Practice Essentials
Pulmonary hamartoma (PH) is the most common benign tumor of the lung and is the third most common cause of solitary pulmonary nodules. [1, 2] PHs occur mostly as peripheral solitary nodules and are incidentally detected on routine radiologic examinations, such as radiography and computed tomography (CT). Endobronchial hamartomas occur much less frequently and represent 1.4–10% of PHs. [3]
Symptoms of hamartoma depend on the location of the tumor. Patients can be asymptomatic with peripheral parenchymal hamartomas, with incidental discovery on chest imaging obtained for another reason. If located endobronchially, they can cause irritation of bronchial mucosa resulting in persistent cough as a presenting symptom. Endobronchial hamartomas can be associated with obstruction of the bronchus with symptoms of fever, cough, expectoration, wheezing, and dyspnea. Complications such as postobstructive pneumonia and lobar atelectasis may occur. Hemoptysis can occur if it impinges on vascular structures and causes invasion or perforation. [3]
PH usually presents with a round shape and smooth margins. The main CT features are intranodular fat and popcorn-like calcifications. [4]
(Evidence of a pulmonary hamartoma is seen in the image below.)
 Posteroanterior (PA) chest radiograph in a man shows an incidental coin lesion in the right midzone with characteristic popcorn calcification.
Posteroanterior (PA) chest radiograph in a man shows an incidental coin lesion in the right midzone with characteristic popcorn calcification.
Accounting for 75% of all benign lung tumors [4] hamartomas are composed of tissues that are normally present in the lung, including fat, epithelial tissue, fibrous tissue, and cartilage.
Radiography
Pulmonary hamartomas are usually asymptomatic and are typically discovered as an incidental coin lesion on a routine chest radiograph. On chest radiographs, pulmonary hamartomas characteristically appear as well-defined, solitary pulmonary nodules; they may show varying patterns of calcification, including an irregular popcorn, stippled, or curvilinear pattern, or even a combination of all 3 patterns. When calcification or fat is detected in a well-circumscribed peripheral lung tumor, a diagnosis of hamartoma can confidently be made. However, the characteristic calcification is seen in only approximately 15% of patients, and detection of fat within a nodule is even rarer on plain radiographs. Popcorn calcification is virtually diagnostic.
When a central lucency occurs in a hamartoma because of the presence of adipose tissue, the lucency may be misinterpreted as air within a cavity, resulting in a significantly different differential diagnosis. When no characteristic calcification or fat is identified in a coin lesion or when multiple lesions are present, the differential diagnosis is extensive.
(Posteroanterior radiographic evidence of lung hamartomas is demonstrated in the images below.)
 Posteroanterior (PA) chest radiograph in a man shows an incidental coin lesion in the right midzone with characteristic popcorn calcification.
Posteroanterior (PA) chest radiograph in a man shows an incidental coin lesion in the right midzone with characteristic popcorn calcification.
 Posteroanterior (PA) chest radiograph shows an incidental finding of a solitary pulmonary nodule adjacent to the left hilum.
Posteroanterior (PA) chest radiograph shows an incidental finding of a solitary pulmonary nodule adjacent to the left hilum.
Most lesions are smaller than 4 cm in diameter and well circumscribed; they are usually lobulated. The lesions show no lobar predominance, and cavitation is extremely rare. In unusual cases, bronchial obstruction occurs with a central tumor, causing obstructive pneumonitis, bronchiectasis, and progressive peripheral lung destruction.
Serial chest radiographs may demonstrate slow growth. Rapid growth has rarely been reported. This feature may make the differentiation of a hamartoma from a bronchogenic carcinoma difficult.
Computed Tomography
CT is the diagnostic tool of choice in the study of the internal characteristics of pulmonary nodules. CT scanning is more sensitive than chest radiography in the detection of fat and calcification. The main CT features suggestive of PH are intranodular fat and popcorn-like calcifications. [16] The Hounsfield values for fat lie within the range of -50 to -120 HU. Fat is identified in 34-50% of lesions, and calcification is identified in 15-30%. [4] Hamartoma may be confidently diagnosed when a sharply marginated, smooth lesion containing calcification and fat is identified on a CT scan. In one third of hamartomas, no calcium or fat is demonstrable on CT scans. The differential diagnosis is extensive in these cases. Central endobronchial tumors may have features that are indistinguishable from those of a bronchial carcinoid.
(CT scans of lung hamartoma are depicted in the images below.)
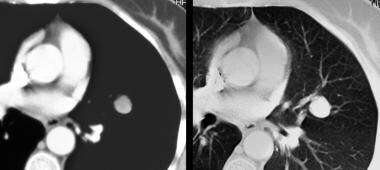 Computed tomography (CT) scans obtained with soft-tissue and lung window settings confirm the presence of a well-defined nodule in the lingula, with a mean Hounsfield value of 26 HU; this finding was unhelpful. Findings from percutaneous, fluoroscopy–guided biopsy confirmed the diagnosis of pulmonary hamartoma.
