-effective in several health care systems. [6]
Degree of confidence
According to one study, infarct heterogeneity identified by cardiac MRI is associated with mortality beyond left ventricular ejection fraction (LVEF) in patients with CAD and left ventricular dysfunction. Researchers have found that this is particularly true for patients with mild or moderate left ventricular dysfunction. They have suggested that additional studies incorporating cardiac MRI in clinical decision-making for defibrillator therapy are warranted.
MRI offers high sensitivity to changes in wall function (eg, wall thickening, radial motion). [18] MRI may be useful for identifying and quantifying impaired blood delivery and wall function in response to interventions. [12, 37, 38, 39, 40, 41, 42, 43] Using such applications is perhaps more vital than visualizing the percentage of stenosis.
Confidence in the data depends on speed and quality of the imaging method, cooperation of the patient (shallow regular breathing or several matching breath holds), accuracy of ECG triggering or gating, and anatomic knowledge and judgment of the person directly supervising data collection.
The usual ECG signal in MRI is markedly distorted by competing signals resulting from movement in a magnetic field and by moving magnetic fields, particularly from blood flow in the great vessels, called the magnetohydrodynamic effect. This distortion makes it difficult to perform electrographic safety monitoring for ischemic changes.
Cardiac MRI by the vessel-chasing approach requires highly informed decision-making as data are being acquired. If the operator acquiring the data understands what the coronary angiogram demonstrates, views may be manipulated for the best match. This consideration is not necessarily positive because the operator may exaggerate the agreement.
Cardiac MRI is a powerful diagnostic method, supporting robust measurements of crucial markers of cardiac structure and function, myocardial perfusion, and scar, and providing detailed insight into myocardial tissue. Accurate and informative diagnostic readouts can help with guiding therapy, monitoring disease progress, and tailoring response to treatment. [44]
The ability of MRI and CT to identify anatomy and the absence of clinically significant obstructions is improving rapidly, but it is not uniform. The value of MRI and CT must be assessed in a truly double-blind fashion until standardized and reliable methods are widely established.
Whether MRI and CT results match in terms of the percentage of stenosis is relatively unimportant. Most important is whether MRI and CT reliably depict normal tissue and culprit lesions, and whether they help in establishing disease severity and in depicting territories supplied by the culprit vessel. Both MRI and CT offer the notable advantage of enabling direct assessment of zones with impaired blood delivery.
Limitations
In an apparent stenosis, one must be certain that the finding is not a partial-volume artifact or a velocity-shear effect. Because local differences in velocity can cause a signal void, estimates of stenosis may be exaggerated.
Magnetic susceptibility artifacts may produce signal voids. Stents, clips, and wires cause local disturbances.
The presence of a pacemaker wire is considered a relative contraindication to MRI because rapidly changing magnetic fields may induce a voltage that can trigger an arrhythmia, induce a burn, or shorten battery life.
When the patient enters and leaves the magnet, the magnetic reed switch on most pacemakers will switch it to fixed mode, and the temperature in metal devices may rise. For example, a pacemaker generator may warm by 1-2°C. However, with informed consent, careful pulse monitoring, and readiness to promptly abort a pulse sequence if an arrhythmia is induced, patients with pacers have undergone MRI with no apparent consequence and no change in pacer thresholds. Of the dozen reports of mishaps related to pacemakers and MRI, none were caused by MRI.
On MRI, calcification is depicted as a black area or a signal void, whereas CT shows calcifications as white—similar to blood filled with contrast agent. These appearances can influence the estimation of stenoses. Also, with 3-D MRI or CT, one must be certain to understand how the images account for local curvature in and out of the imaging planes. In finding the best MRI plane for showing a vessel, radiologists can mistake a local curve that is out of plane for an apparent stenosis. Proper image processing can help to resolve this problem.
With MRI, flow disturbances that cause velocity shear (range of phases in each picture element or pixel resulting from different rates of motion of blood) cause a local decrease in signal intensity, which may create or exaggerate an apparent stenosis.
Ultrasonography
Echocardiography can be used to identify the left main coronary artery. In some patients, much of the right coronary artery (RCA) and the left anterior descending artery (LAD) can be viewed; however, in most patients, the imaging window is inadequate for useful coronary imaging from outside the chest.
In the catheterization laboratory, intravascular ultrasonography (IVUS) may be performed to examine coronary arteries from the inside and to characterize plaque. However, the diameter of the device limits the ability to pass through tight stenoses. Also, injection of a sonographic contrast agent (eg, agitated Renografin) into the coronary arteries, combined with transthoracic or esophageal ultrasonography, can be useful in identifying perfusion territories.
