Practice Essentials
First described by Cooper and Travers in 1818, giant cell tumors (GCTs) of bone have been labeled the most challenging benign bone tumors. Although benign, GCTs show a tendency for significant bone destruction, local recurrence, and occasionally metastasis. The natural history of GCTs varies widely and can range from local bony destruction to local metastasis, metastasis to the lung, metastasis to lymph nodes (rare), or malignant transformation (rare). [1]
A low percentage (1-9%) of GCTs of bone metastasize to the lung. [2] The metastases appear as clusters of GCTs located within the lung. GCT metastases generally appear an average of 3-5 years after the initial diagnosis of the primary lesion; however, in some cases, they may go undetected for 10 years or longer. [3] The natural history of these lung metastases is unpredictable. Pulmonary metastases that spontaneously regress, remain stable, continuously grow slowly, or rapidly progress have been reported.
Pain is the most common presenting symptom. Swelling and deformity are associated with larger lesions. Soft-tissue extension is common. The incidence of pathologic fracture at presentation is 11-37%.
The presence of tumor is the indication for surgery. Radiation therapy (RT) and embolization generally are reserved for cases in which surgical treatment is not feasible.
Epidemiology
In the United States and Europe, GCTs represent approximately 5% of all primary bone tumors and 21% of all benign bone tumors. [1] In China, GCTs have been estimated to account for 20% of all primary bone tumors. [4] An epidemiologic comparison study between 9200 patients treated at Beijing Ji Shui Tan Hospital and 10,165 patients treated at the Mayo Clinic found that the incidence of GCT was significantly higher among the former. [5]
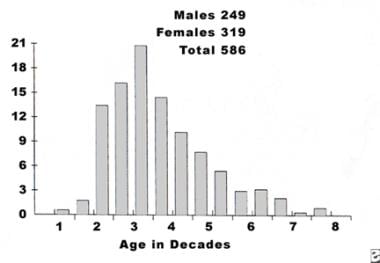
A female predominance exists, with a female-to-male ratio of 1.3-1.5:1 (see the image below). [1] GCTs occur most commonly in the third decade of life; fewer than 5% of GCTs occur in patients who are skeletally immature. [1, 6] In the Mayo Clinic series, 84% of the GCTs occurred in patients older than 19 years. [1]
Prognosis
The overall prognosis generally is good. However, pulmonary metastases have been cited as the cause of death in 16-25% of reported cases. [7, 8, 9]
In a study comparing the outcomes of two surgical treatments—curettage (n = 14) and segmental resection (n = 13)—in patients with GCTs of the proximal humerus who were followed for more than 2 years, Bai et al found that the recurrence rate was 7.1% in the curettage group and 15.4% in the segmental resection group. [10] Postoperative upper-extremity function was significantly better in the curettage group than in the segmental resection group.
-
Approximately 50% of giant cell tumors are located around knee. Most common locations are distal femur, proximal tibia, and proximal humerus and distal radius.
-
Distribution of giant cell tumors according to age and sex of patient. Six patients had multicentric disease.
-
Giant cell tumor. Anteroposterior radiograph of distal femur reveals expansile lytic metaphyseal-epiphyseal lesion.
-
Giant cell tumor. Lateral radiograph of same distal femur as in previous image reveals expansile lytic metaphyseal-epiphyseal lesion.
-
Giant cell tumor. Anteroposterior radiograph of distal radius reveals aggressive lesion characterized by extensive local bony destruction, cortical breakthrough, and significant soft-tissue expansion.
-
Giant cell tumor. Lateral radiograph of same distal radius as in previous image reveals aggressive lesion characterized by extensive local bony destruction, cortical breakthrough, and significant soft-tissue expansion.
-
Giant cell tumor. Sagittal MRI of same distal radius as in previous two images reveals aggressive lesion characterized by extensive local bony destruction, cortical breakthrough, and significant soft-tissue expansion.
-
Giant cell tumor. Anteroposterior radiograph of distal tibia demonstrates extension of lesion to articular surface.