Computed tomography (CT) scans obtained with soft-tissue and lung window settings confirm the presence of a well-defined nodule in the lingula, with a mean Hounsfield value of 26 HU; this finding was unhelpful. Findings from percutaneous, fluoroscopy–guided biopsy confirmed the diagnosis of pulmonary hamartoma.
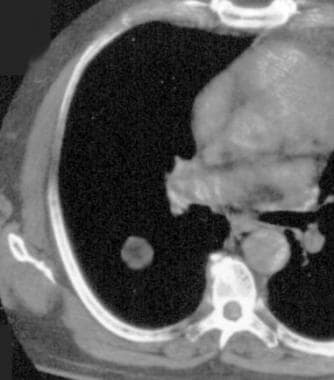 Nonenhanced, axial computed tomography (CT) scan through the midthorax shows a sharply marginated, smooth, fat-containing lesion in the right lung. CT scanning is more sensitive than chest radiography in the depiction of fat and calcification. Using CT scanning, hamartomas may be confidently diagnosed when a sharply marginated, smooth lesion containing calcification and fat is identified.
Nonenhanced, axial computed tomography (CT) scan through the midthorax shows a sharply marginated, smooth, fat-containing lesion in the right lung. CT scanning is more sensitive than chest radiography in the depiction of fat and calcification. Using CT scanning, hamartomas may be confidently diagnosed when a sharply marginated, smooth lesion containing calcification and fat is identified.
 Axial computed tomography (CT) scan just above the carina showing a giant lung hamartoma. Note the characteristic popcorn calcification.
Axial computed tomography (CT) scan just above the carina showing a giant lung hamartoma. Note the characteristic popcorn calcification.
On high-resolution CT (HRCT) scans, fat attenuation is detectable in 34% of tumors, and fat and calcium is detected in 19%. The finding of fat and calcification together is a specific combination for hamartomas, particularly in tumors less than 2.5 cm in diameter. The frequency of calcification increases with increasing tumor size; calcification is found in only 10% of lesions smaller than 2 cm, but this rate reaches 75% for lesions larger than 5 cm.
After retrospectively reviewing multidetector CT results from 55 patients with histologically confirmed pulmonary hamartoma, Hochhegger et al concluded that the adoption of a new threshold for fat content (< -33 HU) could lead to improvement in the overall detection of pulmonary hamartomas by multidetector CT. In the study, pulmonary hamartomas manifested predominantly as peripheral pulmonary nodules with lobulated margins. The accuracy, sensitivity, and specificity of fat detection at a density threshold of -40 HU were 83.7%, 100%, and 87.2%, respectively. At a threshold of -33 HU, better results (95.3%, 100%, and 96.3%, respectively) were realized. Popcorn-like calcifications were found in only 12/55 (21.8%) pulmonary hamartomas and were the only imaging feature in 7.2% of cases. Most (66%) lesions with popcorn-like calcifications also contained fat. [16]
Nuclear Imaging
A paraganglioma that is associated with the Carney triad may be identified with iodine-123 or iodine-131 MIBG scanning. Radionuclide studies have no role in the diagnosis of a lung hamartoma. MIBG uptake may occur in other neuroendocrine tumors.
Functional imaging with FDG-PET can distinguish between benign and malignant nodules because of the increased metabolic activity typically found in cancers. A standardized uptake value greater than 2.5 is used to identify nodules that have a high probability of malignancy. FDG-PET is most cost-effective when the clinical pretest probability of malignancy and the results of the CT are discordant (eg, low pretest probability with chest CT characteristics that are clearly not benign). The ACCP guidelines recommend FDG-PET in persons with solid indeterminate nodules 8 mm or greater in diameter and a low to intermediate pretest probability of malignancy. [21]
-
Posteroanterior (PA) chest radiograph in a man shows an incidental coin lesion in the right midzone with characteristic popcorn calcification.
-
Posteroanterior (PA) chest radiograph shows an incidental finding of a solitary pulmonary nodule adjacent to the left hilum.
-
Computed tomography (CT) scans obtained with soft-tissue and lung window settings confirm the presence of a well-defined nodule in the lingula, with a mean Hounsfield value of 26 HU; this finding was unhelpful. Findings from percutaneous, fluoroscopy–guided biopsy confirmed the diagnosis of pulmonary hamartoma.
-
Nonenhanced, axial computed tomography (CT) scan through the midthorax shows a sharply marginated, smooth, fat-containing lesion in the right lung. CT scanning is more sensitive than chest radiography in the depiction of fat and calcification. Using CT scanning, hamartomas may be confidently diagnosed when a sharply marginated, smooth lesion containing calcification and fat is identified.
-
Axial computed tomography (CT) scan just above the carina showing a giant lung hamartoma. Note the characteristic popcorn calcification.