Pizzuto et al found that transthoracic Doppler echocardiography can improve the diagnostic accuracy of multidetector computed tomography (MDCT) in detecting LAD coronary artery stenosis. In 144 consecutive patients, coronary anatomy was assessed with MDCT, and echocardiography was used to calculate coronary flow reserve (CFR) by measuring the ratio of hyperemic to baseline peak flow velocity; results of both methods were verified with invasive coronary angiography. [32]
In a univariate model, prediction of significant LAD stenosis was slightly, but significantly, better with CFR (sensitivity 90%, specificity 96%, positive predictive value 84%, negative predictive value 97%, diagnostic accuracy 94%) than with MDCT (sensitivity 80%, specificity 93%, positive predictive value 71%, negative predictive value 95%, diagnostic accuracy 90%). When findings from transthoracic Doppler echocardiography and MDCT were consistent, diagnostic accuracy was increased (96%). Among 13 patients with disease missed by MDCT, transthoracic Doppler echocardiography proved 100% accurate in predicting significant LAD stenosis. [32]
Nuclear Imaging
Nuclear imaging does not depict the coronary arteries, but it does demonstrate various metabolites useful for identifying perfusion defects and tissue viability. Thallium-201 and technetium-99m sestamibi are widely used and may be combined to shorten the study of myocardial uptake of radioactive tracer at rest and during stress. [45]
Although a rest-and-stress thallium study takes longer than 4 hours, a combined study performed with thallium and sestamibi may be completed in less than 2 hours.
When positron emission tomography (PET) is used, a rest-and-stress study with rubidium-82 may be completed in 30 minutes because the agent has a half-life less than 5 minutes. A defect during stress that is not evident at rest indicates a zone of induced ischemia. A defect at rest and also during stress indicates persistent metabolic dysfunction resulting from infarction (scar) or from hibernation (prolonged dysfunction). PET with ammonia, fluorinated glucose, or other agents may be used to determine if tissue with a defect at rest is viable. [45]
Degree of confidence
Nuclear medicine tests for CAD improve predictive accuracy over stress tests alone to approximately 90%. The utility of these tests depends on the previous probability of disease, and on whether they are being used to identify CAD or to clarify the pathophysiology of known disease.
Breast attenuation may cause an apparent defect on radionuclide images. Attenuation correction and multiplanar imaging mitigate the problem.
Unusual motion, such as that from a bundle branch block or from coughing during imaging, may cause false-positive results. A persistent defect is commonly interpreted as a fixed defect or a scar, but it may represent prolonged yet still-reversible ischemic impairment of tracer uptake.
The low resolution of nuclear medicine studies compared with other modalities may result in false-negative results. Also, global disease may be missed because defects generally are identified by comparing them to regions with high uptake of the tracer.
-
Selective injection image of the left coronary arteries. D1 = first diagonal, LAD = left anterior descending artery, LCX = left circumflex, LM = left main coronary artery, and OM1= first obtuse marginal.
-
MRIs of the coronaries can be used to build 4-dimensional images (3-dimensional beating heart). These images show a single frame, including a cutaway view to show the cardiac interior, the outer surface (no thresholding), and the extracted coronary artery tree including the aortic root.
-
Elastic-match imaging automatically identifies differences between image volumes. The acquisition of 1 set of contrast-enhanced chest CT images via the coronaries and a nonenhanced set provides a 3-dimensional view of the coronary-artery tree. The nonenhanced volume data were rendered as holographic projections to provide the anatomic context, and the elastic-match coronary tree was overlaid. In addition to automation, this method avoids thresholding so that small branches and filling defects, if present, are represented properly.
-
Elastic-match imaging can be used to identify collateral-dependent myocardium. Left and middle images are baseline and peak-arrival collateral-sensitive MRIs demarcating microvascular development. Right image, based on CT imaging of the heart, was obtained with and without back pressure to nullify collateral-dependent perfusion; white volume on represents collateral-dependent myocardium. The extent of collateral-dependent myocardium corresponds well on MRI and CT (r = 0.95).
-
Contrast-labeled blood to the heart is used to identify the territory at risk. The results of this assessment of the delayed arrival compares favorably to the findings of radionuclide stress imaging, and stress induction of ischemia is not required to identify the zone at risk.
-
Space-time maps show the history of blood arrival to all layers of myocardium on a 2-dimensional map. The indentation indicates the severity of the defect in blood delivery, and the length indicates the size as a percentage of the myocardium, without the need for stress induction of ischemia. In addition to the safety advantage, this method is also more reproducible than stress testing, which is useful in assessing the effect of therapy.
-
Compared with radionuclide images of blood delivery, MRIs and CT scans improve resolution, depiction of the functional effect and the relationship to the coronary supply, and identification of the area at risk without stress. The advantage of radionuclide imaging is primarily its predictive value; stress echocardiography has similar predictive value. MRI and CT have been less available than other studies; therefore, data on their value are relatively limited.
-
X-ray angiography is the criterion standard for delineating the coronary anatomy, but it is inferior to MRI and CT in identifying myocardium with impaired blood delivery, in assessing the functional consequences, and in identifying the development of microvascular collaterals.