-
Giant cell tumor. Lateral radiograph of same distal tibia as in preceding image demonstrates extension of lesion to articular surface.
-
Giant cell tumor. Sagittal MRI of same distal tibia as in previous two images demonstrates extension of lesion to articular surface.
-
Anteroposterior radiograph of wrist arthrodesis performed for giant cell tumor. Soft-tissue recurrence is present. Note peripheral mineralization about soft-tissue recurrence (arrow).
-
Sagittal T1-weighted MRI shows giant cell tumor with low signal intensity.
-
Sagittal T2-weighted MRI shows giant cell tumor with intermediate-to-high signal intensity.
-
Giant cell tumor. CT scan of distal femur reveals absence of matrix within lesion.
-
Intraoperative photograph of giant cell tumor in distal femur.
-
Gross specimen of same giant cell tumor in the distal femur as in preceding image displays typical chocolate-brown and spongy appearance.
-
Bisected gross specimen of giant cell tumor in preceding image reveals blood-filled cystic areas and inner yellow and orange discoloration.
-
Gross specimen of giant cell tumor that fills entire distal radius. Despite cortical disruption, periosteum remains intact (arrow). Once again, note blood-filled cystic areas and areas of orange discoloration.
-
Photomicrograph of giant cell tumor reveals typical appearance. Multinucleated giant cells are dispersed throughout on background of mononuclear cells.
-
Photomicrograph of giant cell tumor reveals typical appearance. Multinucleated giant cells are dispersed throughout on background of mononuclear cells.
-
Photomicrograph of giant cell tumor reveals prominent mitotic activity and rare cellular atypia.
-
Photomicrograph of giant cell tumor reveals prominent mitotic activity and rare cellular atypia.
-
Giant cell tumor. Photomicrograph of multinucleated giant cell. Note centrally located nuclei.
-
Giant cell tumor. Photomicrograph of multinucleated giant cell. Note centrally located nuclei.
-
Giant cell tumor. Photomicrograph of multinucleated giant cell. Note centrally located nuclei.
-
Photomicrograph of giant cell tumor with few multinucleated giant cells but abundant swirls of spindle-shaped stromal cells.
-
Photomicrograph of giant cell tumor with few multinucleated giant cells but abundant swirls of spindle-shaped stromal cells.
-
Photomicrograph of giant cell tumor with intravascular invasion of multinucleated giant cells.
-
Anteroposterior radiograph of giant cell tumor of distal radius.
-
Intraoperative photograph of resection bed of same giant cell tumor of distal radius as in preceding image after distal radius is resected.
-
Intraoperative photograph of same giant cell tumor of distal radius as in previous two images shows wrist arthrodesis with fibular autograft and 16-hole low-contact dynamic compression (LCDC) plate.
-
Postoperative lateral radiograph of same giant cell tumor of distal radius as in preceding image.
-
Giant cell tumor. Intraoperative photograph of distal tibia reveals curetted and burred cavity.
-
Giant cell tumor. Intraoperative photograph of same distal tibia as in preceding image reveals polymethylmethacrylate packed into distal tibial cavity.
-
Giant cell tumor. Anteroposterior radiograph of distal tibia with polymethylmethacrylate packed in distal femur after curettage of lesion.
-
Giant cell tumor. Illustration of large cavity necessary for sufficient curettage.
-
Giant cell tumor. Illustration of direct pour technique.
-
Intraoperative photograph of distal femur with polymethylmethacrylate and Steinman pins inserted into cavity after removal of giant cell tumor.
-
Lateral radiograph of same distal femur as in preceding image with polymethylmethacrylate and Steinman pins inserted into cavity after removal of giant cell tumor.
-
Intraoperative photograph of distal femur after removal of giant cell tumor. Cavity has been curetted and treated with high-speed burr.
-
Giant cell tumor. Intraoperative photograph of distal femoral cavity of same distal femur as in preceding image, obtained while cavity is undergoing argon laser treatment.
-
Giant cell tumor. Intraoperative photograph of distal femoral cavity of same distal femur as in preceding image, obtained after argon laser treatment is complete.